Abstract
Background
Mortality and ECMO rates for congenital diaphragmatic hernia (CDH) remain ~30%. In 2016, we changed our CDH guidelines to minimize stimulation while relying on preductal oxygen saturation, lower mean airway pressures, stricter criteria for nitric oxide (iNO), and inotrope use. We compared rates of ECMO, survival, and survival without ECMO between the two epochs.
Design/Methods
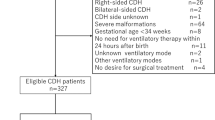
Retrospective review of left-sided CDH neonates at the University of Utah/Primary Children’s Hospital NICUs during pre (2003–2015, n = 163) and post (2016–2019, n = 53) epochs was conducted. Regression analysis controlled for defect size and intra-thoracic liver.
Results
Following guideline changes, we identified a decrease in ECMO (37 to 13%; p = 0.001) and an increase in survival without ECMO (53 to 79%, p = 0.0001). Overall survival increased from 74 to 89% (p = 0.035).
Conclusion(s)
CDH management guideline changes focusing on minimizing stimulation, using preductal saturation and less aggressive ventilator/inotrope support were associated with decreased ECMO use and improved survival.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Ameis D, Khoshgoo N, Keijzer R. Abnormal lung development in congenital diaphragmatic hernia. Semin Pediatr Surg. 2017;26:123–8.
Chandrasekharan PK, Rawat M, Madappa R, Rothstein DH, Lakshminrusimha S. Congenital diaphragmatic hernia - a review. Matern Health Neonatol Perinatol. 2017;11:6.
Mohseni-Bod H, Bohn D. Pulmonary hypertension in congenital diaphragmatic hernia. Sem Pediatr Surg. 2007;16:126–33.
Lally KP. Congenital diaphragmatic hernia—the past 25 (or so) years. J Pediatr Surg. 2016;51:695–8.
Haroon J, Chamberlain RS. An evidence-based review of the current treatment of congenital diaphragmatic hernia. Clin Pediatr. 2013;52:115–24.
Pugliandla PA, Grabowski J, Austin M, Hedrick H, Renaud E, Arnold M, et al. Management of congenital diaphragmatic hernia: A systematic review from the APSA outcomes and evidence based practice committee. J Pediatr Surg. 2015;50:1958–70.
Snoek KG, Reiss IK, Greenough A, Capolupo I, Urlesberger B, Wessel L. for CDH EURO Consortium. et al. Standardized postnatal management of infants with congenital diaphragmatic hernia in Europe: The CDH EURO Consortium Consensus—2015 Update. Neonatology. 2016;110:66–74.
The Canadian Congenital Diaphragmatic Hernia Collaborative. Diagnosis and management of congenital diaphragmatic hernia: a clinical practice guideline. CMAJ. 2018;190:E103–112.
Wung JT, Sahni R, Moffitt ST, Lipsitz E, Stolar CJ. Congenital diaphragmatic hernia: survival treated with very delayed surgery, spontaneous respiration, and no chest tube. J Pediatr Surg. 1995;30:406–9.
Lally KP, Lasky RE, Lally PA, Bagolan P, Davis CF, Frenckner BP. The Congenital Diaphragmatic Hernia Study Group. et al. Standardized reporting for congenital diaphragmatic hernia—an international consensus. J Pediatr Surg. 2013;48:2408–15.
Snoek KG, Capolupo I, van Rosmalen J, Hout Lde J, Vijfhuize S, Greenough A.for the CDH EURO Consortium. et al. Conventional mechanical ventilation versus high-frequency oscillatory ventilation for congenital diaphragmatic hernia: a randomized clinical trial (The VICI-trial). Ann Surg. 2016;263:867–74.
Courtney SE, Durand DJ, Asselin JM, Hudak ML, Aschner JL, Shoemaker CT, Neonatal Ventilation Study Group. High-frequency oscillatory ventilation versus conventional mechanical ventilation for very-low-birth-weight infants. N. Engl J Med. 2002;347:643–52.
Johnson AH, Peacock JL, Greenough A, Marlow N, Limb ES, Marston L. United Kingdom Oscillation Study Group. et al. High-frequency oscillatory ventilation for the prevention of chronic lung disease of prematurity. N. Engl J Med. 2002;347:633–42.
Muhlethaler V, Malcolm G. Mechanical ventilation in the newborn; a simplified approach. Part 2: High-frequency ventilation. J Paediatr Child Health. 2014;50:E10–3.
Dargaville PA, Tingay DG. Lung protective ventilation in extremely preterm infants. J Paediatr Child Health. 2012;48:740–6.
Fougeres E, Teboul J-L, Richard C, Osman D, Chemla D, Monnet X. Hemodynamic impact of a positive end-expiratory pressure setting in acute respiratory distress syndrome: importance of the volume status. Crit Care Med. 2010;38:802–7.
Guevorkian D, Mur S, Cavatorta E, Pognon L, Rakza T, Storme L. Lower distending pressure improves respiratory mechanics in congenital diaphragmatic hernia complicated by persistent pulmonary hypertension. J Pediatr. 2018;200:38–43.
Saugstad OD, Sejersted Y, Solberg R, Wollen EJ, Bjoras M. Oxygenation of the newborn: a molecular approach. Neonatology. 2012;101:315–25.
Perrone S, Bracciali C, Di Virgilio N, Buonocore G. Oxygen use in neonatal care: a two-edged sword. Front Pediatr. 2017;4:143.
