Abstract
The American Rescue Plan provides a pathway for states to expand postpartum Medicaid coverage for low-income mothers through 12 months after delivery. Data suggests that extension of post-partum Medicaid coverage should improve access to outpatient health care services, increase healthcare utilization, improve chronic disease management for at-risk mothers, and reduce disparities in care for racial/ethnic groups over-represented in Medicaid. Opportunities to provide increased preventive care for perinatal mood disorders and smoking cessation also exist. Further, this policy may reduce the burden of late maternal mortality. While improved access to contraceptive service postpartum provides a potential mechanism by which birth outcomes may improve, the effect of this policy on NICU admission, low birth weight (LBW) infants, and preterm birth is unknown. We discuss possible birth, infant and maternal health outcomes which may result from this expansion, drawing on data from the 2010 Medicaid Expansion via the Affordable Care Act.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
America’s Health Insurance Plans, “The Value of Medicaid: Providing Access to Care and Preventive Health Services,” April 2018. Available at: https://www.ahip.org/wpcontent/uploads/2018/04/ValueMedicaid_Report_4.4.18.pdf (Accessed 15 July 2021).
Venkataramani M, Pollack CE, Roberts ET. Spillover effects of adult medicaid expansions on children’s use of preventive services. Pediatrics. 2017;140:e20170953.
Ghosh A, Simon K, Sommers BD The effect of state medicaid expansions on prescription drug use: evidence from the Affordable Care Act. National Bureau of Economic Research. January 2017. Working Paper 23044.
Antonisse L, Garfield R, Rudowitz R, Artiga S The effects of medicaid expansion under the ACA: updated findings from a literature review. Kaiser Family Foundation. Issue Brief. March 2018. Available at: https://files.kff.org/attachment/Issue-Brief-The-Effects-of-Medicaid-Expansion-Under-the-ACA-Updated-Findings-from-a-Literature-Review (Accessed 15 July 2021).
American Hospital Association. The importance of health coverage. October 2019. Available at: https://www.aha.org/system/files/media/file/2019/10/report-importance-of-health-coverage_1.pdf (Accessed 15 July 2021).
Antwi YA, Moriya AS, Simon K, Sommers BD. Changes in emergency department use among young adults after the Patient Protection and Affordable Care Act’s dependent coverage provision. Ann Emerg Med. 2015;65:664–72.
Eckert E. Preserving the momentum to extend postpartum medicaid coverage. Women’s Health Issues 2020;30:401–6.
Daw JR, Kozhimannil KB, Admon LK Health Affairs Blog, High rates of perinatal insurance churn persist after the ACA. 2019. Available at: https://www.healthaffairs.org/do/10.1377/hblog20190913.387157/full/ (Accessed 15 July 2021).
Daw JR, Hatfield LA, Swartz K, Sommers BD. Women in the United States experience high rates of coverage ‘Churn’ in the months before and after childbirth. Health Aff. 2017;36:598–606.
Ranji U, Gomez I, Salganicoff A Expanding postpartum medicaid coverage. Kaiser Family Foundation Issues Brief, May 2019. Available at: http://files.kff.org/attachment/Issue-Brief-Expanding-Postpartum-Medicaid-Coverage (Accessed 5 December 2020).
Najmabadi N Texas lawmakers split over how long to extend Medicaid health coverage for new mothers. The Texas Tribune, May 24, 2021. Available at: https://www.texastribune.org/2021/05/21/texas-medicaid-health-mothers/ (Accessed 30 July 2021).
Ranji U, Gomez I, Salganicoff A Expanding Postpartum Medicaid Coverage. Kaiser Family Foundation, Women’s Health Policy Issue Brief, Marcy 2021. Available at: https://www.kff.org/womens-health-policy/issue-brief/expanding-postpartum-medicaid-coverage/ (Accessed 30 July 2021).
Daw JR, Hatfield LA, Swartz K, Sommers BD. Women in the United States experience high rates of coverage “Churn” in months before and after childbirth. Health Aff. 2017;36:598–606.
Daw JR, Sommers BD. Association of the Affordable Care Act dependent coverage provision with prenatal care use and birth outcomes. JAMA 2018;319:579–87.
Eckert E It’s Past Time to provide continuous medicaid coverage for one year postpartum. Health Affairs, Health Policy Blog. February 6, 2020. Available at: https://www.healthaffairs.org/do/10.1377/hblog20200203.639479/full/ (Accessed 6 July 2021).
