Abstract
Donor human milk is recommended by the American Academy of Pediatrics for high-risk infants when mother’s own milk is absent or insufficient in quantity. Several factors may contribute to the inequitable use of or access to donor human milk, including a limited knowledge of its effects, cost, reimbursement, and regulatory barriers. The American Academy of Pediatrics and the United States Surgeon General have called for investigating barriers that prevent use of donor human milk for high-risk infants and for changes to public policy known to improve availability and affordability. We review the current legislative, regulatory, and economic landscape surrounding donor human milk use in the United States, as well as suggest state- and federal-level solutions to increase access to donor human milk.
Similar content being viewed by others
Introduction
Human milk is the ideal diet for infants and is associated with beneficial health outcomes [1,2,3]. These benefits are especially potent for very premature (<32 weeks gestation) and very low birth weight (VLBW) infants (birth weight <1500 g) [4]. A clear protective effect against necrotizing enterocolitis (NEC), a devastating disease that affects the intestines of premature and other high-risk infants, has been demonstrated in multiple studies, such that if maternal milk is absent or insufficient in quantity, the use of donor human milk (DHM) is recommended [2, 4,5,6,7,8]. The American Academy of Pediatrics (AAP) recommends that DHM be used in high-risk infants when mother’s milk is insufficient in quantity, and that DHM be available based on medical necessity, not financial status [7]. The recommendation for pasteurized DHM when mother’s own milk is not available, is insufficient in quantity, or is contraindicated, was also noted in an AAP Clinical Report focused on human milk for VLBW infants [9].
What is donor human milk and who needs it?
DHM is human milk that has been donated by healthy lactating individuals, then processed and distributed in accordance with established evidence-based guidelines [7, 10]. The first donor milk organization in North America was established in 1910 as the Boston Wet Nurses Directory, which then became a donor milk bank in 1919 [11]. DHM has been used in premature and ill infants for over 100 years when mother’s milk has been insufficient in quantity or unavailable. Human milk contains bioactive factors such as immunoglobulins, human milk oligosaccharides, lysozyme, lactoferrin and other factors that are important to immune and intestinal development and protect against inflammatory disorders, such as NEC [6, 12].
Meta-analysis of randomized controlled trials supports the use of DHM instead of formula in preterm infants. A 2019 Cochrane review found that feeding premature or low birthweight infants formula rather than DHM is associated with a near-doubled NEC risk (Risk Ratio 1.87, 95% CI 1.23–2.85, 9 studies, 1675 infants) [8]. A contemporary large blinded randomized controlled trial from Canada found a reduction in the rate of NEC from 6.6% to 1.7% when comparing preterm formula to DHM fortified with powdered bovine-based fortifier [13].
Outside of prematurity status, other neonatal conditions such as gastrointestinal anomalies and congenital heart disease may place an infant at high risk for feeding complications, including NEC. Evidence to support the use of DHM in these high-risk populations is limited to observational studies [14,15,16,17]. While DHM use is typically restricted to very premature and VLBW infants on the basis of the available evidence showing benefit in this population and cost-effectiveness, individual hospital policy typically determines which infants may receive DHM, and criteria vary widely [18]. Local patterns of use also help determine the cost-effectiveness of DHM use, which is dependent on several factors, including the rate mothers provide their own milk, cost and source of DHM, number of eligible infants, and duration of use. DHM use in VLBW infants may be cost-saving or cost-neutral from the decreased incidence of NEC and shorter hospital stay, which offset the initial investment [19,20,21,22,23]. In addition, those savings may extend beyond hospital discharge; an economic analysis of a randomized controlled trial of comparing health outcomes on VLBW infants fed DHM versus preterm formula demonstrated infants who were fed DHM had decreased post-discharge costs, likely related to lower parental lost wages [23].
Barriers to donor human milk access and use
Although extensive evidence supports the use of DHM in VLBW infants, availability of DHM is a healthcare disparity. DHM use varies by level of care, ranging from 18% of level 1 nurseries to 66% of level 3 and 74% of level 4 units which typically care for post-surgical neonates [20, 24,25,26,27]. Safety-net hospitals (≥75% Medicaid) and hospitals with a high proportion of Black or Hispanic patients are less likely to use DHM compared to non-safety-net hospitals [24, 26, 28]. These differences are not fully explained by lack of supply or geography, as the Human Milk Banking Association of North America (HMBANA), which accredits nonprofit milk banks in the United States and Canada, has 31 active milk bank members and four more in development. The capacity to dispense DHM continues to increase annually, and DHM is routinely shipped overnight to and from milk banks regionally and nationally [29].
