Abstract
Background
Prevalence of oral feeding difficulties in high-risk infants is increasing. Desire to take orally can be influenced by hunger and satiety, which may influence growth and body fat.
Objective
To determine the association between body adiposity and infant oral feeding.
Methods
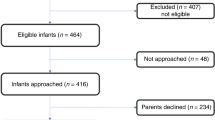
Retrospective case–control study of infants ≥37-week postmenstrual age (PMA). Infants on tube feeding (cases) compared to birth gestation-matched infants on full oral feeding (controls). Body composition was determined by air displacement plethysmography.
Results
Overall, 16 cases vs. 16 controls. At study, cases vs. controls had similar PMA, weight and length z-scores, and calorie intake. The mean oral intake was significantly less in cases vs. controls (66 vs. 168 ml/kg/day, p < 0.001). Cases had significantly higher percentage of fat mass (18.7 vs. 10.9) and fat-mass z-score (1.62 vs. 0.08) (p < 0.05), but similar fat-free mass vs. controls. Five case infants required gastrostomy.
Conclusions
Higher body adiposity may worsen the infant oral feeding outcomes.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
American Academy of Pediatrics Committee on Fetus and Newborn. Hospital discharge of the high-risk neonate. Pediatrics. 2008;122:1119–26.
Stoll BJ, Hansen NI, Bell EF, Walsh MC, Carlo WA, Shankaran S, et al. Trends in care practices, morbidity, and mortality of extremely preterm neonates, 1993-2012. JAMA. 2015;314:1039–51.
Horton J, Atwood C, Gnagi S, Teufel R, Clemmens C. Temporal trends of pediatric dysphagia in hospitalized patients. Dysphagia. 2018;33:655–61.
Hatch LD, Scott TA, Walsh WF, Goldin AB, Blakely ML, Patrick SW. National and regional trends in gastrostomy in very low birth weight infants in the USA: 2000-2012. J Perinatol. 2018;38:1270–6.
Jadcherla SR, Wang M, Vijayapal AS, Leuthner SR. Impact of prematurity and co-morbidities on feeding milestones in neonates: a retrospective study. J Perinatol. 2010;30:201–8.
Jadcherla SR, Khot T, Moore R, Malkar M, Gulati IK, Slaughter JL. Feeding methods at discharge predict long-term feeding and neurodevelopmental outcomes in preterm infants referred for gastrostomy evaluation. J Pediatr. 2017;181:125–130.e1.
Lainwala S, Kosyakova N, Power K, Hussain N, Moore JE, Hagadorn JI, et al. Delayed achievement of oral feedings is associated with adverse neurodevelopmental outcomes at 18 to 26 months follow-up in preterm infants. Am J Perinatol. 2020;37:483–90.
Walsh MC, Bell EF, Kandefer S, Saha S, Carlo WA, D’angio CT, et al. Neonatal outcomes of moderately preterm infants compared to extremely preterm infants. Pediatr Res. 2017;82:297–304.
Kitzmiller JL, Cloherty JP, Younger MD. Diabetic pregnancy and perinatal morbidity. Am J Obstet Gynecol. 1978;131:560–80.
Malkar MB, Viswanathan SK, Jadcherla SR. Pilot study of pharyngoesophageal dysmotility mechanisms in dysphagic infants of diabetic mothers. Am J Perinatol. 2019;36:1237–42.
Tolosa JN, Calhoun DA. Maternal and neonatal demographics of macrosomic infants admitted to the neonatal intensive care unit. J Perinatol. 2017;37:1292–6.
American Academy of Pediatrics. Pediatric Nutrition Handbook. 5th ed. Elk Grove Village, IL: American Academy of Pediatrics; 2004.
Fenton TR, Kim JH. A systematic review and meta-analysis to revise the Fenton growth chart for preterm infants. BMC Pediatr. 2013;13:59.
Johnson MJ, Wootton SA, Leaf AA, Jackson AA. Preterm birth and body composition at term equivalent age: a systematic review and meta-analysis. Pediatrics. 2012;130:e640–649.
Ramel SE, Gray HL, Ode KL, Younge N, Georgieff MK, Demerath EW. Body composition changes in preterm infants following hospital discharge: comparison with term infants. J Pediatr Gastroenterol Nutr. 2011;53:333–8.