Shah S, Kuo AA, Brumberg HL. First aid for Medicaid: losses in children’s health insurance. Pediatr Res. 2021;89(Jan):8–11.
Johnston EM, McMorrow S, Thomas TW, Kenney GM. ACA medicaid expansion and insurance coverage among new mothers living in poverty. Pediatrics 2020;145:e20193178.
McMorrow S, Dubay L, Kenney GM, Johnston EM, Caraveo CA Uninsured New Mothers’ health and health care challenges highlight the benefits of increasing postpartum medicaid coverage. Urban Institute Health Policy Center, May 2020. Available at: https://www.urban.org/sites/default/files/publication/102296/uninsured-new-mothers-health-and-health-care-challenges-highlight-the-benefits-of-increasing-postpartum-medicaid-coverage_0.pdf (Accessed 2 July 2021).
Martin JA, Hamilton BE, Osterman MJK, Driscoll AK, Drake P. Births: final data for 2016. Natl Vital- Stat Rep. 2018;67(Jan):1–55.
Martin JA, Hamilton BE, Osterman MJK Births in the United States, 2017. National Center for Health Statistics Data Brief No. 318. August 2018. Available at: https://www.cdc.gov/nchs/data/databriefs/db318.pdf (Accessed 23 June 2021).
Markus AR, Krohe S, Garro N, Gerstein M, Pellegrini C. Examining the association between Medicaid coverage and preterm births using 2010–2013 National Vital Statistics Birth Data. J Child Poverty. 2017;23(1):79–94.
House Resolution 1319- American Rescue Plan Act of 2021. Section 9812. Modifications to certain coverage under medicaid for pregnant and postpartum women. 117th Congress, 3/11/2021. Available at: https://www.congress.gov/117/bills/hr1319/BILLS-117hr1319enr.pdf (Accessed 20 May 2021).
Ranji U, Salganicoff A, Gomez I Postpartum coverage extension in the American Rescue Plan Act of 2021. Kaiser Family Foundation. Women’s Health Policy. March 18, 2021. Available at: https://www.kff.org/policy-watch/postpartum-coverage-extension-in-the-american-rescue-plan-act-of-2021/ (Accessed 2 June 2021).
Congressional Budget Office. Estimated budgetary effects of HR 1319, American Rescue Plan Act of 2021. Available at: https://www.cbo.gov/publication/57056 (Accessed 2 June 2021).
Medicaid postpartum coverage extension tracker. July 30, 2021. Kaiser Family Foundation. Available at: https://www.kff.org/medicaid/issue-brief/medicaid-postpartum-coverage-extension-tracker/ (Accessed 7 July 2021).
Farrell ME, Evans ML Leaving half the population behind-the continued fight to cover America’s mothers: a call to action. Amer J Obstet Gynecol. 2020;379-82.
Hoyert DL, Maternal mortality rates in the United States, 2019. National Center for Health Statistics, Division of Vital Statistics, April 2021. Available at: https://www.cdc.gov/nchs/data/hestat/maternal-mortality-2021/E-Stat-Maternal-Mortality-Rates-H.pdf (Accessed 8 November 2021).
Eckert E It’s past time to provide continuous medicaid coverage for one year postpartum. Health Affairs, Health Policy Blog. February, 2020. Available at: https://www.healthaffairs.org/do/10.1377/hblog20200203.639479/full/ (Accessed 6 December 2020).
Petersen EE, Davis NL, Goodman D, Cox S, Mayes N, Johnston E, et al. Vital Signs: pregnancy-related deaths, United States, 2011e2015, and strategies for prevention, 13 states, 2013e2017. MMWR Morb Mortal Wkly Rep. 2019;68:423–9.
Kacica M New York State maternal mortality review and NYS VS death data, 2014, 2016, 2017. Data shared at the New York State Perinatal Association Conference, November 5 2020.
Eliason EL. Adoption of medicaid expansion is associated with lower maternal mortality. Women’s Health Issues. 2020;30:147–52.
D’Angelo D, Williams L, Morrow B, Cox S, Harris N, Harrison L, et al. Preconception and interconception health status of women who recently gave birth to a liveborn infant—Pregnancy Risk Assessment Monitoring System (PRAMS), United States, 26 reporting areas, 2004. MMWR Surveill Summ. 2007;56:1–35.
