Abstract
Objective
To determine the associations between age at first postnatal corticosteroids (PNS) exposure and risk for severe bronchopulmonary dysplasia (BPD) and neurodevelopmental impairment (NDI).
Study design
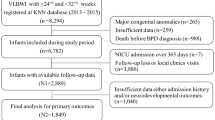
Cohort study of 951 infants born <27 weeks gestational age at NICHD Neonatal Research Network sites who received PNS between 8 days of life (DOL) and 36 weeks’ postmenstrual age was used to produce adjusted odds ratios (aOR).
Results
Compared with infants in the reference group (22–28 DOL-lowest rate), aOR for severe BPD was similar for children given PNS between DOL 8 and 49 but higher among infants treated at DOL 50–63 (aOR 1.77, 95% CI 1.03–3.06), and at DOL ≥64 (aOR 3.06, 95% CI 1.44–6.48). The aOR for NDI did not vary significantly by age of PNS exposure.
Conclusion
For infants at high risk of BPD, initial PNS should be considered prior to 50 DOL for the lowest associated odds of severe BPD.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
Data availability
Data reported in this paper may be requested through a data use agreement. Further details are available at https://neonatal.rti.org/index.cfm?fuseaction=DataRequest.Home.
References
Stoll BJ, Hansen NI, Bell EF, Walsh MC, Carlo WA, Shankaran S, et al. Trends in care practices, morbidity, and mortality of extremely preterm neonates, 1993–2012. JAMA. 2015;314:1039–51.
MacLean JE, DeHaan K, Fuhr D, Hariharan S, Kamstra B, Hendson L, et al. Altered breathing mechanics and ventilatory response during exercise in children born extremely preterm. Thorax. 2016;71:1012–9.
Welsh L, Kirkby J, Lum S, Odendaal D, Marlow N, Derrick G, et al. The EPICure study: maximal exercise and physical activity in school children born extremely preterm. Thorax. 2010;65:165–72.
Natarajan G, Pappas A, Shankaran S, Kendrick DE, Das A, Higgins RD, et al. Outcomes of extremely low birth weight infants with bronchopulmonary dysplasia: impact of the physiologic definition. Early Hum Dev. 2012;88:509–15.
Schmidt B, Roberts RS, Davis PG, Doyle LW, Asztalos EV, Opie G, et al. Prediction of late death or disability at age 5 years using a count of 3 neonatal morbidities in very low birth weight infants. J Pediatr. 2015;167:982–6.e982.
Doyle LW, Cheong JL, Ehrenkranz RA, Halliday HL. Late (>7 days) systemic postnatal corticosteroids for prevention of bronchopulmonary dysplasia in preterm infants. Cochrane Database Syst Rev. 2017;10:Cd001145.
Baud O, Maury L, Lebail F, Ramful D, El Moussawi F, Nicaise C, et al. Effect of early low-dose hydrocortisone on survival without bronchopulmonary dysplasia in extremely preterm infants (PREMILOC): a double-blind, placebo-controlled, multicentre, randomised trial. Lancet. 2016;387:1827–36.
Yeh TF, Lin YJ, Huang CC, Chen YJ, Lin CH, Lin HC, et al. Early dexamethasone therapy in preterm infants: a follow-up study. Pediatrics. 1998;101:E7.
Yeh TF, Lin YJ, Lin HC, Huang CC, Hsieh WS, Lin CH, et al. Outcomes at school age after postnatal dexamethasone therapy for lung disease of prematurity. N. Engl J Med. 2004;350:1304–13.
Doyle LW, Cheong JL, Ehrenkranz RA, Halliday HL. Early (< 8 days) systemic postnatal corticosteroids for prevention of bronchopulmonary dysplasia in preterm infants. Cochrane Database Syst Rev. 2017;10:Cd001146.
Doyle LW, Halliday HL, Ehrenkranz RA, Davis PG, Sinclair JC. Impact of postnatal systemic corticosteroids on mortality and cerebral palsy in preterm infants: effect modification by risk for chronic lung disease. Pediatrics. 2005;115:655–61.
Ancel P, Goffinet F, E WG. Survival and morbidity of preterm children born at 22 through 34 weeks’ gestation in france in 2011: results of the epipage-2 cohort study. JAMA Pediatr. 2015;169:230–8.
