Abstract
Objective
To investigate the association between fluid balance during therapeutic hypothermia (TH) and severity of brain injury on magnetic resonance imaging (MRI) in neonates with hypoxic–ischemic encephalopathy (HIE).
Study design
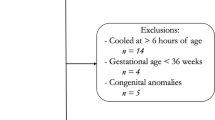
This is a secondary analysis of data from a prospective observational study in neonates with HIE. Daily net positive fluid balance during TH was investigated for association with the adverse primary outcome of death or moderate-to-severe brain injury on MRI using multivariable logistic regression.
Results
Of the 150 neonates included, 50 suffered adverse outcome and had significantly higher net positive fluid balance (53 vs. 19 ml/kg/day, p < 0.01) during first 24 hours of TH. Neonates with a net positive fluid balance (>25 ml/kg/day) at 24 hours of TH had 3.4 (95% CI 1.3–9) times higher odds of adverse outcome.
Conclusions
Positive fluid balance during TH in neonates with HIE is independently associated with death or moderate-to-severe brain injury on MRI.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Shankaran S, Laptook AR, Ehrenkranz RA, Tyson JE, McDonald SA, Donovan EF, et al. Whole-body hypothermia for neonates with hypoxic-ischemic encephalopathy. N. Engl J Med. 2005;353:1574–84.
Jacobs SE, Morley CJ, Inder TE, Stewart MJ, Smith KR, McNamara PJ, et al. Whole-body hypothermia for term and near-term newborns with hypoxic-ischemic encephalopathy: a randomized controlled trial. Arch Pediatr Adolesc Med. 2011;165:692–700.
Jacobs SE, Berg M, Hunt R, Tarnow-Mordi WO, Inder TE, Davis PG Cooling for newborns with hypoxic ischaemic encephalopathy. Cochrane Database Syst Rev. 2013; (1): CD003311.
Natarajan G, Pappas A, Shankaran S. Outcomes in childhood following therapeutic hypothermia for neonatal hypoxic-ischemic encephalopathy (HIE). Semin Perinatol. 2016;40:549–55.
Shankaran S, Natarajan G, Chalak L, Pappas A, McDonald SA, Laptook AR. Hypothermia for neonatal hypoxic-ischemic encephalopathy: NICHD neonatal research network contribution to the field. Semin Perinatol. 2016;40:385–90.
Azzopardi DV, Strohm B, Edwards AD, Dyet L, Halliday HL, Juszczak E, et al. Moderate hypothermia to treat perinatal asphyxial encephalopathy. N Engl J Med. 2009;361:1349–58.
Gluckman PD, Wyatt JS, Azzopardi D, Ballard R, Edwards AD, Ferriero DM, et al. Selective head cooling with mild systemic hypothermia after neonatal encephalopathy: multicentre randomised trial. Lancet 2005;365:663–70.
Azzopardi D. Clinical management of the baby with hypoxic ischaemic encephalopathy. Early Hum Dev. 2010;86:345–50.
Martinello K, Hart AR, Yap S, Mitra S, Robertson NJ. Management and investigation of neonatal encephalopathy: 2017. update Arch Dis Child Fetal Neonatal Ed. 2017;102:F346–58.
Stola A, Perlman J. Post-resuscitation strategies to avoid ongoing injury following intrapartum hypoxia-ischemia. Semin Fetal Neonatal Med. 2008;13:424–31.
Alobaidi R, Morgan C, Basu RK, Stenson E, Featherstone R, Majumdar SR, et al. Association between fluid balance and outcomes in critically ill children: a systematic review and meta-analysis. JAMA Pediatr. 2018;172:257–68.
Bhaskar P, Dhar AV, Thompson M, Quigley R, Modem V. Early fluid accumulation in children with shock and ICU mortality: a matched case-control study. Intensive Care Med. 2015;41:1445–53.
