Abstract
Objective
To characterize pulse oxygen saturation (SpO2) trajectories and respiratory interventions after birth for newborns with cyanotic congenital heart disease (CCHD).
Study design
Retrospective single-site study of newborns ≥32 weeks gestation with CCHD: single ventricle with critical aortic obstruction (SV-CAO), critical pulmonic obstruction (CPO), transposition of the great arteries (TGA). Minute-to-minute SpO2 values and respiratory interventions were summarized and compared.
Results
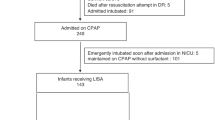
Two hundred infants were enrolled. SpO2 at each minute differed across groups (p < 0.01), with the lowest values in TGA. All interventions were most frequent in TGA (p < 0.01). Continuous positive airway pressure was provided in 22% SV-CAO, 23% CPO, and 66% TGA. Positive pressure ventilation occurred in 7% SV-CAO, 14% CPO, and 33% TGA. Intubation occurred in 4% SV-CAO, 10% CPO, and 53% TGA.
Conclusion
We defined SpO2 trajectories and delivery room respiratory interventions for three CCHD phenotypes. These results inform delivery room management of these high-risk populations.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Finnemore A, Groves A. Physiology of the fetal and transitional circulation. Semin Fetal Neonatal Med. 2015;20:210–6.
Kotaska K, Urinovska R, Klapkova E, Prusa R, Rob L, Binder T. Re-evaluation of cord blood arterial and venous reference ranges for pH, pO2, pCO2, according to spontaneous or cesarean delivery. J Clin Lab Anal. 2010;24:300–4.
Kiserud T. Physiology of the fetal circulation. Semin Fetal Neonatal Med. 2005;10:493–503.
Dawson JA, Kamlin COF, Vento M, Wong C, Cole TJ, Donath SM, et al. Defining the reference range for oxygen saturation for infants after birth. Pediatrics. 2010;125:e1340–7.
Kamlin COF, O’Donnell CPF, Davis PG, Morley CJ. Oxygen saturation in healthy infants immediately after birth. J Pediatr. 2006;148:585–9.
Rabi Y, Yee W, Chen SY, Singhal N. Oxygen saturation trends immediately after birth. J Pediatr. 2006;148:590–4.
Vento M, Cubells E, Escobar JJ, Escrig R, Aguar M, Brugada M, et al. Oxygen saturation after birth in preterm infants treated with continuous positive airway pressure and air: assessment of gender differences and comparison with a published nomogram. Arch Dis Child Fetal Neonatal Ed. 2013;98:F228–32.
Weiner J, Zaichkin GM (eds.). Textbook of Neonatal Resuscitation (NRP), 7th Ed. American Academy of Pediatrics, 2016 https://ebooks.aappublications.org/content/9781610020251/9781610020251.
Hoffman JIE, Kaplan S. The incidence of congenital heart disease. J Am Coll Cardiol. 2002;39:1890–900.
Reller MD, Strickland MJ, Riehle-Colarusso T, Mahle WT, Correa A. Prevalence of congenital heart defects in Metropolitan Atlanta, 1998–2005. J Pediatr. 2008;153:807–13.
Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)-A metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inf. 2009;42:377–81.
Harris PA, Taylor R, Minor BL, Elliott V, Fernandez M, O’Neal L, et al. The REDCap consortium: Building an international community of software platform partners. J Biomed Inf. 2019;95:103208.
R Core Team. R: A language and environment for statistical computing. R Found. Stat Comput. 2020. https://www.r-project.org/.
Martin JA, Hamilton BE, Osterman MJK, Driscoll AK. Births: Final Data for 2018. Natl Vital Stat Rep. 2018;68:1–47.
Padilla-Sánchez C, Baixauli-Alacreu S, Cañada-Martínez AJ, Solaz-García Á, Alemany-Anchel MJ, Torres MV. Delayed vs Immediate Cord Clamping Changes Oxygen Saturation and Heart Rate Patterns in the First Minutes after Birth. J Pediatr. 2020. https://doi.org/10.1016/j.jpeds.2020.07.045.
Niles DE, Cines C, Insley E, Foglia EE, Elci OU, Skåre C, et al. Incidence and characteristics of positive pressure ventilation delivered to newborns in a US tertiary academic hospital. Resuscitation. 2017;115:102–9.
Bjorland PA, Øymar K, Ersdal HL, Rettedal SI. Incidence of newborn resuscitative interventions at birth and short-term outcomes: A regional population-based study. BMJ Paediatr Open. 2019;3:13–16.