Doyle LW, Halliday HL, Ehrenkranz RA, Davis PG, Sinclair JC. An update on the impact of postnatal systemic corticosteroids on mortality and cerebral palsy in preterm infants: effect modification by risk of bronchopulmonary dysplasia. J Pediatr. 2014;165:1258–60.
American Academy of Pediatrics, Committee on Fetus and Newborn. Postnatal corticosteroids to prevent or treat bronchopulmonary dysplasia. Pediatrics. 2010;126:800–8.
Costeloe KL, Hennessy EM, Haider S, Stacey F, Marlow N, Draper ES. Short term outcomes after extreme preterm birth in England: comparison of two birth cohorts in 1995 and 2006 (the EPICure studies). BMJ. 2012;345:e7976.
Onland W, De Jaegere AP, Offringa M, van Kaam A. Systemic corticosteroid regimens for prevention of bronchopulmonary dysplasia in preterm infants. Cochrane Database Syst Rev. 2017;1:Cd010941.
Walsh MC, Morris BH, Wrage LA, Vohr BR, Poole WK, Tyson JE, et al. Extremely low birthweight neonates with protracted ventilation: mortality and 18-month neurodevelopmental outcomes. J Pediatr. 2005;146:798–804.
Jensen EA, DeMauro SB, Kornhauser M, Aghai ZH, Greenspan JS, Dysart KC. Effects of multiple ventilation courses and duration of mechanical ventilation on respiratory outcomes in extremely low-birth-weight infants. JAMA Pediatr. 2015;169:1011–7.
Choi Y-B, Lee J, Park J, Jun YH. Impact of prolonged mechanical ventilation in very low birth weight infants: results from a National Cohort Study. J Pediatr. 194:34–39.e33.
Ehrenkranz RA, Walsh MC, Vohr BR, Jobe AH, Wright LL, Fanaroff AA, et al. Validation of the National Institutes of Health consensus definition of bronchopulmonary dysplasia. Pediatrics. 2005;116:1353–60.
Malavolti AM, Bassler D, Arlettaz-Mieth R, Faldella G, Latal B, Natalucci G. Bronchopulmonary dysplasia-impact of severity and timing of diagnosis on neurodevelopment of preterm infants: a retrospective cohort study. BMJ Paediatr Open. 2018;2:e000165.
Jobe AH, Bancalari E. Bronchopulmonary dysplasia. Am J Respir Crit Care Med. 2001;163:1723–9.
Bayley N Bayley. Scales of infant and toddler development—3rd Edition. Harcourt Assessment Inc.: San Antonio; 2006.
Palisano R, Rosenbaum P, Walter S, Russell D, Wood E, Galuppi B. Development and reliability of a system to classify gross motor function in children with cerebral palsy. Dev Med Child Neurol. 1997;39:214–23.
Dupont WD, Plummer WD RC_SPLINE: Stata module to generate restricted cubic splines. Statistical Software Components, S447301. 2004. Accessed 15 May 2018. https://ideas.repec.org/c/boc/bocode/s447301.html
Harrell FE. Regression Modeling Strategies: With Applications to Linear Models, Logistic and Ordinal Regression, and Survival Analysis. Spinger-Verlag New York, Inc: New York, NY; 2001.
Alexander GR, Himes JH, Kaufman RB, Mor J, Kogan M. A United States national reference for fetal growth. Obstet Gynecol. 1996;87:163–8.
Doyle LW, Ehrenkranz RA, Halliday HL. Late (> 7 days) postnatal corticosteroids for chronic lung disease in preterm infants. Cochrane Database Syst Rev. 2014;5:Cd001145.
Halliday HL, Patterson CC, Halahakoon CW. A multicenter, randomized open study of early corticosteroid treatment (OSECT) in preterm infants with respiratory illness: comparison of early and late treatment and of dexamethasone and inhaled budesonide. Pediatrics. 2001;107:232–40.
Merz U, Peschgens T, Kusenbach G, Hornchen H. Early versus late dexamethasone treatment in preterm infants at risk for chronic lung disease: a randomized pilot study. Eur J Pediatr. 1999;158:318–22.
