Abstract
Objective
Investigate relevance of diastolic flow abnormalities in celiac trunk (aCT) and middle cerebral artery (aMCA) among preterms with persistent hemodynamically significant patent ductus arteriosus (phsPDA, diameter ≥ 1.5 mm, and age ≥ 7 days).
Study design
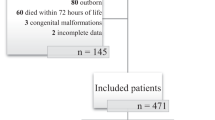
Five hundred fifteen echocardiograms from 156 neonates born <28 weeks gestation age (GA) were analyzed retrospectively. Infants with aCT or aMCA at any time were compared with the rest. Separate comparisons were performed for aCT and aMCA. Primary outcome was composite of death, chronic lung disease (CLD), or necrotizing enterocolitis ≥ stage 2. Logistic regression was used to adjust for confounders.
Result
Mean (SD) weight and GA were 820(214) g and 25.2(1.3) weeks. aMCA, but not aCT, was associated with primary outcome [adjusted odds ratio 2.17, 95% CI: 1.01–4.67] and CLD [2.20 (0.99–4.87)].
Conclusion
aMCA may be a valid marker for defining the clinical significance of phsPDA in preterm neonates. aCeT may be of limited value in selecting patients for treatment.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Zonnenberg I, de Waal K. The definition of a haemodynamic significant duct in randomized controlled trials: a systematic literature review. Acta Paediatr. 2012;101:247–51.
Sehgal A, McNamara PJ. Does echocardiography facilitate determination of hemodynamic significance attributable to the ductus arteriosus? Eur J Pediatr. 2009;168:907–14.
Kluckow M, Evans N. Early echocardiographic prediction of symptomatic patent ductus arteriosus in preterm infants undergoing mechanical ventilation. J Pediatr. 1995;127:774–9.
El-Khuffash A, James AT, Corcoran JD, Dicker P, Franklin O, Elsayed YN, et al. A patent ductus arteriosus severity score predicts chronic lung disease or death before discharge. J Pediatr. 2015;167:1354–61.e2.
Sehgal A, Paul E, Menahem S. Functional echocardiography in staging for ductal disease severity: role in predicting outcomes. Eur J Pediatr. 2013;172:179–84.
Carlo WF, Kimball TR, Michelfelder EC, Border WL. Persistent diastolic flow reversal in abdominal aortic Doppler-flow profiles is associated with an increased risk of necrotizing enterocolitis in term infants with congenital heart disease. Pediatrics 2007;119:330–5.
Coombs RC, Morgan ME, Durbin GM, Booth IW, McNeish AS. Gut blood flow velocities in the newborn: effects of patent ductus arteriosus and parenteral indomethacin. Arch Dis Child. 1990;65:1067–71.
Shimada S, Kasai T, Konishi M, Fujiwara T. Effects of patent ductus arteriosus on left ventricular output and organ blood flows in preterm infants with respiratory distress syndrome treated with surfactant. J Pediatr. 1994;125:270–7.
El-Khuffash A, Higgins M, Walsh K, Molloy EJ. Quantitative assessment of the degree of ductal steal using celiac artery blood flow to left ventricular output ratio in preterm infants. Neonatology. 2008;93:206–12.
Perlman JM, Hill A, Volpe JJ. The effect of patent ductus arteriosus on flow velocity in the anterior cerebral arteries: ductal steal in the premature newborn infant. J Pediatr. 1981;99:767–71.
Weir FJ, Ohlsson A, Myhr TL, Fong K, Ryan ML. A patent ductus arteriosus is associated with reduced middle cerebral artery blood flow velocity. Eur J Pediatr. 1999;158:484–7.
Hsu KH, Nguyen J, Dekom S, Ramanathan R, Noori S. Effects of patent ductus arteriosus on organ blood flow in infants born very preterm: a prospective study with serial echocardiography. J Pediatr. 2020;216:95–100.e2.
Lee SK, McMillan DD, Ohlsson A, Pendray M, Synnes A, Whyte R, et al. Variations in practice and outcomes in the Canadian NICU network: 1996–1997. Pediatrics 2000;106:1070–9.
Shah PS, Seidlitz W, Chan P, Yeh S, Musrap N, Lee SK, et al. Internal audit of the canadian neonatal network data collection system. Am J Perinatol. 2017;34:1241–9.