Both the AAP and the Surgeon General have called for investigation into the barriers that prevent the use of DHM and for changes to policy to improve availability and affordability [7, 30]. We review the current legislative, economic, and regulatory landscape surrounding DHM use in the US, describe how limitations of current policies create barriers to care, and suggest solutions to improve access to DHM for vulnerable infants. Understanding current state policies and regulations can assist advocates in leveraging policy tools to facilitate access to DHM for infants who could most benefit.
Review of state legislative and regulatory policies for donor human milk
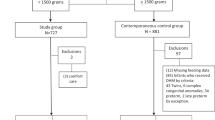
After using the commercial legal database, Westlaw, as well as state-government websites to identify enacted statutes and regulations that included direct reference to DHM, we evaluated the results regarding DHM provision and insurance reimbursement (search strategy available in Supplementary Table 1). We compared approaches of all states identified with regards to their DHM coverage policies including public versus commercial insurance reimbursement, varying definitions of medical necessity, patient age limits, and inpatient versus outpatient benefit.
At the time of this manuscript submission, 14 states and the District of Columbia have enacted DHM legislation or regulations addressing Medicaid or commercial insurance coverage (Table 1). California was the first to approve Medicaid reimbursement for DHM in 1998. Since then, advocates have worked to increase DHM access [10, 31]. Over half of the existing state-level policies have been enacted since the 2017 publication of the AAP Policy on DHM [7]. Nine states pursued legislative mandates, while five and the District of Columbia created coverage through state regulatory measures. Since 2020, seven additional states have introduced legislation for DHM coverage, including Georgia, Maine, Massachusetts, Nevada, Oklahoma, South Carolina, and Virginia. Although it is unlikely that all of these efforts will result in enacted legislation, they represent important ongoing state level advocacy.
The DHM legislation or regulations vary widely. Age limits for coverage are different between states, with Missouri and Kansas the most restrictive, covering DHM until 3 months of age, and Texas allowing for outpatient DHM up to 20 years, although this is an extreme exception. The availability of mother’s own milk is another variable, with New Jersey allowing for an infant up to 6 months of age to receive DHM if mother’s own milk is generally insufficient in quantity or unavailable, while the District of Columbia lists reasons a mother is unable to provide milk, including due to illness, death, surgery, chronic condition, drug, or medication use. Missouri does not explicitly require unavailability or inadequate supply of mother’s own milk and New York also includes language that the mother had optimal lactation support. Medical necessity is defined variably. Some states, such as Connecticut, include a requirement of “medical necessity,” relying on a broader definition of medical necessity that applies to all Medicaid treatment, for example. Others, such as Illinois, list specific medical conditions to be considered in the context of ordering DHM for a VLBW infant.
State law insurance reimbursement requirements are limited to Medicaid in many states; in New York, Medicaid coverage was mandated in 2017 and then subsequent statutes passed in 2018 required coverage by all insurance providers. Regulations in Illinois, Kentucky, and New Jersey also include commercial insurance coverage requirements. Kentucky is unique in that it requires coverage for human milk-based fortifier as part of an exclusive human milk diet for commercial plans but includes no Medicaid requirements [32]. South Carolina does not have a statewide policy, however Select Health, one of the state’s managed Medicaid plans, began covering DHM in 2016 [33]. It is possible that other states have similar unique situations where individual plans have implemented a DHM benefit without broader coverage by Medicaid.
Coverage for DHM within Medicaid programs is uniquely suited to improve access for premature and other high-risk infants. Medicaid covers approximately 40% of all US births and 50% of all early preterm births [34]. It also covers a disproportionate share (59–65%) of Hispanic and Black infants, who are more likely to be born in safety-net hospitals and who may be more likely to develop NEC associated with reduced human milk use [35, 36].
