Abstract
Objective
Describe sources of discrepancy between self-assessed LoMC (level of maternal care) and CDC LOCATe®-assessed (Levels of Care Assessment Tool) LoMC.
Study design
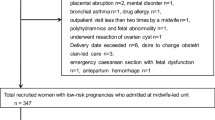
CDC LOCATe® was implemented at 480 facilities in 13 jurisdictions, including states, territories, perinatal regions, and hospital systems, in the U.S. Cross-sectional analyses were conducted to compare facilities’ self-reported LoMC and LOCATe®-assessed LoMC.
Result
Among 418 facilities that self-reported an LoMC, 41.4% self-reported a higher LoMC than their LOCATe®-assessed LoMC. Among facilities with discrepancies, the most common elements lacking to meet self-reported LoMC included availability of maternal-fetal medicine (27.7%), obstetric-specializing anesthesiologist (16.2%), and obstetric ultrasound services (12.1%).
Conclusion
Two in five facilities self-report a LoMC higher than their LOCATe®-assessed LoMC, indicating discrepancies between perceived maternal care capabilities and those recommended in current LoMC guidelines. Results highlight an opportunity for states to engage with facilities, health systems, and other stakeholders about LoMC and collaborate to strengthen systems for improving maternal care delivery.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Ryan GM Jr. Toward improving the outcome of pregnancy: recommendations for the regional development of perinatal health services. Obstet Gynecol. 1975;46:375–84.
D’Alton ME, Bonanno CA, Berkowitz RL, Brown HL, Copel JA, Cunningham FG, et al. Putting the “M” back in maternal-fetal medicine. Am J Obstet Gynecol. 2013;208:442–8.
Menard MK, Kilpatrick S, Saade G, Hollier LM, Joseph GF Jr, Barfield W, et al. Levels of maternal care. Am J Obstet Gynecol. 2015;212:259–71.
Kilpatrick SJ, Menard MK, Zahn CM, Callaghan WM. Obstetric care consensus #9: levels of maternal care: (replaces Obstetric Care Consensus Number 2, February 2015). Am J Obstet Gynecol. 2019;221:B19–b30.
Lu MC, Highsmith K, de la Cruz D, Atrash HK. Putting the “M” Back in the Maternal and Child Health Bureau: Reducing Maternal Mortality and Morbidity. Matern Child Health J. 2015;19:1435–9.
Building US Capacity to Review and Prevent Maternal Deaths. Report from Nine Maternal Mortality Review Committees. 2018.
Nowakowski L, Barfield WD, Kroelinger CD, Lauver CB, Lawler MH, White VA, et al. Assessment of state measures of risk-appropriate care for very low birth weight infants and recommendations for enhancing regionalized state systems. Matern Child Health J. 2012;16:217–27.
Blackmon LR, Barfield WD, Stark AR. Hospital neonatal services in the United States: variation in definitions, criteria, and regulatory status, 2008. J Perinatol. 2009;29:788–94.
Vladutiu CJ, Minnaert JJ, Sosa S, Menard MK. Levels of Maternal Care in the United States: An Assessment of Publicly Available State Guidelines. J Womens Health (Larchmt). 2020;29:353–61.
Kroelinger CD, Okoroh EM, Goodman DA, Lasswell SM, Barfield WD. Designation of neonatal levels of care: a review of state regulatory and monitoring policies. J Perinatol. 2019;40:369–76.
National Institute for Children’s Health Quality (NICHQ). Collaborative Improvement and Innovation Network to Reduce Infant Mortality (Infant Mortality CoIIN) [Available from: https://www.nichq.org/project/collaborative-improvement-and-innovation-network-reduce-infant-mortality-infant-mortality.
Catalano A, Bennett A, Busacker A, Carr A, Goodman D, Kroelinger C, et al. Implementing CDC’s level of care assessment tool (LOCATe): a national collaboration to improve maternal and child health. J Women’s Health (Larchmt). 2017;26:1265–9.
Health DoR. CDC Levels of Care Assessment Tool (CDC LOCATe) https://www.cdc.gov/reproductivehealth/maternalinfanthealth/cdc-locate/index.html: Centers for Disease Control and Prevention; updated May 29, 2019.
Zahn CM, Remick A, Catalano A, Goodman D, Kilpatrick SJ, Menard MK. Levels of maternal care verification pilot: translating guidance into practice. Obstet Gynecol. 2018;132:1401–6.
American Association of Birth Centers. Standards for Birth Centers. 2017.
Commission for the Accreditation of Birth Centers. Get Accredited 2020. Available from: https://www.birthcenteraccreditation.org/get-accredited/.
Committee on Trauma. Resources for Optimal Care of the Injured Patient. American College of Surgeons; 2014.
American Academy of Pediatrics Committee of Fetus and Neonatal. Levels of Neonatal Care. Pediatrics.2012;130:587–97.
Freiman MP, Cromwell J. Reimbursement of sole community hospitals under Medicare’s prospective payment system. Health Care Financing Review. 1987;9:39–54.
Whitaker GR, Holmes GM, Pink HG. The Impact of the Low Volume Hospital (LVH) Program on the Viability of Small, Rural Hospitals. NC Rural Health Research Program. 2016;1–7. [Available from: https://www.shepscenter.unc.edu/wp-content/uploads/dlm_uploads/2016/10/Impact-of-LVH.pdf.
Acknowledgements
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention. We want to thank the implementing agencies responsible for LOCATe® in each jurisdiction that provided CDC LOCATe® data included in this analysis. Any published findings and conclusions do not necessarily represent the official position of the jurisdictions that participated in LOCATe®. This project was supported in part by an appointment to the Research Participation Program at the Centers for Disease Control and Prevention administered by the Oak Ridge Institute for Science and Education through an interagency agreement between the U.S. Department of Energy and the Centers for Disease Control and Prevention.
Author information
Authors and Affiliations
Contributions
SM conceptualized and designed the work; acquired, analyzed, and interpreted the data; and drafted the manuscript. JB and MM conceptualized and designed the work and revised the manuscript critically for important intellectual content. AE, MB, and DG conceptualized and designed the work; acquired the data; and revised the manuscript critically for important intellectual content.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Madni, S.A., Ewing, A.C., Beauregard, J.L. et al. CDC LOCATe: discrepancies between self-reported level of maternal care and LOCATe-assessed level of maternal care among 463 birth facilities. J Perinatol 42, 589–594 (2022). https://doi.org/10.1038/s41372-021-01268-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41372-021-01268-3
This article is cited by
-
Validation of a measure of hospital maternal level of care for the United States
BMC Health Services Research (2024)
-
Operationalizing risk-appropriate perinatal care in a rural US State: directions for policy and practice
BMC Health Services Research (2023)
-
Levels of neonatal care among birth facilities in 20 states and other jurisdictions: CDC levels of care assessment toolSM (CDC LOCATeSM)
Journal of Perinatology (2023)
-
Maternal and neonatal risk-appropriate care: gaps, strategies, and areas for further research
Journal of Perinatology (2023)