Orr ST, Reiter JP, James SA, Orr CA. Maternal health prior to pregnancy and preterm birth among urban, low income black women in Baltimore: the Baltimore Preterm Birth Study. Ethn Dis. 2012;22:85–89.
Kitzmiller JL, Johnson K, Parker C, Posner SF, Atrash H. Pre-conception care of diabetes, congenital malformations and spontaneous abortions. Diabetes Care. 1996;19:514–41.
Crowther CA, Hiller JE, Moss JR, McPhee AJ, Jeffries WS, Robinson JS. Effect of treatment of gestational diabetes mellitus on pregnancy outcomes. N. Engl J Med. 2005;352:2477–86.
Black MH, Chou H, Sacks DA, Dublin S, Lawrence JM, Harrison TN, et al. Prehypertension prior to or during early pregnancy is associated with increased risk for hypertensive disorders in pregnancy and gestational diabetes. J Hypertens. 2015;33:1860–7.
McBride CA, Bernstein IM, Badger GJ, Horbar JD, Soll RF. The effect of maternal hypertension on mortality in infants 22, 29 weeks gestation. Pregnancy Hypertens. 2015;5:362–6.
Montoro MN. Management of hypothyroidism during pregnancy. Clin Obstet Gynecol. 1997;40:65–80.
Idris I, Srinivasan R, Simm A. Maternal hypothyroidism in early and late gestation: effects on neonatal and obstetrical outcome. Clin Endorinol. 2005;63:560–5.
Shah SI, Brumberg HL. Predictions of the Affordable Care Act’s impact on neonatal practice. J Perinatol. 2016;36:586–92.
American College of Obstetricians and Gynecologists Committee Opinion No. 736. Optimizing postpartum care. Obstet Gynecol. 2018;131:e140–50.
Tully KP, Stuebe AM, Verbiest SB. The fourth trimester: a critical transition period with unmet maternal health needs. Am J Obstet Gynecol. 2017;217:37–41.
Myerson R, Crawford S, Wherry LR. Medicaid expansion increased preconception health counseling, folic acid intake, an postpartum contraception. Health Aff. 2020;39:1883–90.
Margerison CE, MacCallum CL, Chen J, Zamani-Hank Y, Kaestner R. Impacts of medicaid expansion on health among women of reproductive age. Am J Prev Med. 2020;58:1–11.
Bryant A, Blake-Lamb T, Hatoum I, Kotelchuck M. Women’s use of health care in the first 2 years postpartum: occurrence and correlates. Mater Child Health J. 2016;20(Suppl 1):81–91.
Medicaid: Prenatal and Postpartum Care: Postpartum Care. Medicaid.gov. Available at: https://www.medicaid.gov/state-overviews/scorecard/postpartum-care/index.html (Accessed 23 May 2021).
Ahrens KA, Nelson H, Stidd RL, Moskosky S, Hutcheon JA. Short interpregnancy intervals and adverse perinatal outcomes in high-resource settings: an updated systematic review. Paediatr Perinat Epidemiol. 2019;33:O25–O47.
DiBari JN, Yu SM, Chao SM, Lu MC Use of postpartum care: predictors and barriers. J Pregnancy 2014, Article ID 530769
Levine LD, Nkonde-Price C, Limaye M, Srinivas SK. Factors associated with postpartum follow-up and persistent hypertension among women with severe preeclampsia. J Perinatol. 2016;36:1079–82.
Ehrenthal DB, Maiden K, Rogers S, Ball A. Postpartum healthcare after gestational diabetes and hypertension. J Women’s Health. 2014;23:760–4.
Gordon SH, Sommers BD, Wilson IB, Trivedi AN. Effects of medicaid expansion on postpartum coverage and outpatient utilization. Health Aff. 2020;39(Jan):77–84.
Stuebe A, Moore JE, Mittal P, Reddy L, Low LK, Brown H Extending medicaid coverage for postpartum moms. Health Affairs, Health Policy Blog, May 6, 2019 Available at: https://www.healthaffairs.org/do/10.1377/hblog20190501.254675/full/ (Accessed 1 December 2020).
Stewart DE, Vigod S. Postpartum Depression. N. Engl J Med. 2016;375:2177–85.
Levinson M, Parvez B, Aboudi DA, Shah S Impact of maternal stressors and neonatal clinical factors in post-partum depression screening scores. J Matern Fetal Neonatal Med. 2020 1–9.
