Abstract
Objectives
To examine risk factors for mortality among preterm infants during newborn and subsequent hospitalizations, and whether they differ by race/ethnicity.
Study design
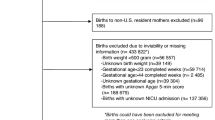
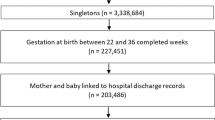
We conducted a cross-sectional analysis using the 2016 Kids Inpatient Database. Hospitalizations of preterm infants were categorized as “newborn” for birth admissions, and “post-newborn” for all others. Multivariate logistic regression was performed to calculate associations of mortality with sociodemographic factors.
Results
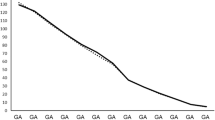
Of 285915 hospitalizations, there were 7827 (2.7%) deaths. During newborn hospitalizations, adjusted OR (aOR) of death equaled 1.14 (95% CI 1.09–1.20) for males, 68.73 (61.91–76.30) for <29 weeks GA, and 0.81 (0.71–0.92) for transfer. Stratified by race/ethnicity, aOR was 0.69 (0.61–0.71) for Medicaid only among black infants. During post-newborn hospitalizations, death was associated with transfer (aOR 5.02, 3.31–7.61).
Conclusions
Risk factors for death differ by hospitalization types and race/ethnicity. Analysis by hospitalization types may identify risk factors that inform public health interventions for reducing infant mortality.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
Data availability
Datasets utilized in the paper are publicly available through the Agency for Healthcare Research and Quality at https://www.hcup-us.ahrq.gov/kidoverview.jsp
References
Kochanek KDM, Xu SL, Arias J, Deaths E. Final data for 2017. Natl Vital- Stat Rep. 2019;68:1–76.
Mathews TJ, Driscoll AK. Trends in infant mortality in the United States, 2005-2014. NCHS. Data Brief. 2017;279:1–8.
Health status. 2016. https://www.oecd-ilibrary.org/content/data/data-00540-en.
Xu J, Murphy SL, Kochanek KD, Bastian B, Arias E. Deaths: final data for 2016. Natl Vital- Stat Rep. 2018;67:1–76.
Collins JW Jr, David RJ. The differential effect of traditional risk factors on infant birthweight among blacks and whites in Chicago. Am J Public Health. 1990;80:679–81.
Collins JW Jr, Wall SN, David RJ. Adequacy of prenatal care utilization, maternal ethnicity, and infant birthweight in Chicago. J Natl Med Assoc. 1997;89:198–203.
Berg CJ, Wilcox LS, d’Almada PJ. The prevalence of socioeconomic and behavioral characteristics and their impact on very low birth weight in black and white infants in Georgia. Matern Child Health J. 2001;5:75–84.
Kleinman JC, Kessel SS. Racial differences in low birth weight. Trends and risk factors. N. Engl J Med. 1987;317:749–53.
El-Sayed AM, Tracy M, Galea S. Life course variation in the relation between maternal marital status and preterm birth. Ann Epidemiol. 2012;22:168–74.
Cooperstock MS, Bakewell J, Herman A, Schramm WF. Association of sociodemographic variables with risk for very preterm birth in twins. Obstet Gynecol. 1998;92:53–6.
Byrd DR, Katcher ML, Peppard P, Durkin M, Remington PL. Infant mortality: explaining black/white disparities in Wisconsin. Matern Child Health J. 2007;11:319–26.
Khanani I, Elam J, Hearn R, Jones C, Maseru N. The impact of prenatal WIC participation on infant mortality and racial disparities. Am J Public Health. 2010;100:S204–9.
Ngui EM, Cortright AL, Michalski K. Relationship of paternity status, welfare reform period, and racial/ethnic disparities in infant mortality. Am J Mens Health. 2015;9:350–9.
Howell EA. Racial disparities in infant mortality: a quality of care perspective. Mt Sinai J Med. 2008;75:31–5.
Underwood MA, Danielsen B, Gilbert WM. Cost, causes and rates of rehospitalization of preterm infants. J Perinatol. 2007;27:614–9.
Kuzniewicz MW, Parker SJ, Schnake-Mahl A, Escobar GJ. Hospital readmissions and emergency department visits in moderate preterm, late preterm, and early term infants. Clin Perinatol. 2013;40:753–75.
