Abstract
Objective
To examine the relationship between intestinal perforations (caused by either spontaneous perforation (SIP) or necrotizing enterocolitis (NEC)) and the outcome “death due to intestinal perforation”.
Methods
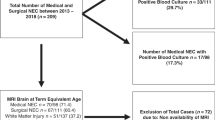
Multivariable logistic regression analyses were used to compare infants <28 weeks’ gestation with SIP (n = 32) and perforated-NEC (n = 45) for the outcome perforation-related death.
Results
In univariate analyses the incidence of death due to perforation was higher among infants with perforated-NEC (36%) than infants with SIP (13%). However, infants with perforated-NEC were more likely to be older than 10 days and have bacteremia/fungemia with non-coagulase-negative staphylococci (non-CONS) organisms than infants with SIP. After adjusting for confounding the only variable that was significantly associated with mortality due to perforation was the presence of non-CONS bacteremia/fungemia at the onset of perforation.
Conclusions
The apparent association between death and perforated-NEC could be explained by the higher incidence of non-CONS bacteremia/fungemia among infants with perforated-NEC.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
Data availability
The datasets generated and/or analysed during the current study are available from the corresponding author on reasonable request.
References
Bizzarro MJ, Ehrenkranz RA, Gallagher PG. Concurrent bloodstream infections in infants with necrotizing enterocolitis. J Pediatr. 2014;164:61–66.
Shah J, Singhal N, da Silva O, Rouvinez-Bouali N, Seshia M, Lee SK, et al. Intestinal perforation in very preterm neonates: risk factors and outcomes. J Perinatol. 2015;35:595–600.
Najaf TA, Vachharajani NA, Warner BW, Vachharajani AJ. Interval between clinical presentation of necrotizing enterocolitis and bowel perforation in neonates. Pediatr Surg Int. 2010;26:607–9.
Caplan MS, Fanaroff A. Necrotizing: a historical perspective. Semin Perinatol. 2017;41:2–6.
Hackam D, Caplan M. Necrotizing enterocolitis: pathophysiology from a historical context. Semin Pediatr Surg. 2018;27:11–18.
Pumberger W, Mayr M, Kohlhauser C, Weninger M. Spontaneous localized intestinal perforation in very-low-birth-weight infants: a distinct clinical entity different from necrotizing enterocolitis. J Am Coll Surg. 2002;195:796–803.
Gordon PV. Understanding intestinal vulnerability to perforation in the extremely low birth weight infant. Pediatr Res. 2009;65:138–44.
Lai S, Yu W, Wallace L, Sigalet D. Intestinal muscularis propria increases in thickness with corrected gestational age and is focally attenuated in patients with isolated intestinal perforations. J Pediatr Surg. 2014;49:114–9.
Gordon PV, Swanson JR, Attridge JT, Clark R. Emerging trends in acquired neonatal intestinal disease: is it time to abandon Bell’s criteria? J Perinatol. 2007;27:661–71.
Blakely ML, Lally KP, McDonald S, Brown RL, Barnhart DC, Ricketts RR, et al. Postoperative outcomes of extremely low birth-weight infants with necrotizing enterocolitis or isolated intestinal perforation: a prospective cohort study by the NICHD Neonatal Research Network. Ann Surg. 2005;241:984–9. discussion 989-94
Hintz SR, Kendrick DE, Stoll BJ, Vohr BR, Fanaroff AA, Donovan EF, et al. Neurodevelopmental and growth outcomes of extremely low birth weight infants after necrotizing enterocolitis. Pediatrics. 2005;115:696–703.
Fisher JG, Jones BA, Gutierrez IM, Hull MA, Kang KH, Kenny M, et al. Mortality associated with laparotomy-confirmed neonatal spontaneous intestinal perforation: a prospective 5-year multicenter analysis. J Pediatr Surg. 2014;49:1215–9.
Stone HH, Kolb LD, Geheber CE. Bacteriologic considerations in perforated necrotizing enterocolitis. South Med J. 1979;72:1540–4.
Kliegman RM, Fanaroff AA. Neonatal necrotizing enterocolitis: a nine-year experience. II. Outcome assessment. Am J Dis Child. 1981;135:608–11.
Palmer SR, Biffin A, Gamsu HR. Outcome of neonatal necrotising enterocolitis: results of the BAPM/CDSC surveillance study, 1981-84. Arch Dis Child. 1989;64:388–94.
Heida FH, Hulscher JB, Schurink M, van Vliet MJ, Kooi EM, Kasper DC, et al. Bloodstream infections during the onset of necrotizing enterocolitis and their relation with the pro-inflammatory response, gut wall integrity and severity of disease in NEC. J Pediatr Surg. 2015;50:1837–41.
Elfvin A, Dinsdale E, Wales PW, Moore AM. Low birthweight, gestational age, need for surgical intervention and gram-negative bacteraemia predict intestinal failure following necrotising enterocolitis. Acta Paediatr. 2015;104:771–6.
Mollitt DL, Tepas JJ 3rd, Talbert JL. The microbiology of neonatal peritonitis. Arch Surg. 1988;123:176–9.
La Rosa PS, Warner BB, Zhou Y, Weinstock GM, Sodergren E, Hall-Moore CM, et al. Patterned progression of bacterial populations in the premature infant gut. Proc Natl Acad Sci USA. 2014;111:12522–7.