Ramel SE, Demerath EW, Gray HL, Younge N, Boys C, Georgieff MK. The relationship of poor linear growth velocity with neonatal illness and two-year neurodevelopment in preterm infants. Neonatology. 2012;102:19–24.
Sewell MF, Huston-Presley L, Super DM, Catalano P. Increased neonatal fat mass, not lean body mass, is associated with maternal obesity. Am J Obstet Gynecol. 2006;195:1100–3.
Kara M, Orbak Z, Döneray H, Ozkan B, Akcay F. The relationship between skinfold thickness and leptin, ghrelin, adiponectin, and resistin levels in infants of diabetic mothers. Fetal Pediatr Pathol. 2017;36:1–7.
Logan KM, Gale C, Hyde MJ, Santhakumaran S, Modi N. Diabetes in pregnancy and infant adiposity: systematic review and meta-analysis. Arch Dis Child Fetal Neonatal Ed. 2017;102:F65–72.
Klok MD, Jakobsdottir S, Drent ML. The role of leptin and ghrelin in the regulation of food intake and body weight in humans: a review. Obes Rev. 2007;8:21–34.
Wren AM, Seal LJ, Cohen MA, Brynes AE, Frost GS, Murphy KG, et al. Ghrelin enhances appetite and increases food intake in humans. J Clin Endocrinol Metab. 2001;86:5992.
Nagel E, Hickey M, Teigen L, Kuchnia A, Curran K, Soumekh L, et al. Clinical Application of body composition methods in premature infants. J Parenter Enteral Nutr. 2020.
Norris T, Ramel SE, Catalano P, Caoimh CN, Roggero P, Murray D, et al. New charts for the assessment of body composition, according to air-displacement plethysmography, at birth and across the first 6 mo of life. Am J Clin Nutr. 2019;109:1353–60.
Austin J, Marks D. Hormonal regulators of appetite. Int J Pediatr Endocrinol. 2009;2009:141753.
Shekhawat PS, Garland JS, Shivpuri C, Mick GJ, Sasidharan P, Pelz CJ, et al. Neonatal cord blood leptin: its relationship to birth weight, body mass index, maternal diabetes, and steroids. Pediatr Res. 1998;43:338–43.
Tapanainen P, Leinonen E, Ruokonen A, Knip M. Leptin concentrations are elevated in newborn infants of diabetic mothers. Horm Res. 2001;55:185–90.
Katsuki A, Urakawa H, Gabazza EC, Murashima S, Nakatani K, Togashi K, et al. Circulating levels of active ghrelin is associated with abdominal adiposity, hyperinsulinemia and insulin resistance in patients with type 2 diabetes mellitus. Eur J Endocrinol. 2004;151:573–7.
Stylianou C, Galli-Tsinopoulou A, Farmakiotis D, Rousso I, Karamouzis M, Koliakos G, et al. Ghrelin and leptin levels in obese adolescents. Relationship with body fat and insulin resistance. Hormones. 2007;6:295–303.
Pfister KM, Gray HL, Miller NC, Demerath EW, Georgieff MK, Ramel SE. Exploratory study of the relationship of fat-free mass to speed of brain processing in preterm infants. Pediatr Res. 2013;74:576–83.
Ramel SE, Gray HL, Christiansen E, Boys C, Georgieff MK, Demerath EW. Greater early gains in fat-free mass, but not fat mass, are associated with improved neurodevelopment at 1 year corrected age for prematurity in very low birth weight preterm infants. J Pediatr. 2016;173:108–15.
Cauble JS, Dewi M, Hull HR. Validity of anthropometric equations to estimate infant fat mass at birth and in early infancy. BMC Pediatr. 2017;17:88.
Olhager E, Forsum E. Assessment of total body fat using the skinfold technique in full-term and preterm infants. Acta Paediatr. 2006;95:21–28.
Deierlein AL, Thornton J, Hull H, Paley C, Gallagher D. An anthropometric model to estimate neonatal fat mass using air displacement plethysmography. Nutr Metab. 2012;9:21.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
SV is the guarantor of the article. All authors declare no potential competing conflicts of interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Viswanathan, S., Osborn, E. & Jadcherla, S. Body adiposity and oral feeding outcomes in infants: a pilot study. J Perinatol 41, 1059–1064 (2021). https://doi.org/10.1038/s41372-021-00975-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41372-021-00975-1