Figure 1 shows the percentage of VLBW infants born in states with any form of DHM policy from 2009–2019. In 2009, 6144 (11%) VLBW infants were born in a state with a DHM policy. In 2019, that number increased to 20,145 (43%). However, these numbers may be an overrepresentation of covered infants based on the policy differences discussed above and in Table 1. Over half of VLBW infants are born in the 35 states without DHM coverage, and thus some of these infants may lack access to this intervention. Interestingly, if all DHM bills proposed in state legislatures in 2020 and 2021 become law, an additional estimated 4300 VLBW infants would have potential access to DHM, representing, in addition to those already covered, an estimated 53% of all VLBW infants in the US.
Percent of VLBW infants born each year in a state with any form of donor human milk policy (inpatient coverage, outpatient coverage, or both) was calculated using CDC Wonder Natality database from 2007 to 2019 [52]. The numerator for each year is the number of live born infants with BW < 1500 g in a state with a DHM policy. The denominator is the total number of infants born in the US with birth weight <1500 g for the given year. VLBW from Louisiana and Illinois are not included as CDC Wonder Natality is current through 2019, and coverage was not required until 2020.
Federal law and policy
There is federal precedent to support breastfeeding and the use of human milk even prior to the Patient Protection and Affordable Care Act (ACA) [37]. However, the ACA substantially strengthened breastfeeding policies, requiring insurance plans to provide breastfeeding support, counseling, and equipment [38]. As well, the ACA requires dedicated space for breastfeeding and mandatory break time for pumping for hourly-wage working mothers, impacting upwards of 19 million women [39, 40]. However, few federal policies explicitly address the provision of DHM.
The Special Supplemental Nutrition Program for Women Infants and Children (WIC) is a federal program for which eligibility is determined by the federal government based on participant category (pregnant, postpartum, breastfeeding, infant or child up to age 5), income and nutritional risk [41]. WIC program regulations require local WIC agencies to create policies to support breastfeeding, especially for women who are most likely to need assistance [42]. Prior to 2000, WIC allowed the use of DHM on a case by case basis; however in 2000 the agency prohibited DHM as an allowable substitute for WIC-eligible formulas citing the lack of federal health and safety standards for milk banking operations, lack of mandatory pathogen, drug and toxin screening, and the alteration to the nutritive value of human milk by the pasteurization process as the key drivers for its policy change [43]. Current medical evidence, including safety shown in multiple clinical trials, have mitigated these concerns for DHM use in VLBW or preterm infants. In addition, a 2011 Food and Drug Administration public advisory committee meeting stated that the “processing adopted by the Human Milk Banking Association of North America and Prolacta, a commercial vendor of human milk products, appears to control the [infectious disease] risks adequately” [44].
TriCare, the federal health care program for uniformed service members, retirees, and their families around the world, however, takes a different approach. Tricare changed its coverage to cover the use of DHM up to 12 months of age starting in 2019 [45]. However, plans within Tricare implement this benefit in a variety of ways, with some members required to cover initial expenses out-of-pocket prior to reimbursement, placing a potentially large financial burden on families that may prohibit access.
Steps to advance access to donor human milk
We believe there are four critical steps necessary to improve access to DHM.
Engaging key stakeholders
Key stakeholders, including families of high-risk infants, patients impacted by diseases such as NEC, healthcare professionals, and policy makers, must be engaged and educated on the benefits of DHM. Lactation education for healthcare professionals should include the evidence base for DHM and the production pipeline and accessibility of DHM so they can communicate clearly with patient families regarding risks and benefits to better inform consent. Families should have access to education about DHM, as well as information on how to donate milk for those who are able. Potential donors can visit the HMBANA website (www.hmbana.org) for guidance about the screening process, including health questionnaires, medical clearance, and blood testing.
Policy changes
Policies at the hospital, state and federal level can support the use of DHM in appropriate high-risk infants. Hospitals that provide infants in the neonatal intensive care unit access to DHM have seen associated increases in mother’s milk use as this may enhance the recognized value of human milk to infant health [20, 46, 47]. Advocacy efforts from the child health community can draw on successes from states with current DHM policies to overcome the lack of awareness of the benefits of DHM among policy makers as well as hesitancy about increased short-term spending from fiscally wary administrators and legislatures.