Robertson E, Grace S, Wallington T, Stewart DE. Antenatal risk factors for postpartum depression: a synthesis of recent literature. Gen Hosp Psychiatry. 2004;26:289–95.
O’Connor E, Rossom RC, Henninger M, Groom HC, Burda BU. Primary care screening for and treatment of depression in pregnant and postpartum women evidence report and systematic review for the US Preventative Services Task Force. JAMA 2016;315:388–406.
Chaudron LH. Postpartum depression: what pediatricians need to know. Pediatr Rev. 2003;24:154–61.
Bishop TF, Press MJ, Keyhani S, Pincus HA. Acceptance of insurance by psychiatrists and the implications for access to mental health care. JAMA Psychiatry. 2014;71:176–81.
Chester A, Schmit S, Alker J, Golden O Medicaid expansion promotes children’s development and family success by treating maternal depression. Georgetown University Health Policy Institute. Center for Children and Families, July 2016. Available at: https://ccf.georgetown.edu/wp-content/uploads/2016/07/Maternal-Depression-4.pdf (Accessed 6 July 2021).
Baicker K, Taubman SL, Allen HL, Bernstein M, Gruber JH, Newhouse JP, et al. The Oregon experiment-effects of Medicaid on clinical outcomes. N. Engl J Med. 2013;368:1713–22.
Shah S. Smoking cessation counseling and PPSV 23-valent pneumococcal polysaccharide vaccine administration parents of neonatal intensive care unit (NICU)-admitted infants: a life-changing opportunity. J Neonatal-Perinat Med. 2011;4:263–7.
Cornelius M, Day N. Developmental consequences of prenatal tobacco exposure. Curr Opin Neurol. 2009;22:121–5.
Kondracki AJ. Prevalence and patters of cigarette smoking before and during early and late pregnancy according to maternal characteristics: the first national data based on the 2003 birth certificate revision, United States, 2016. Reprod Health. 2019;16:142.
Young S, Sherrill D, Arnott J, Diepeveen D, LeSouef PN, Landau LI. Parental factors affecting respiratory function during the first year of life. Pediatr Pulmonol. 2000;29:331–40.
Farber HJ, Groner J, Walley S, Nelson K. Protecting children from tobacco, nicotine and tobacco smoke. Pediatrics. 2015;136:e1439–e1467.
Jarlenski J, Bleich SN, Bennett WL, Stuart EA, Barry CL. Medicaid enrollment policy increased smoking cessation among pregnant women but had no impact on birth outcomes. Health Aff. 2014;33:997–1005.
Adams EK, Markowitz S, Dietz P, Tong VT. Expansion of medicaid covered smoking cessation services: maternal smoking and birth outcomes. Medicare Medicaid Res Rev. 2013;3:E1–E23.
Brown CC, Moore JE, Felix HC, Stewart MK, Bird TM, Lowery CL, et al. Association of state medicaid expansion status with low birth weight and preterm birth. JAMA 2019;321:1598–609.
Martin JA, Hamilton BE, Osterman MJK, Driscoll AK, Drake P. Births: final data for 2017. Natl Vital- Stat Rep. 2018;67:1–50.
Bhatt CB, Beck-Sagué CM. Medicaid expansion and infant mortality in the United States. Am J Public Health. 2018;108:565–7.
Conway K, Deb P. Is prenatal care really ineffective? Or, is the ‘devil’ in the distribution. J Health Econ. 2005;25:489–513.
Fiscella K. Does prenatal care improve birth outcomes? A critical review. Obstet Gynecol. 1995;85:468–79.
VanderWeele TJ, Lantos J, Siddique J, Lauderdale DS. A comparison of four prenatal care indices in birth outcome models: comparable results for predicting small-for-gestational-age outcome but different results for preterm birth or infant mortality. J Clin Epidemiol. 2009;62:438–45.
Chetty R, Stepner M, Abraham S, Lin S, Scuderi B, Turner N, et al. The association between income and life expectancy in the United States, 2001–2014. JAMA. 2016;315:1750–66.
Borque SL, Juhl AL, Hwang SS Trends in maternal insurance status and effect on neonatal outcomes in Colorado. Pediatric Academic Societies, (Accessed 6 May 2018).
Hartman S, Brown E, Holub D, Horst M, Loomis E. Optimizing interconception care: rationale for the IMPLICIT model. Semin Perinatol. 2020;44:151247–56.
