Abstract
Objective
To increase the usage rate of mothers’ own milk (MOM) among neonates with prenatal opioid exposure from a baseline average of 47% to an average of 75% over two years.
Study design
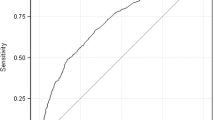
Between October 2018 and December 2020, we implemented various Plan-Do-Study-Act cycles that involved engaging providers in postpartum counseling for mothers with opioid dependence, using electronic medical records to track the rate of counseling, providing NAS educational materials to parents, and establishing a rooming-in unit. Our outcome measure was the provision of MOM to eligible neonates, while our process measure was the rate of postpartum counseling.
Results
During this initiative, we witnessed a special cause variation with an increase in the usage rate of MOM from a baseline of 47% to a 27-month average of 85% by December 2020.
Conclusion
A series of quality improvement efforts resulted in increased usage of MOM among infants at risk of NAS.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Haight SC, Ko JY, Tong VT, Bohm MK, Callaghan WM. Opioid use disorder documented at delivery hospitalization - United States, 1999-2014. MMWR Morb Mortal Wkly Rep. 2018;67:845–9.
Hirai AH, Ko JY, Owens PL, Stocks C, Patrick SW. Neonatal abstinence syndrome and maternal opioid-related diagnoses in the US, 2010-2017. JAMA 2021;325:146–55.
Hudak ML, Tan RC. Committee on drugs, committee on fetus and newborn, American Academy of Pediatrics. Neonatal drug withdrawal. Pediatrics 2012;129:e540–60.
Kocherlakota P. Neonatal abstinence syndrome. Pediatrics 2014;134:e547–61.
Winkelman TNA, Villapiano N, Kozhimannil KB, Davis MM, Patrick SW Incidence and costs of neonatal abstinence syndrome among infants with medicaid: 2004–2014. Pediatrics. 2018;141:e20173520.
Wang X, Zhu Y, Dave CV, Alrwisan AA, Voils SA, Winterstein AG. Trends of neonatal abstinence syndrome epidemic and maternal risk factors in Florida. Pharmacotherapy 2017;37:806–13.
Reddy UM, Davis JM, Ren Z, Greene MF. Opioid use in pregnancy, neonatal abstinence syndrome, and childhood outcomes workshop invited speakers. opioid use in pregnancy, neonatal abstinence syndrome, and childhood outcomes: executive summary of a joint workshop by the eunice kennedy shriver national institute of child health and human development, american college of obstetricians and gynecologists, american academy of pediatrics, society for maternal-fetal medicine, centers for disease control and prevention, and the march of dimes foundation. Obstet Gynecol. 2017;130:10–28.
Wachman EM, Grossman M, Schiff DM, Philipp BL, Minear S, Hutton E, et al. Quality improvement initiative to improve inpatient outcomes for neonatal abstinence syndrome. J Perinatol. 2018;38:1114–22.
Walsh MC, Crowley M, Wexelblatt S, Ford S, Kuhnell P, Kaplan HC, et al. Ohio perinatal quality collaborative. ohio perinatal quality collaborative improves care of neonatal narcotic abstinence syndrome. Pediatrics. 2018;141:e20170900.
Reid CN, Foti TR, Mbah AK, Hudak ML, Balakrishnan M, Kirby RS, et al. Multilevel factors associated with length of stay for neonatal abstinence syndrome in Florida’s NICUs: 2010–2015. J Perinatol. 2021;41:1389–96.
Lembeck AL, Tuttle D, Locke R, Lawler L, Jimenez P, Mackley A, Paul DA. Breastfeeding and formula selection in neonatal abstinence syndrome. Am J Perinatol. 2020 Jun 30.
Welle-Strand GK, Skurtveit S, Jansson LM, Bakstad B, Bjarko L, Ravndal E. Breastfeeding reduces the need for withdrawal treatment in opioid-exposed infants. Acta Paediatr. 2013;102:1060–6.
Abdel-Latif ME, Pinner J, Clews S, Cooke F, Lui K, Oei J. Effects of breast milk on the severity and outcome of neonatal abstinence syndrome among infants of drug-dependent mothers. Pediatrics 2006;117:e1163–9.
MacVicar S, Humphrey T, Forbes-McKay KE. Breastfeeding and the substance-exposed mother and baby. Birth. 2018;45:450–8.
Short VL, Gannon M, Abatemarco DJ. The association between breastfeeding and length of hospital stay among infants diagnosed with neonatal abstinence syndrome: a population-based study of in-hospital births. Breastfeed Med. 2016;11:343–9.
Wachman EM, Byun J, Philipp BL. Breastfeeding rates among mothers of infants with neonatal abstinence syndrome. Breastfeed Med. 2010;5:159–64.
Reece-Stremtan S, Marinelli KA. ABM clinical protocol #21: guidelines for breastfeeding and substance use or substance use disorder, revised 2015. Breastfeed Med. 2015;10:135–41.
Crook K, Brandon D. Prenatal breastfeeding education: impact on infants with neonatal abstinence syndrome. Adv Neonatal Care. 2017;17:299–305.
MacMillan KDL, Rendon CP, Verma K, Riblet N, Washer DB, Volpe Holmes A. Association of rooming-in with outcomes for neonatal abstinence syndrome: a systematic review and meta-analysis. JAMA Pediatr. 2018;172:345–51.
Benneyan JC, Lloyd RC, Plsek PE. Statistical process control as a tool for research and healthcare improvement. Qual Saf Health Care. 2003;12:458–64.
Mohammed MA, Worthington P, Woodall WH. Plotting basic control charts: tutorial notes for healthcare practitioners. Qual Saf Health Care. 2008;17:137–45.
Whalen BL, Holmes AV, Blythe S. Models of care for neonatal abstinence syndrome: what works? Semin Fetal Neonatal Med. 2019;24:121–32.
Wachman EM, Schiff DM, Silverstein M. Neonatal abstinence syndrome: advances in diagnosis and treatment. JAMA 2018;319:1362–74.
Allegaert K, van den Anker JN. Neonatal abstinence syndrome: on the evidence to add breastfeeding to any clinical pathway. Pediatr Crit Care Med. 2014;15:579–80.
McKnight S, Coo H, Davies G, Holmes B, Newman A, Newton L, et al. Rooming-in for infants at risk of neonatal abstinence syndrome. Am J Perinatol. 2016;33:495–501.
Funding
The authors did not receive any funding for this work. Financial support was obtained from CMN and Walmart to establish private rooms in the NAS unit.
Author information
Authors and Affiliations
Contributions
IH, SS, JC, MM, AE, PS helped design and implement the study. AA, JM collected data on MOM usage. JV helped to implement the study and educate the staff members. IH, SS, JC helped to write the manuscript. MLH provided guidance, mentorship, and reviewed and critically revised the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Shukla, S., Hanna, I., Cortez, J. et al. Increasing usage of mother’s own milk in neonates at risk of neonatal abstinence syndrome: MOM-NAS quality improvement initiative. J Perinatol 41, 2684–2689 (2021). https://doi.org/10.1038/s41372-021-01209-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41372-021-01209-0
This article is cited by
-
Intrauterine Drug Exposure—What the Pediatrician Needs to Know
Current Treatment Options in Pediatrics (2023)
-
Neonatal abstinence syndrome and mother’s own milk at discharge
Journal of Perinatology (2022)