Papile LA, Tyson JE, Stoll BJ, Wright LL, Donovan EF, Bauer CR, et al. A multicenter trial of two dexamethasone regimens in ventilator-dependent premature infants. N. Engl J Med. 1998;338:1112–9.
Wilson-Costello D, Walsh MC, Langer JC, Guillet R, Laptook AR, Stoll BJ, et al. Impact of postnatal corticosteroid use on neurodevelopment at 18 to 22 months’ adjusted age: effects of dose, timing, and risk of bronchopulmonary dysplasia in extremely low birth weight infants. Pediatrics. 2009;123:e430–437.
Vohr BR, Stephens BE, Higgins RD, Bann CM, Hintz SR, Das A, et al. Are outcomes of extremely preterm infants improving? Impact of Bayley assessment on outcomes. J Pediatr. 2012;161:222–8 e223.
Onland W, Cools F, Kroon A, Rademaker K, Merkus MP, Dijk PH, et al. Effect of hydrocortisone therapy initiated 7 to 14 days after birth on mortality or bronchopulmonary dysplasia among very preterm infants receiving mechanical ventilation: a randomized clinical TrialEffect of hydrocortisone on BPD and mortality in very preterm mechanically ventilated infants effect of hydrocortisone on BPD and mortality in very preterm mechanically ventilated infants. JAMA. 2019;321:354–63.
Kersbergen KJ, de Vries LS, van Kooij BJ, Isgum I, Rademaker KJ, van Bel F, et al. Hydrocortisone treatment for bronchopulmonary dysplasia and brain volumes in preterm infants. J Pediatr. 2013;163:666–71.e1.
NICHD Neonatal Research Network. Hydrocortisone for BPD. May 13, 2011 ed. Bethesda, MD: National Library of Medicine.
Acknowledgements
The National Institutes of Health, the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD), the National Center for Research Resources, and the National Center for Advancing Translational Sciences provided grant support for the Neonatal Research Network’s Generic Database and Follow-up Studies through cooperative agreements. While NICHD staff did have input into the study design, conduct, analysis, and manuscript drafting, the content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. Data collected at participating sites of the NICHD Neonatal Research Network (NRN) were transmitted to RTI International, the data coordinating center (DCC) for the network, which stored, managed and analyzed the data for this study. On behalf of the NRN, AD (DCC Principal Investigator) and Douglas Kendrick (DCC Statistician) had full access to all the data in the study and take responsibility for the integrity of the data and accuracy of the data analysis. We are indebted to our medical and nursing colleagues and the infants and their parents who agreed to take part in this study.
Eunice Kennedy Shriver National Institute of Child Health and Human Development Neonatal Research Network
Michael S. Caplan8, Abbott R. Laptook9, Martin Keszler9, Betty R. Vohr9, Barbara Alksninis9, Kristin M. Basso9, Robert Burke9, Melinda Caskey9, Katharine Johnson9, Mary Lenore Keszler9, Andrea M. Knoll9, Theresa M. Leach9, Emilee Little9, Elisabeth C. McGowan9, Elisa Vieira9, Victoria E. Watson9, Suzy Ventura9, Michele C. Walsh10, Anna Maria Hibbs10, Deanne E. Wilson-Costello10, Nancy S. Newman10, Allison H. Payne10, Bonnie S. Siner10, Monika Bhola10, Gulgun Yalcinkaya10, William E. Truog11, Eugenia K. Pallotto11, Howard W. Kilbride11, Cheri Gauldin11, Anne Holmes11, Kathy Johnson11, Allison Scott11, Kurt Schibler12, Edward F. Donovan12, Cathy