Abstract
Objective
To report substance and polysubstance use at the time of delivery.
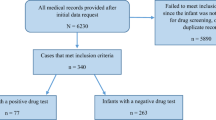
Study design
A cross-sectional study was performed on mothers consented for universal drug testing (99%) during hospital admission at six delivery hospitals in Cincinnati, Ohio. Mass spectrometry urinalysis detected positivity rates of 46 substances. Rates of positive drug tests for individual and common co-occurring substances measured were reported.
Results
2531 maternal samples were tested (88%) and 33% contained cotinine, 11.3% THC, 7.2% opioids, 3.8% cocaine, and 1.9% methamphetamines. Polysubstance use prevalence was as high as 15%. Among mothers testing positive for methadone or buprenorphine, 93% also tested positive for cotinine and 39% tested positive for a third substance in addition to cotinine.
Conclusions
Substance use at delivery is more prevalent than previously reported. Many mothers testing positive for opioids also test positive for other substances, which may increase overdose risk and exacerbate neonatal opioid withdrawal syndrome (NOWS).
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Forray A. Substance use during pregnancy. F1000Research. 2016;5:1–9.
Hayatbakhsh MR, Flenady VJ, Gibbons KS, Kingsbury AM, Hurrion E, Mamun AA, et al. Birth outcomes associated with cannabis use before and during pregnancy. Pediatr Res. 2012;71:215–9.
Fried PA, O’Connell CM. A comparison of the effects of prenatal exposure to tobacco, alcohol, cannabis and caffeine on birth size and subsequent growth. Neurotoxicol Teratol. 1987;9:79–85.
Varner MW, Silver RM, Hogue CJR, Willinger M, Parker CB, Thorsten VR, et al. Association between stillbirth and illicit drug use and smoking during pregnancy. Obstet Gynecol. 2014;123:113–25.
Gunn JKL, Rosales CB, Center KE, Nuñez A, Gibson SJ, Christ C, et al. Prenatal exposure to cannabis and maternal and child health outcomes: A systematic review and meta-analysis. BMJ Open. 2016;6:1–8.
Coleman-Cowger VH, Oga EA, Peters EN, Mark K. Prevalence and associated birth outcomes of co-use of Cannabis and tobacco cigarettes during pregnancy. Neurotoxicol Teratol. 2018;68:84–90.
Hall ES, Mcallister JM, Wexelblatt SL. Developmental disorders and medical complications among infants with subclinical intrauterine opioid exposures. Popul Health Manag. 2019;22:19–24.
Daseking M, Petermann F, Tischler T, Waldmann HC. Smoking during pregnancy is a risk factor for executive function deficits in preschool-aged children. Geburtshilfe Frauenheilkd. 2015;75:64–71.
Nygaard E, Slinning K, Moe V, Walhovd KB. Cognitive function of youths born to mothers with opioid and poly-substance abuse problems during pregnancy. Child Neuropsychol. 2017;23:159–87.
Yeoh SL, Eastwood J, Wright IM, Morton R, Melhuish E, Ward M, et al. Cognitive and motor outcomes of children with prenatal opioid exposure: a systematic review and meta-analysis. JAMA Netw Open. 2019;2:1–14.
Sanlorenzo LA, Cooper WO, Dudley JA, Stratton S, Maalouf FI, Patrick SW. Increased severity of neonatal abstinence syndrome associated with concomitant antenatal opioid and benzodiazepine exposure. Hosp Pediatr. 2019;9:569–75.
Wachman EM, Newby PK, Vreeland J, Byun J, Bonganzi A, Bauchner H, et al. The relationship between maternal opioid agonists and psychiatric medications on length of hospitalization for neonatal abstinence syndrome. J Addict Med. 2011;5:293–9.
Jansson LM, Di Pietro JA, Elko A, Williams EL, Milio L, Velez M. Pregnancies exposed to methadone, methadone and other illicit substances, and poly-drugs without methadone: A comparison of fetal neurobehaviors and infant outcomes. Drug Alcohol Depend. 2012;122:213–9.
Kaltenbach K, Holbrook AM, Coyle MG, Heil SH, Salisbury AL, Stine SM, et al. Predicting treatment for neonatal abstinence syndrome in infants born to women maintained on opioid agonist medication. Addiction. 2012;107:45–52.
Jansson LM, Velez ML, McConnell K, Spencer N, Tuten M, Jones H, et al. Maternal buprenorphine treatment and infant outcome. Drug Alcohol Depend. 2017;180:56–61.