Rusconi B, Good M, Warner BB. The microbiome and biomarkers for necrotizing enterocolitis: are we any closer to prediction? J Pediatr. 2017;189:40–47 e42.
Jacquot A, Neveu D, Aujoulat F, Mercier G, Marchandin H, Jumas-Bilak E, et al. Dynamics and clinical evolution of bacterial gut microflora in extremely premature patients. J Pediatr. 2011;158:390–6.
Normann E, Fahlen A, Engstrand L, Lilja HE. Intestinal microbial profiles in extremely preterm infants with and without necrotizing enterocolitis. Acta Paediatr. 2013;102:129–36.
Sim K, Shaw AG, Randell P, Cox MJ, McClure ZE, Li MS, et al. Dysbiosis anticipating necrotizing enterocolitis in very premature infants. Clin Infect Dis. 2015;60:389–97.
Torrazza RM, Ukhanova M, Wang X, Sharma R, Hudak ML, Neu J, et al. Intestinal microbial ecology and environmental factors affecting necrotizing enterocolitis. PLoS One. 2013;8:e83304.
Zhou Y, Shan G, Sodergren E, Weinstock G, Walker WA, Gregory KE. Longitudinal analysis of the premature infant intestinal microbiome prior to necrotizing enterocolitis: a case-control study. PLoS ONE. 2015;10:e0118632.
Liebowitz M, Clyman RI. Prophylactic indomethacin compared with delayed conservative management of the patent ductus arteriosus in extremely preterm infants: effects on neonatal outcomes. J Pediatr. 2017;187:119–26.
Clyman RI, Wickremasinghe A, Merritt TA, Solomon T, McNamara P, Jain A, et al. Hypotension following patent ductus arteriosus ligation: the role of adrenal hormones. J Pediatr. 2014;164:1449–55.
Liebowitz MC, Clyman RI. Predicting the need for home oxygen therapy in preterm infants born before 28 weeks’ gestation. Am J Perinatol. 2016;33:34–39.
Rao SC, Basani L, Simmer K, Samnakay N, Deshpande G. Peritoneal drainage versus laparotomy as initial surgical treatment for perforated necrotizing enterocolitis or spontaneous intestinal perforation in preterm low birth weight infants. Cochrane Datab. Syst. Rev. 2011;CD006182. https://doi.org/10.1002/14651858.CD006182.pub2.
Caplan MS, Underwood MA, Modi N, Patel R, Gordon PV, Sylvester KG, et al. Necrotizing enterocolitis: using regulatory science and drug development to improve outcomes. J Pediatr. 2019;212:208–215 e201.
Hartel C, Hartz A, Pagel J, Rupp J, Stein A, Kribs A, et al. NOD2 loss-of-function mutations and risks of necrotizing enterocolitis or focal intestinal perforation in very low-birth-weight infants. Inflamm Bowel Dis. 2016;22:249–56.
Neu J, Pammi M. Pathogenesis of NEC: impact of an altered intestinal microbiome. Semin Perinatol. 2017;41:29–35.
Stewart CJ, Fatemizadeh R, Parsons P, Lamb CA, Shady DA, Petrosino JF, et al. Using formalin fixed paraffin embedded tissue to characterize the preterm gut microbiota in necrotising enterocolitis and spontaneous isolated perforation using marginal and diseased tissue. BMC Microbiol. 2019;19:52.
Warner BB, Deych E, Zhou Y, Hall-Moore C, Weinstock GM, Sodergren E, et al. Gut bacteria dysbiosis and necrotising enterocolitis in very low birthweight infants: a prospective case-control study. Lancet. 2016;387:1928–36.
Funding
This work was supported by grant from the U.S. Public Health Service National Heart, Lung and Blood Institute (HL109199) and a gift from the Jamie and Bobby Gates Foundation.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
We have no conflict of interests. None of the authors have any potential conflict of interest, real or perceived; None of the authors have any financial agreement with any company whose product figures prominently in the manuscript. There are no “sponsors” of this project. And there are no “sponsors” who have had a role in (1) study design; (2) the collection, analysis, and interpretation of data; (3) the writing of the report; and (4) the decision to submit the paper for publication. RIC wrote the first draft of the manuscript and no honorarium, grant, or other form of payment was given to anyone to produce the manuscript.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Clyman, R.I., Jin, C. & Hills, N.K. A role for neonatal bacteremia in deaths due to intestinal perforation: spontaneous intestinal perforation compared with perforated necrotizing enterocolitis. J Perinatol 40, 1662–1670 (2020). https://doi.org/10.1038/s41372-020-0691-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41372-020-0691-4
This article is cited by
-
Wide use of broad-spectrum antibiotics in very low birth weight infants with spontaneous focal intestinal perforation—is it really justified?
Infection (2024)
-
Prophylactic indomethacin, antenatal betamethasone, and the risk of intestinal perforation in infants <28 weeks’ gestation
Journal of Perinatology (2023)
-
Prophylactic efficacy of enteral antifungal administration of miconazole for intestinal perforation, especially for necrotizing enterocolitis: a historical cohort study at a single institution
Surgery Today (2021)