Grisby12, Kate Bridges12, Barbara Alexander12, Estelle E. Fischer12, Holly L. Mincey12, Jody Hessling12, Teresa L. Gratton12, Lenora Jackson12, Kristin Kirker12, Greg Muthig12, Jean J. Steichen12, Stacey Tepe12, Kimberly Yolton12, Ronald N. Goldberg13, C. Michael Cotten13, Ricki F. Goldstein13, Patricia L. Ashley13, William F. Malcolm13, Kathy J. Auten13, Kimberley A. Fisher13, Sandra Grimes13, Kathryn E. Gustafson13, Melody B. Lohmeyer13, Joanne Finkle13, Matthew M. Laughon13, Carl L. Bose13, Janice Bernhardt13, Gennie Bose13, Diane Warner13, Janice Wereszczak13, David P. Carlton14, Barbara J. Stoll14, Ira Adams-Chapman14, Ellen C. Hale14, Yvonne Loggins14, Ann Blackwelder14, Lynn C. Wineski14, Maureen Mulligan LaRossa14, Sheena L. Carter14, Rosemary D. Higgins15, Stephanie Wilson Archer15, Brenda B. Poindexter16, Anna M. Dusick16, Lu-Ann Papile16, Susan Gunn16, Faithe Hamer16, Dianne E. Herron16, Abbey C. Hines16, Carolyn Lytle16, Heike M. Minnich16, Lucy Smiley16, Leslie Dawn Wilson16, Kathleen A. Kennedy17, Jon E. Tyson17, Georgia E. McDavid17, Nora I. Alaniz17, Julie Arldt-McAlister17, Katrina Burson17, Allison G. Dempsey17, Andrea F. Duncan17, Patricia W. Evans17, Charles E. Green17, Beverly Foley Harris17, Margarita Jiminez17, Janice John17, Patrick M. Jones17, Layne M. Lillie17, Anna E. Lis17, Sara C. Martin17, Brenda H. Morris17, M. Layne Poundstone17, Shawna Rodgers17, Saba Siddiki17, Maegan C. Simmons17, Daniel Sperry17, Patti L. Pierce Tate17, Sharon L. Wright17, Pablo J. Sanchez18, Leif D. Nelin18, Sudarshan R. Jadcherla18, Patricia Luzader18, Christine A. Fortney18, Gail E. Besner18, Nehal A. Parikh18, Abhik Das19, Dennis Wallace19, Marie G. Gantz19, W. Kenneth Poole19, Jamie E. Newman19, Jeanette O’Donnell Auman19, Margaret M. Crawford19, Jenna Gabrio19, Carolyn M. Petrie Huitema19, Kristin M. Zaterka-Baxter19, Krisa P. Van Meurs20, David K. Stevenson20, Susan R. Hintz20, M. Bethany Ball20, Alexis S. Davis20, Andrew W. Palmquist20, Melinda S. Proud20, Barbara Bentley20, Elizabeth Bruno20, Maria Elena DeAnda20, Anne M. DeBattista20, Beth Earhart20, Lynne C. Huffman20, Jean G. Kohn20, Casey Krueger20, Hali E. Weiss20, Ivan D. Frantz III21, John M. Fiascone21, Brenda L. MacKinnon21, Anne Furey21, Ellen Nylen21, Elisabeth C. McGowan21, Cecelia E. Sibley21, Ana K. Brussa21, Waldemar A. Carlo22, Namasivayam Ambalavanan22, Myriam Peralta-Carcelen22, Monica V. Collins22, Shirley S. Cosby22, Fred J. Biasini22, Kristen C. Johnston22, Kathleen G. Nelson22, Cryshelle S. Patterson22, Vivien A. Phillips22, Sally Whitley22, Uday Devaskar23, Meena Garg23, Isabell B. Purdy23, Teresa Chanlaw23, Rachel Geller23, Neil N. Finer24, Yvonne E. Vaucher24, David Kaegi24, Maynard R. Rasmussen24, Kathy Arnell24, Clarence Demetrio24, Martha G. Fuller24, Wade Rich24, Tarah T. Colaizy25, Michael J. Acarregui25, Jane E. Brumbaugh25, Dan L. Ellsbury25, John A. Widness25, Karen J. Johnson25, Donia B. Campbell25, Diane L. Eastman25, Jacky R. Walker25, Shahnaz Duara26, Charles R. Bauer26, Ruth Everett-Thomas26, Sylvia Fajardo-Hiriart26, Arielle Rigaud26, Maria Calejo26, Silvia M. Frade Eguaras26, Michelle Harwood Berkowits26, Andrea Garcia26, Helina Pierre26, Alexandra Stoerger26, Kristi L. Watterberg27, Jean R. Lowe27, Janell F. Fuller27, Robin K. Ohls27, Conra Backstrom Lacy27, Andrea F. Duncan27, Rebecca Montman27, Sandra