Wade KC, Lorch SA, Bakewell-Sachs S, Medoff-Cooper B, Silber JH, Escobar GJ. Pediatric care for preterm infants after NICU discharge: high number of office visits and prescription medications. J Perinatol. 2008;28:696–701.
Cifuentes J, Bronstein J, Phibbs CS, Phibbs RH, Schmitt SK, Carlo WA. Mortality in low birth weight infants according to level of neonatal care at hospital of birth. Pediatrics. 2002;109:745–51.
Jensen EA, Lorch SA, Association between off-peak hour birth and neonatal morbidity and mortality among very low birth weight infants. J Pediatr. 2017;186:41–48.e4.
Shah KP, deRegnier RO, Grobman WA, Bennett AC. Neonatal mortality after interhospital transfer of pregnant women for imminent very preterm birth in Illinois. JAMA Pediatr. 2020;174:358–65.
Lasswell SM, Barfield WD, Rochat RW, Blackmon L. Perinatal regionalization for very low-birth-weight and very preterm infants: a meta-analysis. JAMA. 2010;304:992–1000.
Fang JL, Mara KC, Weaver AL, Clark RH, Carey WA. Outcomes of outborn extremely preterm neonates admitted to a NICU with respiratory distress. Arch Dis Child Fetal Neonatal Ed. 2020;105:33–40.
Odetola FO, Davis MM, Cohn LM, Clark SJ. Interhospital transfer of critically ill and injured children: an evaluation of transfer patterns, resource utilization, and clinical outcomes. J Hosp Med. 2009;4:164–70.
Caskey RN, Davis MM. Differences associated with age, transfer status, and insurance coverage in end-of-life hospital care for children. J Hosp Med. 2008;3:376–83.
Rosenberg AL, Hofer TP, Strachan C, Watts CM, Hayward RA. Accepting critically ill transfer patients: adverse effect on a referral center’s outcome and benchmark measures. Ann Intern Med. 2003;138:882–90.
Sampalis JS, Denis R, Frechette P, Brown R, Fleiszer D, Mulder D. Direct transport to tertiary trauma centers versus transfer from lower level facilities: impact on mortality and morbidity among patients with major trauma. J Trauma. 1997;43:288–95. discussion 95-6.
Rapoport J, Teres D, Lemeshow S, Harris D. Timing of intensive care unit admission in relation to ICU outcome. Crit Care Med. 1990;18:1231–5.
Brandon GD, Adeniyi-Jones S, Kirkby S, Webb D, Culhane JF, Greenspan JS. Are outcomes and care processes for preterm neonates influenced by health insurance status?. Pediatrics. 2009;124:122–7.
Durbin DR, Giardino AP, Shaw KN, Harris MC, Silber JH. The effect of insurance status on likelihood of neonatal interhospital transfer. Pediatrics. 1997;100:E8
Gifford K, Walls J, Ranji U, Salganicoff A, Gomez I. Medicaid coverage of pregnancy and perinatal benefits: results from a state survey. April 2017, https://files.kff.org/attachment/Report-Medicaid-Coverage-of-Pregnancy-and-Perinatal-Benefits [accessed March 2022].
Meghea CI, You Z, Raffo J, Leach RE, Roman LA. Statewide medicaid enhanced prenatal care programs and infant mortality. Pediatrics. 2015;136:334–42.
Bhatt CB, Beck-Sague CM. Medicaid expansion and infant mortality in the United States. Am J Public Health. 2018;108:565–7.
Jacob J, Kamitsuka M, Clark RH, Kelleher AS, Spitzer AR. Etiologies of NICU deaths. Pediatrics 2015;135:e59–65.
Author information
Authors and Affiliations
Contributions
Drs. Matoba and Davis conceptualized and designed the study and drafted the initial manuscript. Dr. Kwon carried out the statistical analyses, reviewed and revised the manuscript. Drs. Collins and Davis critically reviewed the manuscript for important intellectual content. All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Matoba, N., Kwon, S., Collins, J.W. et al. Risk factors for death during newborn and post-newborn hospitalizations among preterm infants. J Perinatol 42, 1288–1293 (2022). https://doi.org/10.1038/s41372-022-01363-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41372-022-01363-z
This article is cited by
-
End of life care in a level IV outborn neonatal intensive care unit
Journal of Perinatology (2024)