Medically necessary DHM should be covered and reimbursed by state Medicaid plans and commercial insurance. DHM, as a benefit, should seamlessly be covered for inpatient as well as outpatient use in certain high-risk conditions. Many infants with conditions such as gastroschisis, intestinal failure, or severe congenital heart disease have complex nutritional needs after discharge from a neonatal unit, and their access to DHM should continue at home, if deemed appropriate for their nutritional needs by their treating clinicians. DHM advocates can work collaboratively on the state level, either through the legislative process or directly with state health agencies, to advance policies that support DHM as an explicit part of policies that promote breastfeeding and lactation, as they are all inextricably linked.
The most inclusive approach would involve federal legislation requiring that DHM be a fully covered benefit by all insurance policies. Important beyond DHM coverage are additional federal policies that support breastfeeding such as those implemented in the ACA. Mothers establishing lactation for VLBW infants, who are unable to directly breastfeed, must have access to NICU-specific lactation expertise as well as high-quality, hospital grade breast-pumps. The AAP recommends effective and efficient double electric breast pumps for mothers of VLBW infants to maximize and maintain milk expression at the hospital and at home [9]. Policies that more broadly support families, including paid family leave, ensuring a livable wage through universal basic income or raising the minimum wage, and housing and educational support would also help mediate the economic burden associated with the provision of mother’s own milk [39, 48]. Similarly, since previously cited concerns regarding the safety of DHM have been adequately addressed, including DHM as a WIC-eligible specialty nutritional product, when medically indicated, would increase access for low-income families, further reducing disparities in DHM availability. While the potential for expanding the use of DHM must be balanced with the supply of DHM, HMBANA now has 31 participating milk banks and reported record-breaking donation volumes in 2020 despite the COVID-19 pandemic [29].
Just as important as advocating for policies that improve health, is ensuring that those policies are implemented, and practices adjusted. Additionally, policies that lack appropriate funding will be ineffective. Funds should be appropriated as part of the original legislative or regulatory mandate. Policy implementation should be simple and streamlined to reduce barriers for hospitals and make verification of use and payment easy for Medicaid agencies. Further, implementation efforts of state policies should include a periodic reassessment by Medicaid agencies to determine the potential cost-savings of DHM and consider revision of the indications for use and payment based on established medical evidence. State and local chapters of organizations such as the AAP have government relations committees and other structures in place that may be able to assist local advocates’ efforts.
Funding for research and milk banks
Funding to support human milk research and milk bank creation and maintenance is needed. Research funding may support the study of human milk, including approaches to maximally preserve beneficial nutrients and bioactive factors in DHM after processing, and evaluate the evidence for DHM use in high-risk infant populations outside of those born prematurely. Funding could also support the creation and maintenance of new non-profit milk banks. Recent legislation passed in Arkansas created a state-funded milk bank, an action that will directly benefit infants in that state [49]. The infant mortality rate in Arkansas is higher than most other states in the country, and creation of a state milk bank may increase access to DHM availability for hospitalized infants in Arkansas.
Advocacy
Finally, DHM advocacy efforts are critically important and require institutional and financial support. Evidenced-based medicine should be central in the creation of health and social policy, and child advocates need support in their efforts to advocate and educate for improved health outcomes [50]. Advocacy and policy education can be incorporated into medical training programs to give future physicians the tools necessary to effectively influence child health policy [51]. DHM advocates can network with colleagues in states with successful DHM regulations to adapt advocacy approaches and enact change in their own state. From initial discussions through the final passage of a bill or policy, the legislative process can take years. Importantly, effective implementation of adopted policy will also need additional advocacy efforts. Philanthropic funding and grant support can sustain policy research, development, and implementation and allow volunteer advocates to build networks and enact change.
While it may seem challenging to begin advocating, but many others have gone through the process. In the authors’ experience, we have found it very helpful to connect with other states and groups to discuss strategies and tools for advocacy. For those interested in new advocacy efforts, you might reach out to the corresponding author for more information.