Sundquist Beauman27, Barbara Schmidt28, Haresh Kirpalani28, Aasma S. Chaudhary28, Soraya Abbasi28, Toni Mancini28, Dara M. Cucinotta28, Judy C. Bernbaum28, Marsha Gerdes28, Hallam Hurt28, Carl T. D’Angio29, Dale L. Phelps29, Ronnie Guillet29, Satyan Lakshminrusimha29, Julie Babish Johnson29, Linda J. Reubens29, Cassandra A. Horihan29, Diane Hust29, Rosemary L. Jensen29, Emily Kushner29, Joan Merzbach29, Gary J. Myers29, Holly I. M. Wadkins29, Stephanie Guilford29, Deanna Maffett29, Osman Farooq29, Diane Prinzing29, Anne Marie Reynolds29, Mary Rowan29, Michael G. Sacilowski29, Ashley Williams29, Karen Wynn29, Kelley Yost29, William Zorn29, Lauren Zwetsch29, Pablo J. Sanchez30, Luc P. Brion30, Roy J. Heyne30, Walid A. Salhab30, Charles R. Rosenfeld30, Diana M. Vasil30, Lijun Chen30, Alicia Guzman30, Gaynelle Hensley30, Melissa H. Leps30, Nancy A. Miller30, Janet S. Morgan30, Sally S. Adams30, Catherine Twell Boatman30, Elizabeth T. Heyne30, Linda A. Madden30, Lizette E. Lee30, Roger G. Faix31, Bradley A. Yoder31, Karen A. Osborne31, Cynthia Spencer31, Kimberlee Weaver-Lewis31, Shawna Baker31, Karie Bird31, Jill Burnett31, Michael Steffen31, Jennifer J. Jensen31, Sarah Winter31, Karen Zanetti31, T. Michael O’Shea32, Robert G. Dillard32, Lisa K. Washburn32, Barbara G. Jackson32, Nancy Peters32, Korinne Chiu32, Deborah Evans Allred32, Donald J. Goldstein32, Raquel Halfond32, Carroll Peterson32, Ellen L. Waldrep32, Cherrie D. Welch32, Melissa Whalen Morris32, Gail Wiley Hounshell32, Seetha Shankaran33, Athina Pappas33, John Barks33, Rebecca Bara33, Laura A. Goldston33, Girija Natarajan33, Monika Bajaj33, Sanjay Chawla33, Lilia C. De Jesus33, Beena G. Sood33, Mary Christensen33, Stephanie A. Wiggins33, Diane White33, Richard A. Ehrenkranz34, Harris Jacobs34, Christine G. Butler34, Patricia Cervone34, Sheila Greisman34, Monica Konstantino34, JoAnn Poulsen34, Janet Taft34, Joanne Williams34, Elaine Romano34
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Members of the Eunice Kennedy Shriver National Institute of Child Health and Human Development Neonatal Research Network are listed below Acknowledgements.
Rights and permissions
About this article
Cite this article
Harmon, H.M., Jensen, E.A., Tan, S. et al. Timing of postnatal steroids for bronchopulmonary dysplasia: association with pulmonary and neurodevelopmental outcomes. J Perinatol 40, 616–627 (2020). https://doi.org/10.1038/s41372-020-0594-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41372-020-0594-4
This article is cited by
-
Prophylactic early low-dose hydrocortisone and survival without bronchopulmonary dysplasia among extremely preterm infants born at 22–27 weeks’ gestation
Journal of Perinatology (2024)
-
The impact of early tracheostomy on neurodevelopmental outcomes of infants with severe bronchopulmonary dysplasia exposed to postnatal corticosteroids
Journal of Perinatology (2023)
-
Presumed adrenal insufficiency in neonates treated with corticosteroids for the prevention of bronchopulmonary dysplasia
Journal of Perinatology (2022)
-
Pattern of postnatal steroid use for bronchopulmonary dysplasia in extremely preterm infants
Journal of Perinatology (2022)
-
Using quality improvement to implement consensus guidelines for postnatal steroid treatment of preterm infants with developing bronchopulmonary dysplasia
Journal of Perinatology (2021)