Li Y, Wang J, Bai Z, Chen J, Wang X, Pan J, et al. Early fluid overload is associated with acute kidney injury and PICU mortality in critically ill children. Eur J Pediatr. 2016;175:39–48.
Silva JM, de Oliveira AM, Nogueira FA, Vianna PM, Pereira Filho MC, Dias LF, et al. The effect of excess fluid balance on the mortality rate of surgical patients: a multicenter prospective study. Crit Care. 2013;17:R288.
Zhao Z, Wang D, Jia Y, Tian Y, Wang Y, Wei Y, et al. Analysis of the association of fluid balance and short-term outcome in traumatic brain injury. J Neurol Sci. 2016;364:12–18.
Selewski DT, Akcan-Arikan A, Bonachea EM, Gist KM, Goldstein SL, Hanna M, et al. The impact of fluid balance on outcomes in critically ill near-term/term neonates: a report from the AWAKEN study group. Pediatr Res. 2019;85:79–85.
Selewski DT, Cornell TT, Lombel RM, Blatt NB, Han YY, Mottes T, et al. Weight-based determination of fluid overload status and mortality in pediatric intensive care unit patients requiring continuous renal replacement therapy. Intensive Care Med. 2011;37:1166–73.
Barkovich AJ, Hajnal BL, Vigneron D, Sola A, Partridge JC, Allen F, et al. Prediction of neuromotor outcome in perinatal asphyxia: evaluation of MR scoring systems. AJNR Am J Neuroradiol. 1998;19:143–9.
Cheong JL, Coleman L, Hunt RW, Lee KJ, Doyle LW, Inder TE, et al. Prognostic utility of magnetic resonance imaging in neonatal hypoxic-ischemic encephalopathy: substudy of a randomized trial. Arch Pediatr Adolesc Med. 2012;166:634–40.
Sarnat HB, Sarnat MS. Neonatal encephalopathy following fetal distress. A clinical and electroencephalographic study. Arch Neurol. 1976;33:696–705.
Dell, KR. Fluid, electrolytes, and acid-base homeostasis. In: Martin RJ, Fanaroff AA, Walsh MC (eds). Fanaroff and martin’s neonatal-perinatal medicine, 9th edition: St. Louis, Missouri: Elsevier; 2011. p. 676.
Ultman JS. Computational model for insensible water loss from the newborn. Pediatrics 1987;79:760–65.
Kelleher MM, O’Carroll M, Gallagher A, Murray DM, Dunn Galvin A, Irvine AD, et al. Newborn transepidermal water loss values: a reference dataset. Pediatr Dermatol. 2013;30:712–16.
Lindower JB. Water balance in the fetus and neonate. Semin Fetal Neonatal Med. 2017;22:71–75.
Li AM, Chau V, Poskitt KJ, Sargent MA, Lupton BA, Hill A, et al. White matter injury in term newborns with neonatal encephalopathy. Pediatr Res. 2009;65:85–89.
Selewski DT, Charlton JR, Jetton JG, Guillet R, Mhanna MJ, Askenazi DJ, et al. Neonatal acute kidney injury. Pediatrics 2015;136:e463–73.
Natarajan G, Mathur A, Zaniletti I, DiGeronimo R, Lee KS, Rao R, et al. Withdrawal of life-support in neonatal hypoxic-ischemic encephalopathy. Pediatr Neurol. 2019;91:20–26.
Anderson JM, Belton NR. Water and electrolyte abnormalities in the human brain after severe intrapartum asphyxia. J Neurol Neurosurg Psychiatry. 1974;37:514–20.
Pryse-Davies J, Beard RW. A necropsy study of brain swelling in the newborn with special reference to cerebellar herniation. J Pathol. 1973;109:51–73.
Lupton BA, Hill A, Roland EH, Whitfield MF, Flodmark O. Brain swelling in the asphyxiated term newborn: pathogenesis and outcome. Pediatrics 1988;82:139–46.