Conclusion
The majority of high-risk infants who need access to DHM are not born in a state or district where that access is guaranteed; no state currently covers the cost of DHM whether inpatient, outpatient, or for all infants who may benefit from its use. State and federal level advocacy is needed to ensure that DHM is available to all infants based on medical necessity, rather than privileging infants who happen to be born in a state or district where access is guaranteed. High-risk infants would particularly benefit from legislative and regulatory changes that would increase patient access to and affordability of DHM, including mandated coverage.
References
Ip S, Chung M, Raman G, Chew P, Magula N, DeVine D, et al. Breastfeeding and maternal and infant health outcomes in developed countries. Evid Rep Technol Assess Full Rep. 2007;153:1–186.
Section on B. Breastfeeding and the use of human milk. Pediatrics. 2012;129:e827–841.
Chetta KE, Schulz EV, Wagner CL. Outcomes improved with human milk intake in preterm and full-term infants. Semin Perinatol. 2021;45:151384.
Miller J, Tonkin E, Damarell RA, McPhee AJ, Suganuma M, Suganuma H, et al. A systematic review and meta-analysis of human milk feeding and morbidity in very low birth weight infants. Nutrients 2018;10:707.
Organization WH. Optimal feeding of low birth-weight infants in low-and middle-income countries. 2011. https://www.who.int/elena/titles/donormilk_infants/en/.
Nutrition ECo, Arslanoglu S, Corpeleijn W, Moro G, Braegger C, Campoy C, et al. Donor human milk for preterm infants: current evidence and research directions. J Pediatr Gastroenterol Nutr. 2013;57:535–42.
Committee on Nutrition, Section on Breastfeeding, Committee on Fetus and Newborn. Donor human milk for the high-risk infant: preparation, safety, and usage options in the United States. Pediatrics. 2017;139:e20163440.
Quigley M, Embleton ND, McGuire W. Formula versus donor breast milk for feeding preterm or low birth weight infants. Cochrane Database Syst Rev. 2019;7:CD002971.
Parker MG, Stellwagen LM, Noble L, Kim JH, Poindexter BB, Puopolo KM, et al. Promoting human milk and breastfeeding for the very low birth weight infant. Pediatrics. 2021;148:e2021054272.
Schmaltz CH, Bouchet-Horwitz J, Summers L. Advocating for pasteurized donor human milk: the journey for medicaid reimbursement in New York State. Adv Neonatal Care. 2019;19:431–40.
Jones F, Human Milk Banking Association of North A. History of North American donor milk banking: one hundred years of progress. J Hum Lact. 2003;19:313–8.
Nolan LS, Parks OB, Good M. A review of the immunomodulating components of maternal breast milk and protection against necrotizing enterocolitis. Nutrients. 2019;12:14.
O’Connor DL, Gibbins S, Kiss A, Bando N, Brennan-Donnan J, Ng E, et al. Effect of supplemental donor human milk compared with preterm formula on neurodevelopment of very low-birth-weight infants at 18 months: a randomized clinical trial. JAMA. 2016;316:1897–905.
Cognata A, Kataria-Hale J, Griffiths P, Maskatia S, Rios D, O’Donnell A, et al. Human milk use in the preoperative period is associated with a lower risk for necrotizing enterocolitis in neonates with complex congenital heart disease. J Pediatr. 2019;215:11–16 e12.
Hoban R, Khatri S, Patel A, Unger SL. Supplementation of mother’s own milk with donor milk in infants with gastroschisis or intestinal atresia: a retrospective study. Nutrients. 2020;12:589.
McKittrick MM, Khaki S, Gievers L, Larson IA. Clinical and sociodemographic factors associated with human donor milk supplementation in term newborns. Hosp Pediatr. 2020;10:489–95.
McCune S, Perrin MT. Donor human milk use in populations other than the preterm infant: a systematic scoping review. Breastfeed Med. 2021;16:8–20.
Hagadorn JI, Brownell EA, Lussier MM, Parker MG, Herson VC. Variability of criteria for pasteurized donor human milk use: a survey of U.S. neonatal intensive care unit medical directors. JPEN J Parenter Enter Nutr. 2016;40:326–33.
Stey A, Barnert ES, Tseng CH, Keeler E, Needleman J, Leng M, et al. Outcomes and costs of surgical treatments of necrotizing enterocolitis. Pediatrics. 2015;135:e1190–1197.