Choo RE, Huestis MA, Schroeder JR, Shin AS, Jones HE. Neonatal abstinence syndrome in methadone-exposed infants is altered by level of prenatal tobacco exposure. Drug Alcohol Depend. 2004;75:253–60.
Desai RJ, Huybrechts KF, Hernandez-Diaz S, Mogun H, Patorno E, Kaltenbach K, et al. Exposure to prescription opioid analgesics in utero and risk of neonatal abstinence syndrome: population based cohort study. BMJ. 2015;350:h2102.
Wexelblatt SL, Ward LP, Torok K, Tisdale E, Meinzen-derr JK, Greenberg JM. Universal maternal drug testing in a high-prevalence region of prescription opiate abuse. J Pediatr. 2015;166:582–6.
Hall ES, Wexelblatt SL, Greenberg JM. Self-reported and laboratory evaluation of late pregnancy nicotine exposure and drugs of abuse. J Perinatol. 2016;36:814–8.
Hall ES, Mcallister JM, Kelly EA, Setchell KD, Megaraj V, Jimenez KL, et al. Regional comparison of self-reported late pregnancy cigarette smoking to mass spectrometry analysis. J Perinatol. 2021;41:2417–23. https://doi.org/10.1038/s41372-021-01045-2.
Roberts SCM, Nuru-Jeter A. Women’s perspectives on screening for alcohol and drug use in prenatal care. Women’s Heal Issues. 2010;20:193–200.
Stone R. Pregnant women and substance use: fear, stigma, and barriers to care. Heal Justice 2015;3:1–15. https://doi.org/10.1186/s40352-015-0015-5.
Campbell J, Matoff-Stepp S, Velez ML, Cox HH, Laughon K. Pregnancy-associated deaths from homicide, suicide, and drug overdose: review of research and the intersection with intimate partner violence. J Women’s Heal. 2021;30:236–44.
Goldman-Mellor S, Margerison CE. Maternal drug-related death and suicide are leading causes of postpartum death in California. Am J Obstet Gynecol. 2019;221:489.e1–489.
Roberts SCM, Pies C. Complex calculations: How drug use during pregnancy becomes a barrier to prenatal care. Matern Child Health J. 2011;15:333–41.
Smith ML, Nichols DC, Underwood P, Fuller Z, Moser MA, LoDico C, et al. Morphine and codeine concentrations in human urine following controlled poppy seeds administration of known opiate content. Forensic Sci Int. 2014;241:87–90.
Rohrig TP, Moore C. The determination of morphine in urine and oral fluid following ingestion of poppy seeds. J Anal Toxicol. 2003;27:449–52.
Mchugh ML. The Chi-square test of independence Lessons in biostatistics. Biochem Med. 2013;23:143–9.
Rothman K. No adjustments are needed for multiple comparisons. Epidemiology 1990;Jan:43–6.
Saville D. Multiple comparison procedures: the practical solution. Am Stat. 1990;44:174–80.
Volkow ND, Han B, Compton WM, McCance-Katz EF. Self-reported medical and nonmedical cannabis use among pregnant women in the United States. JAMA - J Am Med Assoc. 2019;322:167–9.
Crume TL, Juhl AL, Brooks-Russell A, Hall KE, Wymore E, Borgelt LM. Cannabis use during the perinatal period in a state with legalized recreational and medical marijuana: the association between maternal characteristics, breastfeeding patterns, and neonatal outcomes. J Pediatr. 2018;197:90–96.
Ko JY, Farr SL, Tong VT, Creanga AA, Callaghan WM. Prevalence and patterns of marijuana use among pregnant and nonpregnant women of reproductive age. Am J Obstet Gynecol. 2015;213:201.e1–201.e10.
Corsi DJ, Walsh L, Weiss D, Hsu H, El-Chaar D, Hawken S, et al. Association between self-reported prenatal cannabis use and maternal, perinatal, and neonatal outcomes. JAMA - J Am Med Assoc. 2019;322:145–52.
Richardson KA, Hester AK, McLemore GL. Prenatal cannabis exposure - The “first hit” to the endocannabinoid system. Neurotoxicol Teratol. 2016;58:5–14.
Roncero C, Valriberas-Herrero I, Mezzatesta-Gava M, Villegas JL, Aguilar L, Grau-López L. Cannabis use during pregnancy and its relationship with fetal developmental outcomes and psychiatric disorders. A systematic review. Reprod Health. 2020;17:1–9.