Lipman B, Serwer GA, Brazy JE. Abnormal cerebral hemodynamics in preterm infants with patent ductus arteriosus. Pediatrics. 1982;69:778–81.
Shortland DB, Gibson NA, Levene MI, Archer LN, Evans DH, Shaw DE. Patent ductus arteriosus and cerebral circulation in preterm infants. Dev Med Child Neurol. 1990;32:386–93.
Martin CG, Snider AR, Katz SM, Peabody JL, Brady JP. Abnormal cerebral blood flow patterns in preterm infants with a large patent ductus arteriosus. J Pediatr. 1982;101:587–93.
Wong SN, Lo RN, Hui PW. Abnormal renal and splanchnic arterial Doppler pattern in premature babies with symptomatic patent ductus arteriosus. J Ultrasound Med. 1990;9:125–30.
Hoodbhoy SA, Cutting HA, Seddon JA, Campbell ME. Cerebral and splanchnic hemodynamics after duct ligation in very low birth weight infants. J Pediatr. 2009;154:196–200.
Jim WT, Chiu NC, Chen MR, Hung HY, Kao HA, Hsu CH, et al. Cerebral hemodynamic change and intraventricular hemorrhage in very low birth weight infants with patent ductus arteriosus. Ultrasound Med Biol. 2005;31:197–202.
Schena F, Francescato G, Cappelleri A, Picciolli I, Mayer A, Mosca F, et al. Association between hemodynamically significant patent ductus arteriosus and Bronchopulmonary Dysplasia. J Pediatr. 2015;166:1488–92.
Broadhouse KM, Price AN, Durighel G, Cox DJ, Finnemore AE, Edwards AD, et al. Assessment of PDA shunt and systemic blood flow in newborns using cardiac MRI. NMR Biomed. 2013;26:1135–41.
Louis D, Mukhopadhyay K, Sodhi KS, Jain V, Kumar P. Superior mesenteric artery Doppler is poor at predicting feed intolerance and NEC in preterm small for gestational age neonates. J Matern Fetal Neonatal Med. 2013;26:1855–9.
Clyman R, Wickremasinghe A, Jhaveri N, Hassinger DC, Attridge JT, Sanocka U, et al. Enteral feeding during indomethacin and ibuprofen treatment of a patent ductus arteriosus. J Pediatr. 2013;163:406–11.
Sellmer A, Bjerre JV, Schmidt MR, McNamara PJ, Hjortdal VE, Host B, et al. Morbidity and mortality in preterm neonates with patent ductus arteriosus on day 3. Arch Dis Child Fetal Neonatal Ed. 2013;98:F505–10.
Benitz WE. Learning to live with patency of the ductus arteriosus in preterm infants. J Perinatol. 2011;31:S42–8.
Acknowledgements
We would like to acknowledge the contribution of Mr Junmin Yang Msc, Statistician, MiCare Research Center, Mount Sinai Hospital, University of Toronto for conducting the statistical analysis for this study and the Canadian Neonatal Network for providing the demographic and clinical outcome data of study infants.
Author information
Authors and Affiliations
Contributions
AJ drafted the research question, AJ and DEW designed the study design and concept, PD, LM, PS, and PJM reviewed and made significant intellectual contribution to the research design. LK, PD, and JP also contributed to research methodology and acquired the study data and prepared files for analysis. AJ, LM, and PS also contributed resources toward the conduct and completion of this project. All authors made significant contribution to the interpretation of the results. AJ and DEW prepared the initial draft of the paper, while PD, LK, JP, LM, PS, and PJM reviewed the paper and provided significant critical revisions. All authors approved the final paper and accept responsibility for all elements of this paper.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Keusters, L., Purna, J., Deshpande, P. et al. Clinical validity of systemic arterial steal among extremely preterm infants with persistent patent ductus arteriosus. J Perinatol 41, 84–92 (2021). https://doi.org/10.1038/s41372-020-0663-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41372-020-0663-8
This article is cited by
-
Morbidity associated with patent ductus arteriosus in preterm newborns: a retrospective case-control study
Italian Journal of Pediatrics (2021)
-
The often forgotten systemic effects of ductus arteriosus: impact on decision-making and future trials
Journal of Perinatology (2021)