Kantorowska A, Wei JC, Cohen RS, Lawrence RA, Gould JB, Lee HC. Impact of donor milk availability on breast milk use and necrotizing enterocolitis rates. Pediatrics. 2016;137:e20153123.
Johnson TJ, Patel AL, Bigger HR, Engstrom JL, Meier PP. Cost savings of human milk as a strategy to reduce the incidence of necrotizing enterocolitis in very low birth weight infants. Neonatology. 2015;107:271–6.
Johnson TJ, Berenz A, Wicks J, Esquerra-Zwiers A, Sulo KS, Gross ME, et al. The economic impact of donor milk in the neonatal intensive care unit. J Pediatr. 2020;224:57–65 e54.
Trang S, Zupancic JAF, Unger S, Kiss A, Bando N, Wong S, et al. Cost-effectiveness of supplemental donor milk versus formula for very low birth weight infants. Pediatrics. 2018;141:e20170737.
Parker MG, Barrero-Castillero A, Corwin BK, Kavanagh PL, Belfort MB, Wang CJ. Pasteurized human donor milk use among US level 3 neonatal intensive care units. J Hum Lact. 2013;29:381–9.
Perrine CG, Scanlon KS. Prevalence of use of human milk in US advanced care neonatal units. Pediatrics. 2013;131:1066–71.
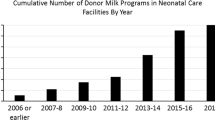
Perrin MT. Donor human milk and fortifier use in United States level 2, 3, and 4 neonatal care hospitals. J Pediatr Gastroenterol Nutr. 2018;66:664–9.
Parker MG, Burnham LA, Kerr SM, Belfort MB, Perrin MT, Corwin MJ, et al. National prevalence of donor milk use among level 1 nurseries. Hosp Pediatr. 2020;10:1078–86.
Parker MG, Burnham LA, Kerr S, Belfort MB, Perrin M, Corwin M, et al. Prevalence and predictors of donor milk programs among U.S. advanced neonatal care facilities. J Perinatol. 2020;40:672–80.
Human Milk Banking Association of North America. Nonprofit milk banks celebrate modest growth, despite pandemic. 2021. https://www.hmbana.org/news/nonprofit-milk-banks-celebrate-modest-growth-despite-pandemic.html.
Office of the Surgeon General (US); Centers for Disease Control and Prevention (US); Office of Women’s Health (US). The surgeon general’s call to action to support breastfeeding. Rockville (MD): The Surgeon General’s Call to Action to Support Breastfeeding; 2011.
Bennett CJ, Mannel R. A call for medicaid coverage of pasteurized donor milk for foster children. J Hum Lact. 2020;36:86–90.
Ky. Rev. Stat. Ann. § 304.17A-139. https://perma.cc/Y48J-VG6J.
FirstChoice by Select Health of South Carolina. Clinical Policies. 2020. https://www.selecthealthofsc.com/provider/resources/shsc-clinical-policies.aspx.
Markus AR, Krohe S, Garro N, Gerstein M, Pellegrini C. Examining the association between Medicaid coverage and preterm births using 2010–2013 National Vital Statistics Birth Data. J Child Poverty. 2016;23:79–94.
Martin JA, Hamilton BE, Osterman MJK, Driscoll AK. Births: final data for 2019. Natl Vital Stat Rep. 2021;70:1–51.
Goldstein GP, Pai VV, Liu J, Sigurdson K, Vernon LB, Lee HC, et al. Racial/ethnic disparities and human milk use in necrotizing enterocolitis. Pediatr Res. 2020;88:3–9. (Suppl 1)
Arnold LD. U.S. health policy and access to banked donor human milk. Breastfeed Med. 2008;3:221–9.
Patient Protection and Affordable Care Act, 42 U.S.C. § 300gg-13 (2021), 29 C.F.R. 2590.715-2713 (2021), Health Resources & Services Administration, Women’s Preventive Services Guidelines. https://www.hrsa.gov/womens-guidelines-2019. Accessed on 9 Sept 2021.
Shah S, Parvez B, Brumberg HL. Ensuring breastfeeding-supportive legislation. Pediatr Res. 2017;81:394–5.