Alaro D, Bashir A, Musoke R, Wanaiana L. Prevalence and outcomes of acute kidney injury in term neonates with perinatal asphyxia. Afr Health Sci. 2014;14:682–88.
Aggarwal A, Kumar P, Chowdhary G, Majumdar S, Narang A. Evaluation of renal functions in asphyxiated newborns. J Trop Pediatr. 2005;51:295–99.
Perlman JM, Tack ED. Renal injury in the asphyxiated newborn infant: relationship to neurologic outcome. J Pediatr. 1988;113:875–79.
Cavallin F, Rubin G, Vidal E, Cainelli E, Bonadies L, Suppiej A, et al. Prognostic role of acute kidney injury on long-term outcome in infants with hypoxic-ischemic encephalopathy. Pediatr Nephrol. 2020;35:477–83.
Kaplan SL, Feigin RD. Inappropriate secretion of antidiuretic hormone complicating neonatal hypoxic-ischemic encephalopathy. J Pediatr. 1978;92:431–33.
Kecskes Z, Healy G, Jensen A Fluid restriction for term infants with hypoxic-ischaemic encephalopathy following perinatal asphyxia. Cochrane Database Syst Rev. 2005; (3):CD004337.
Kochanek PM, Tasker RC, Bell MJ, Adelson PD, Carney N, Vavilala MS, et al. Management of pediatric severe traumatic brain injury: 2019 consensus and guidelines-based algorithm for first and second tier therapies. Pediatr Crit Care Med. 2019;20:269–79.
Rossi S, Picetti E, Zoerle T, Carbonara M, Zanier ER, Stocchetti N. Fluid management in acute brain injury. Curr Neurol Neurosci Rep. 2018;18:74.
van der Jagt M. Fluid management of the neurological patient: a concise review. Crit Care. 2016;20:126.
Shenkin HA, Bezier HS, Bouzarth WF. Restricted fluid intake. rational management of the neurosurgical patient. J Neurosurg. 1976;45:432–6.
Koskinen LO, Olivecrona M, Grände PO. Severe traumatic brain injury management and clinical outcome using the Lund concept. Neuroscience 2014;283:245–55.
Tanigasalam V, Plakkal N, Vishnu Bhat B, Chinnakali P. Does fluid restriction improve outcomes in infants with hypoxic ischemic encephalopathy? A pilot randomized controlled trial. J Perinatol. 2018;38:1512–7.
Montaldo P, Caredda E, Pugliese U, Zanfardino A, Delehaye C, Inserra E, et al. Continuous glucose monitoring profile during therapeutic hypothermia in encephalopathic infants with unfavorable outcome. Pediatr Res. 2020;88:218–24.
Basu SK, Kaiser JR, Guffey D, Minard CG, Guillet R, Gunn AJ, et al. Hypoglycaemia and hyperglycaemia are associated with unfavourable outcome in infants with hypoxic ischaemic encephalopathy: a post hoc analysis of the CoolCap Study. Arch Dis Child Fetal Neonatal Ed. 2016;101:F149–55.
Kasai M, Lear CA, Davidson JO, Beacom MJ, Drury PP, Maeda Y, et al. Early sinusoidal heart rate patterns and heart rate variability to assess hypoxia-ischaemia in near-term fetal sheep. J Physiol. 2019;597:5535–48.
Lear CA, Kasai M, Drury PP, Davidson JO, Miyagi E, Bennet L, et al. Plasma vasopressin levels are closely associated with fetal hypotension and neuronal injury after hypoxia-ischemia in near-term fetal sheep. Pediatr Res. 2020; e-pub ahead of print.
Summanen M, Bäck S, Voipio J, Kaila K. Surge of peripheral arginine vasopressin in a rat model of birth asphyxia. Front Cell Neurosci. 2018;12:2.
Ayus JC, Achinger SG, Arieff A. Brain cell volume regulation in hyponatremia: role of sex, age, vasopressin, and hypoxia. Am J Physiol Ren Physiol. 2008;295:F619–24.