Afjeh S-A, Sabzehei M-K, Esmaili F. Neonatal resuscitation in the delivery room from a tertiary level hospital: Risk factors and outcome. Iran J Pediatr. 2013;23:675–80.
Perlman JM, Wyllie J, Kattwinkel J, Wyckoff MH, Aziz K, Guinsburg R et al. Part 7: Neonatal resuscitation: 2015 international consensus on cardiopulmonary resuscitation and emergency cardiovascular care science with treatment recommendations. 2015. https://doi.org/10.1161/CIR.0000000000000276.
Lawrenson J, Eyskens B, Vlasselaers D, Gewillig M. Manipulating parallel circuits: the perioperative management of patients with complex congenital cardiac disease. Cardiol Young 2003;13:316–22.
Donofrio MT, Moon-Grady AJ, Hornberger LK, Copel JA, Sklansky MS, Abuhamad A, et al. Diagnosis and treatment of fetal cardiac disease: A scientific statement from the american heart association. Circulation. 2014;129:2183–242.
Donofrio M. Predicting the future: delivery room planning of congenital heart disease diagnosed by fetal echocardiography. Am J Perinatol. 2018;35:549–52.
Badurdeen S, Roberts C, Blank D, Miller S, Stojanovska V, Davis P et al. Haemodynamic Instability and Brain Injury in Neonates Exposed to Hypoxia−Ischaemia. Brain Sci. 2019; 9. https://doi.org/10.3390/brainsci9030049.
Oei JL, Vento M. Is there a ‘right’ amount of oxygen for preterm infant stabilization at birth? Front Pediatr. 2019;7:354.
Katheria AC, Hassen K, Rich W, Poeltler D, Finer N. Resuscitation outcomes of infants that do not achieve a 5 min target SpO(2) saturation. J Perinatol. 2019;39:1635–9.
Oei JL, Finer NN, Saugstad OD, Wright IM, Rabi Y, Tarnow-Mordi W et al. Outcomes of oxygen saturation targeting during delivery room stabilisation of preterm infants. Arch Dis Child Fetal Neonatal Ed. 2017. https://doi.org/10.1136/archdischild-2016-312366.
Kelly CJ, Arulkumaran S, Tristão Pereira C, Cordero-Grande L, Hughes EJ, Teixeira RPAG, et al. Neuroimaging findings in newborns with congenital heart disease prior to surgery: an observational study. Arch Dis Child. 2019;104:1042–8.
Wernovsky G, Licht DJ. Neurodevelopmental outcomes in children with congenital heart disease-what can we impact? Pediatr Crit Care Med. 2016;17:S232–42.
Louis D, Sundaram V, Kumar P. Pulse oximeter sensor application during neonatal resuscitation: a randomized controlled trial. Pediatrics. 2014;133:476–82.
Gandhi B, Rich W, Finer N. Time to achieve stable pulse oximetry values in VLBW infants in the delivery room. Resuscitation. 2013;84:970–3.
Baquero H, Alviz R, Castillo A, Neira F, Sola A. Avoiding hyperoxemia during neonatal resuscitation: time to response of different SpO2 monitors. Acta Paediatr. 2011;100:515–8.
Acknowledgements
We acknowledge members of the Children’s Hospital of Philadelphia Fetal Heart Program for assistance in accessing the Fetal Heart Registry for this study. We acknowledge Molly Passarella, MS, for her independent review of the statistical analyses.
Author information
Authors and Affiliations
Contributions
AT conceptualized the study design, collected and analyzed the data, and drafted the manuscript. AM refined the study collection tools, collected data, and reviewed and revised the manuscript. MH and DW analyzed the data, and reviewed and revised the manuscript. AA conceptualized the study design and reviewed and revised the manuscript. JR conceptualized the study design, analyzed the data, and reviewed and revised the manuscript. EF conceptualized the study design, refined the study collection tools, analyzed the data and reviewed and revised the manuscript. All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Prior presentation of study data: Accepted for presentation at Pediatric Academic Societies conference and Eastern Society for Pediatric Research in 2020 (presented virtually at ESPR in September 2020).
Supplementary information
Rights and permissions
About this article
Cite this article
Thomas, A.R., Ma, A.L., Weinberg, D.D. et al. Delivery room oxygen physiology and respiratory interventions for newborns with cyanotic congenital heart disease. J Perinatol 41, 2309–2316 (2021). https://doi.org/10.1038/s41372-021-01029-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41372-021-01029-2
This article is cited by
-
Call to action: prioritizing delivery room care for neonates with critical congenital heart disease
Journal of Perinatology (2024)