Lakshminrusimha S, Russell JA, Steinhorn RH, Swartz DD, Ryan RM, Gugino SF, et al. Pulmonary hemodynamics in neonatal lambs resuscitated with 21%, 50%, and 100% oxygen. Pediatr Res. 2007;62:313–8.
Lakshminrusimha S, Swartz DD, Gugino SF, Ma CX, Wynn KA, Ryan RM, et al. Oxygen concentration and pulmonary hemodynamics in newborn lambs with pulmonary hypertension. Pediatr Res. 2009;66:539–44.
Jancelewicz T, Brindle ME, Guner YS, Lally PA, Lally KP, Harting MT.for the Congenital Diaphragmatic Hernia Study Group (CDHSG) and Pediatric Surgery Research Collaborative (PedSRC). Toward standardized management of congenital diaphragmatic hernia: an analysis of practice guidelines. J Surg Res. 2019;243:229–35.
Riley JS, Antiel RM, Rintoul NE, Ades AM, Waqar LN, Lin N, et al. Reduced oxygen concentration for the resuscitation of infants with congenital diaphragmatic hernia. J Perinatol. 2018;38:834–43.
Gien J, Kinsella JP. Differences in preductal and postductal arterial blood gas measurements in infants with severe congenital diaphragmatic hernia. Arch Dis Child Fetal Neonatal Ed. 2016;101:F314–318.
Moffitt ST, Schulze KF, Sahni R, Wung J-T, Myers MM, Stolar CJ. Preoperative cardiorespiratory trends in infants with congenital diaphragmatic hernia. J Pediatr Surg. 1995;130:604–11.
Tan Y-W, Adamson L, Forster C, Davies B, Sharkey D. Using serial oxygenation index as an objective predictor of survival for antenatally diagnosed congenital diaphragmatic hernia. J Pediatr Surg. 2012;47:1984–9.
Tan Y-W, Ali K, Andradi G, Sasidharan L, Greenough A, Davenport M. Prognostic value of the oxygenation index to predict survival and timing of surgery in infants with congenital diaphragmatic hernia. J Pediatr Surg. 2019;54:1567–72.
Lakshminrusimha S. The pulmonary circulation in neonatal respiratory failure. Clin Perinatol. 2012;39:655–83.
Tourneux P, Rakza T, Bouissou A, Krim G, Storme L. Pulmonary circulatory effects of norepinephrine in newborn infants with persistent pulmonary hypertension. J Pediatr. 2008;153:345–9.
Schwartz SM, Vermilion RP, Hirschl RB. Evaluation of left ventricular mass in children with left-sided congenital diaphragmatic hernia. J Pediatr. 1994;125:447–51.
Karpuz D, Giray D, Celik Y, Hallioglu O. Prognostic markers in congenital diaphragmatic hernia: Left ventricular diameter and pulmonary hypertension. Pediatr Int. 2018;60:122–6.
Altit G, Bhombal S, Van Meurs K, Tacy TA. Diminished cardiac performance and left ventricular dimensions in neonates with congenital diaphragmatic hernia. Pediatr Cardiol. 2018;39:993–1000.
Patel N, Lally PA, Kipfmueller F, Massolo AC, Luco M, Van Meurs KP, et al. Congenital Diaphragmatic Hernia Study Group. Ventricular dysfunction is a critical determinant of mortality in congenital diaphragmatic hernia. Am J Respir Crit Care Med. 2019;200:1522–30.
Kinsella JP, Steinhorn RH, Mullen MP, Hopper RK, Keller RL, Ivy DD, Pediatric Pulmonary Hypertension Network (PPHNet). et al. The left ventricle in congenital diaphragmatic hernia: implications for the management of pulmonary hypertension. J Pediatr. 2018;197:17–22.
Moenkemeyer F, Patel N. Right ventricular diastolic function measured by tissue Doppler imaging predicts early outcome in congenital diaphragmatic hernia. Pediatr Crit Care Med. 2014;15:49–55.
Denney S, Howley LW, Hodges M, Liechty KW, Marwan AI, Gien J, et al. Impact of objective echocardiographic criteria for timing of congenital diaphragmatic hernia repair. J Pediatr. 2018;192:99–104.e4.
Lakshminrusimha S, Keszler M, Kirpalani H, Van Meurs K, Chess P, Ambalavanan N, et al. Milrinone in congenital diaphragmatic hernia—a randomized pilot trial: study protocol, review of literature and survey of current practices. Matern Health Neonatol Perinatol. 2017;3:27.
Shanmugam H, Brunelli L, Botto LD, Krikov S, Feldkamp ML. Epidemiology and prognosis of congenital diaphragmatic hernia: a population-based cohort study in Utah. Birth Defects Res. 2017;109:1451–9.
Author information
Authors and Affiliations
Contributions
No outside honorarium, grant, or other form of payment was provided to anyone to produce the manuscript. MJY and BAY contributed to the conception and design of the study, data collection and analysis, and manuscript preparation; SF, KR, and CCY contributed to conception and design as well as manuscript preparation. All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Yang, M.J., Fenton, S., Russell, K. et al. Left-sided congenital diaphragmatic hernia: can we improve survival while decreasing ECMO?. J Perinatol 40, 935–942 (2020). https://doi.org/10.1038/s41372-020-0615-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41372-020-0615-3
This article is cited by
-
Congenital diaphragmatic hernia: quality improvement using a maximal lung protection strategy and early surgery-improved survival
European Journal of Pediatrics (2023)
-
High-frequency oscillatory ventilation versus conventional ventilation in the respiratory management of term neonates with a congenital diaphragmatic hernia: a retrospective cohort study
European Journal of Pediatrics (2022)