Patient Protection and Affordable Care Act § 4207, amending the Fair Labor Standards Act and codified at 29 U.S.C.A. § 207(r) (2021). https://perma.cc/HD3E-PQZ5.
Food and Nutrition Service USDoA. Special supplemental nutrition program for women, infants, and children (WIC). 2021. https://www.fns.usda.gov/wic.
Food and Nutrition Service USDoA. Breastfeeding is a priority in the WIC program. 2021. https://www.fns.usda.gov/wic/breastfeeding-priority-wic-program.
Food and Nutrition Service USDoA. Use of banked human breastmilk (BBM) in the WIC program. 2000. https://www.fns.usda.gov/wic/use-banked-human-breastmilk-bbm-wic-program.
Therapeutics FaDAOoP, Staff PMH. FDA advisory committee discusses safety of human milk banks. AAP N. 2011;32:6–6.
Tricare. Banked donor breast milk. 2020. https://www.tricare.mil/CoveredServices/IsItCovered/BankedDonorMilk.
Marinelli KA, Lussier MM, Brownell E, Herson VC, Hagadorn JI. The effect of a donor milk policy on the diet of very low birth weight infants. J Hum Lact. 2014;30:310–6.
Williams T, Nair H, Simpson J, Embleton N. Use of donor human milk and maternal breastfeeding rates: a systematic review. J Hum Lact. 2016;32:212–20.
Patel AL, Johnson TJ, Meier PP. Racial and socioeconomic disparities in breast milk feedings in US neonatal intensive care units. Pediatr Res. 2021;89:344–52.
An Act to Create the Arkansas Breast Milk Bank; To Create the Breast Milk Bank Special Fund; And For Other Purposes; 2021 Arkansas Laws Act 255, § 1, codified at Ark. Code Ann. § 20-7-140 (West 2021). https://perma.cc/6JRA-XUCQ.
Shah S, Brumberg HL, Kuo A, Balasubramaniam V, Wong S, Opipari V. Academic advocacy and promotion: how to climb a ladder not yet built. J Pediatr. 2019;213:4–7 e1.
Earnest MA, Wong SL, Federico SG. Perspective: physician advocacy: what is it and how do we do it? Acad Med. 2010;85:63–67.
United States Department of Health and Human Services (US DHHS); Centers for Disease Control and Prevention (CDC); National Center for Health Statistics (NCHS); Division of Vital Statistics. Natality public-use data 2007–2019, on CDC WONDER Online Database. 2020. https://wonder.cdc.gov/natality-current.html.
Acknowledgements
We are most grateful for the assistance of Pam Brannon, Georgia State University College of Law Coordinator of Faculty Services, and student research assistants Madison Hayes, Colin Daniels, and Kevin Schukle as well as Jennifer Williams, RN INCLC, Andrea K. Welker, J.D, M.A., and the Child Advocacy Today CAT Legal Clinical Program. In addition we would like to thank the American Academy of Pediatrics Section on Neonatal-Perinatal Medicine for grant support to the Georgia Chapter of the American Academy of Pediatrics to advocate for Medicaid coverage of donor human milk in Georgia.
Author information
Authors and Affiliations
Contributions
SIS and RMP conceived the manuscript subject. ATR and ERM equally contributed to the main conceptual ideas, drafted the manuscript with contribution and critical revisions from all authors. MB devised the legal search strategy, reviewed, collated, and interpreted results. All authors discussed the results, edited, and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
RMP and ATR receive salary support from the NEC Society for a PCORI-funded capacity-building and research prioritization award on NEC. RMP serves on the data monitoring committee for IBT Therapeutics and Premier Research. JHK is a paid consultant for Fujifilm and serves as a medical advisor for Medela. He is on the Board of Directors for Innara Health and owns shares in Astarte Medical and Nicolette. All other authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Rose, A.T., Miller, E.R., Butler, M. et al. US state policies for Medicaid coverage of donor human milk. J Perinatol 42, 829–834 (2022). https://doi.org/10.1038/s41372-022-01375-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41372-022-01375-9
This article is cited by
-
Medicaid and newborn care: challenges and opportunities
Journal of Perinatology (2023)
-
Advocacy in neonatology: current issues and introduction to the series
Journal of Perinatology (2023)