Clapp MA, James KE, Kaimal A, Daw JR. Preconception coverage before and after the affordable care act medicaid expansions. Obstet Gynecol. 2018;132:1394–1400.
Partridge S, Balayla J, Holcroft CA, Abenhaim HA. Inadequate prenatal care utilization and risks of infant mortality and poor birth outcome: a retrospective analysis of 28,729,765 U.S. deliveries over 8 years. Am J Perinatol. 2012;29:787–93.
Rodrigues T, Barros HSO. Short interpregnancy interval and risk of spontaneous preterm delivery. Eur J Obstet Gynecol Reprod Biol. 2008;136:184–8.
McKinney D, House M, Chen A, Muglia L, DeFranco E. The influence of interpregnancy interval on infant mortality. Am J Obstet Gynecol. 2017;216:316.e1–316.e9.
Zhu BP, Rolfs RT, Nangle BE, Horan JM. Effect of the interval between pregnancies on perinatal outcomes. N. Engl J Med. 1999;340:589–94.
American College of Obstetricians and Gynecologists. Obstetric Care Consensus, Interpregnancy Care. January 2019. Available at: https://www.acog.org/clinical/clinical-guidance/obstetric-care-consensus/articles/2019/01/interpregnancy-care (Accessed 5 July 2021).
Moniz MH, Kirch MA, Solway E, Goold SD, Ayanian JZ, Kieffer EC, et al. Association of access to family planning services with medicaid expansion among female enrollees in Michigan. JAMA Netw Open. 2018;1:e181627.
Kavanaugh ML, Douglas-Hall A, Finn SM. Health insurance coverage and contraceptive use at the state level: findings from the 2017 behavioral risk factor surveillance system. Contracept X. 2019;2:100014.
Johnson K, Rosenbaum S, Handley M The next steps to advance maternal and child health in medicaid: filling gaps in postpartum coverage and newborn enrollment. Health Affairs, Health Policy Blog, January 9, 2020. Available at: https://www.healthaffairs.org/do/10.1377/hblog20191230.967912/full/ (Accessed 6 December 2020).
Grosse SD, Waitzman NJ, Yang N, Abe K, Barfield WD. Employer sponsored plan expenditures for infants born preterm. Pediatrics 2017;140:e20171078.
Institute of Medicine (US) Committee on Understanding Premature Birth and Assuring Healthy Outcomes. Preterm Birth: causes, consequences, and prevention. Behrman RE, Butler AS, editors. Washington (DC): National Academies Press (US); 2007.
Kuo DZ, Berry JG, Hall M, Lyle R, Stille CJ. Health-care spending and utilization for children discharged from a neonatal intensive care unit. J Perinatol. 2018;38:734–41.
Barradas DT, Wasserman MP, Daniel-Robinson L, Bruce MA, DiSantis KO, Navarro FH, et al. Hospital utilization and costs among preterm infant by payer: nationwide inpatient sample. 2009 Matern Child Health J. 2016;20:808–18.
McLaurin KK, Wade SW, Kong AM, Diakun D, Olajide IR, Germano J. Characteristics and health care utilization of otherwise healthy commercially and Medicaid-insured preterm and full term infants in the US. Pediatr Health Med Ther. 2019;10:21–31.
Author information
Authors and Affiliations
Contributions
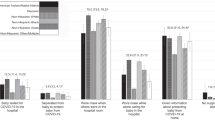
SS wrote the draft of the manuscript, made revisions based on reviewers suggestions and created Fig. 1. HF reviewed several drafts of the manuscript, created Table 1 and made critical revisions of the draft. Medicaid and Moms: The Potential Impact of Extending Medicaid Coverage to Mothers for 1 Year After Delivery. SS MD FAAP, HF MD, FAAP.
Corresponding author
Ethics declarations
competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Shah, S., Friedman, H. Medicaid and moms: the potential impact of extending medicaid coverage to mothers for 1 year after delivery. J Perinatol 42, 819–824 (2022). https://doi.org/10.1038/s41372-021-01299-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41372-021-01299-w
This article is cited by
-
Advocacy in neonatology: current issues and introduction to the series
Journal of Perinatology (2023)
-
“Medi-Mom”: maternal mortality and extending postpartum Medicaid coverage
Pediatric Research (2023)
-
Substance Use Disorder-Related Deaths and Maternal Mortality in New Mexico, 2015–2019
Maternal and Child Health Journal (2023)