Hall ES, Wexelblatt SL, Greenberg JM. Surveillance of intrauterine opioid exposures. 2018;21:486–92.
Percy Z, Brokamp C, Mcallister JM, Ryan P, Wexelblatt SL, Hall ES. Subclinical and overt newborn opioid exposure: prevalence and first-year healthcare utilization. J Pediatr. 2017;222:52–58.
Azadi A, Dildy GA. Universal screening for substance abuse at the time of parturition. Am J Obstet Gynecol. 2008;198:30–32.
John WS, Wu L-T. Trends and correlates of cocaine use and cocaine use disorder in the United States from 2011 to 2015. Drug Alcohol Depend. 2017;180:376–84.
Arria AM, Derauf C, LaGasse LL, Grant P, Shah R, Smith L, et al. Methamphetamine and other substance use during pregnancy: Preliminary estimates from the infant development, environment, and lifestyle (IDEAL) study. Matern Child Health J. 2006;10:293–302.
Wright TE, Schuetter R, Tellei J, Sauvage L. Methamphetamines and pregnancy outcomes. J Addict Med. 2015;9:111–7.
Yossuck P, Tacker DH. Drug positivity findings from a universal umbilical cord tissue drug analysis program in appalachia. J Appl Lab Med. 2020;6:285–97.
Chisolm MS, Fitzsimons H, Leoutsakos JMS, Acquavita SP, Heil SH, Wilson-Murphy M, et al. A comparison of cigarette smoking profiles in opioid-dependent pregnant patients receiving methadone or buprenorphine. Nicotine Tob Res. 2013;15:1297–304.
Jones HE, Heil SH, O’Grady KE, Martin PR, Kaltenbach K, Coyle MG, et al. Smoking in pregnant women screened for an opioid agonist medication study compared to related pregnant and non-pregnant patient samples. Am J Drug Alcohol Abus. 2009;35:375–80.
Jones HE, Heil SH, Baewert A, Arria AM, Kaltenbach K, Martin PR, et al. Buprenorphine treatment of opioid-dependent pregnant women: A comprehensive review. Addiction. 2012;107:5–27.
Maupin R, Lyman R, Fatsis J, Prystowiski E, Nguyen A, Wright C, et al. Characteristics of women who deliver with no prenatal care. J Matern Neonatal Med. 2004;16:45–50.
Friedman SH, Heneghan A, Rosenthal M. Disposition and health outcomes among infants born to mothers with no prenatal care. Child Abus Negl. 2009;33:116–22.
Hulsey EG, Li Y, Hacker K, Williams K, Collins K, Dalton E. Potential emerging risks among children following parental opioid-related overdose death. JAMA - J Am Med Assoc. 2020;174:503–4.
Morris CD, Garver-Apgar CE. Nicotine and opioids: a call for co-treatment as the standard of care. J Behav Heal Serv Res. 2020;47:601–13.
Acknowledgements
We would like to acknowledge financial support from Chiesi Farmaceutici S.p.A and Amgis Foundation, Inc.
Funding
In addition to financial support from Chiesi Farmaceutici S.p.A and Amgis Foundation, Inc., BLS is funded by the NIH/NIDA: K99DA049908.
Author information
Authors and Affiliations
Contributions
BLS and SLW drafted the initial manuscript, along with conducting the investigation, formal analysis, and data curation. Study conceptualization and design were performed by ESH, JMM, TJW, MPM, and KDRS. Methodology was performed by BLS, SLW, ESH, JMM, VM, KLJ, and KDRS. Supervision/oversight for the investigation was conducted by SLW and KDRS. Funding was acquired by SLW and resources were provided by SLW and JMM. All authors assisted in reviewing or editing the manuscript, have given final approval of the version to be published, and agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Competing interests
We disclose that financial support for this work was provided by a grant from Chiesi Farmaceutici and a gift from Amgis Foundation, Inc. However, neither organization participated in study design, data collection, data analysis and interpretation, manuscript preparation, or the decision for manuscript submission. SLW has been a member of the speaker bureau for Abbott Nutrition in the past 2 years.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Smith, B.L., Hall, E.S., McAllister, J.M. et al. Rates of substance and polysubstance use through universal maternal testing at the time of delivery. J Perinatol 42, 1026–1031 (2022). https://doi.org/10.1038/s41372-022-01335-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41372-022-01335-3