Evers KS, Wellmann S. Arginine vasopressin and copeptin in perinatology. Front Pediatr. 2016;4:75.
Ayus JC, Armstrong D, Arieff AI. Hyponatremia with hypoxia: effects on brain adaptation, perfusion, and histology in rodents. Kidney Int. 2006;69:1319–25.
Durkan AM, Alexander RT. Acute kidney injury post neonatal asphyxia. J Pediatr. 2011;158:e29–33.
El-Gamasy MA, Alarabawy R. Relation of serum creatinine to sarnat scoring and brain computerized tomography of neonates with hypoxic ischemic encephalopathy. A single-center experience. J Pediatr Neurosci. 2018;13:437–42.
Gupta C, Massaro AN, Ray PE. A new approach to define acute kidney injury in term newborns with hypoxic ischemic encephalopathy. Pediatr Nephrol. 2016;31:1167–78.
Sarkar S, Askenazi DJ, Jordan BK, Bhagat I, Bapuraj JR, Dechert RE, et al. Relationship between acute kidney injury and brain MRI findings in asphyxiated newborns after therapeutic hypothermia. Pediatr Res. 2014;75:431–5.
Selewski DT, Jordan BK, Askenazi DJ, Dechert RE, Sarkar S. Acute kidney injury in asphyxiated newborns treated with therapeutic hypothermia. J Pediatr. 2013;162:725–9.
Acknowledgements
We thank the many technicians, nurses, physicians, and scientists at the Children’s National Hospital Neonatal Intensive Care Unit who contributed to the development and implementation of the original prospective study, and the families of participating infants.
Funding
This study was supported by the Clinical and Translational Science Institute at Children’s National (UL1TR000075, 1KL2RR031987-01) and the National Institutes of Health Intellectual and Developmental Disabilities Research Consortium (U54 HD090257).
Author information
Authors and Affiliations
Contributions
KMO conceptualized and designed the study, drafted the initial manuscript, and approved the final manuscript as submitted. SKB conceptualized and designed the study, performed statistical analysis, drafted the initial manuscript, and approved the final manuscript as submitted. MR conceptualized and designed the study, reviewed and revised the initial manuscript, and approved the final manuscript as submitted. SM and VG performed data collection, reviewed and revised the initial manuscript, and approved the final manuscript as submitted. GV performed the radiologic classification of MRIs according to the Barkovich criteria, reviewed and revised the initial manuscript, and approved the final manuscript as submitted. NH performed statistical analysis, summarized results, critically reviewed the manuscript, and approved the final manuscript as submitted. JB supervised statistical analysis, summarized results, critically reviewed the manuscript, and approved the final manuscript as submitted. TC conceptualized and designed the study, reviewed and revised the manuscript, and approved the final manuscript as submitted. ANM conceptualized and designed the study, supervised data analysis and interpretation, reviewed and revised the manuscript, and approved the final manuscript as submitted. All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no potential conflicts of interest to disclose. The contents of this article are solely the responsibility of the authors and do not necessarily represent the official views of the National Institutes of Health Intellectual and Developmental Disabilities Research Consortium or the United States Air Force.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ottolini, K.M., Basu, S.K., Herrera, N. et al. Positive fluid balance is associated with death and severity of brain injury in neonates with hypoxic–ischemic encephalopathy. J Perinatol 41, 1331–1338 (2021). https://doi.org/10.1038/s41372-021-00988-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41372-021-00988-w
This article is cited by
-
Comparative evaluation of approach to cardiovascular care in neonatal encephalopathy undergoing therapeutic hypothermia
Journal of Perinatology (2022)
-
Patterns of acute kidney and hepatic injury and association with adverse outcomes in infants undergoing therapeutic hypothermia for hypoxic ischemic encephalopathy
Journal of Perinatology (2022)