Abstract
Objective
To assess whether prenatal exposure to marijuana (THC) results in abnormal amplitude integrated encephalograms (aEEG).
Design
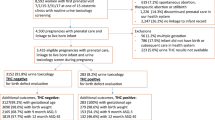
This was a (2018–2020) prospective cohort study of prenatally THC-exposed newborns. Maternal and Infant demographics, urine (UDS) and umbilical cord drug screening (UCDS) were recorded. A limited channel continuous aEEG was obtained within 48 h of birth. Statistical analysis included univariate, multivariate, and logistical regression.
Results
A total of 30 mother/infant dyads were enrolled. 60% (18/30) of neonates had abnormal aEEGs with sleep wake cycle (SWC) disturbances (p < 0.001). UCDS Carboxy-THC pg/g levels were similar in infants with abnormal [1758 (296,2838)] and normal aEEG [1589 (332,2794)], p = 0.82.
Conclusions
Absence of SWCs on aEEG is associated with prenatal THC exposure. While THC UCDS levels did not correlate to aEEG results future longitudinal studies are necessary to obtain detailed history of THC use and to evaluate its association with abnormal aEEG and the neurodevelopmental outcomes.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Jansson LM, Jordan CJ, Velez ML. Perinatal marijuana use and the developing child. JAMA. 2018;320:545–6.
El Marroun H, Tiemeier H, Jaddoe VW, Hofman A, Verhulst FC, van den Brink W, et al. Agreement between maternal cannabis use during pregnancy according to self-report and urinalysis in a population-based cohort: the generation R study. Eur Addict Res. 2011;17:37–43.
Ko JY, Farr SL, Tong VT, Creanga AA, Callaghan WM. Prevalence and patterns of marijuana use among pregnant and nonpregnant women of reproductive age. Am J Obstet Gynecol. 2015;213:201.e1–e10.
Redberg RF. JAMA internal medicine-the year in review, 2017. JAMA Intern Med. 2018;178:456–7.
Gunn JK, Rosales CB, Center KE, Nunez A, Gibson SJ, Christ C, et al. Prenatal exposure to cannabis and maternal and child health outcomes: a systematic review and meta-analysis. BMJ Open. 2016;6:e009986.
Fried PA. The Ottawa Prenatal Prospective Study (OPPS): methodological issues and findings–it’s easy to throw the baby out with the bath water. Life Sci. 1995;56:2159–68.
Committee Opinion Summary NO. 722. Marijuana use during pregnancy and lactation. Obstet Gynecol. 2017;130:931–2.
Day N, Cornelius M, Goldschmidt L, Richardson G, Robles N, Taylor P. The effects of prenatal tobacco and marijuana use on offspring growth from birth through 3 years of age. Neurotoxicol Teratol. 1992;14:407–14.
El Marroun H, Brown QL, Lund IO, Coleman-Cowger VH, Loree AM, Chawla D, et al. An epidemiological, developmental and clinical overview of cannabis use during pregnancy. Preventive Med. 2018;116:1–5.
Behnke M, Smith VC. Committee on substance A, committee on F, newborn. Prenatal substance abuse: short- and long-term effects on the exposed fetus. Pediatrics. 2013;131:e1009–24.
Laprevote V, Bon L, Krieg J, Schwitzer T, Bourion-Bedes S, Maillard L, et al. Association between increased EEG signal complexity and cannabis dependence. Eur Neuropsychopharmacol. 2017.
Scher MS, Richardson GA, Coble PA, Day NL, Stoffer DS. The effects of prenatal alcohol and marijuana exposure: disturbances in neonatal sleep cycling and arousal. Pediatr Res. 1988;24:101–5.
Variane GFT, Magalhaes M, Gasperine R, Alves H, Scoppetta T, Figueredo RJG, et al. Early amplitude-integrated electroencephalography for monitoring neonates at high risk for brain injury. J Pediatr. 2017;93:460–6.
Massaro AN, Tsuchida T, Kadom N, El-Dib M, Glass P, Baumgart S, et al. aEEG evolution during therapeutic hypothermia and prediction of NICU outcome in encephalopathic neonates. Neonatology. 2012;102:197–202.
Rana D, Pollard L, Rowland J, Dhanireddy R, Pourcyrous M. Amplitude-integrated EEG in infants with neonatal abstinence syndrome. J Neonatal Perinat Med. 2019;12:391–7.
Hellstrom-Westas DVL, Rosen I. An atlas of amplitude integrated EEGs in the newborn. London: CRC Press; 2008.
CFM NB. Natus Brainz Olympic CFM manual. San Carlos, CA 2017.
Sisman J, Campbell DE, Brion LP. Amplitude-integrated EEG in preterm infants: maturation of background pattern and amplitude voltage with postmenstrual age and gestational age. J Perinatol. 2005;25:391–6.
El Marroun H, Tiemeier H, Steegers EA, Jaddoe VW, Hofman A, Verhulst FC, et al. Intrauterine cannabis exposure affects fetal growth trajectories: the generation R Study. J Am Acad Child Adolesc Psychiatry. 2009;48:1173–81.
Tortoriello G, Morris CV, Alpar A, Fuzik J, Shirran SL, Calvigioni D, et al. Miswiring the brain: delta9-tetrahydrocannabinol disrupts cortical development by inducing an SCG10/stathmin-2 degradation pathway. EMBO J. 2014;33:668–85.
Grotenhermen F. Pharmacokinetics and pharmacodynamics of cannabinoids. Clin Pharmacokinet. 2003;42:327–60.
Richardson KA, Hester AK, McLemore GL. Prenatal cannabis exposure—The “first hit” to the endocannabinoid system. Neurotoxicol Teratol. 2016;58:5–14.
Goldschmidt L, Day NL, Richardson GA. Effects of prenatal marijuana exposure on child behavior problems at age 10. Neurotoxicol Teratol. 2000;22:325–36.
Day N, Sambamoorthi U, Taylor P, Richardson G, Robles N, Jhon Y, et al. Prenatal marijuana use and neonatal outcome. Neurotoxicol Teratol. 1991;13:329–34.
Dahl RE, Scher MS, Williamson DE, Robles N, Day N. A longitudinal study of prenatal marijuana use. Effects on sleep and arousal at age 3 years. Arch Pediatr Adolesc Med. 1995;149:145–50.
Fried PA. Prenatal exposure to tobacco and marijuana: effects during pregnancy, infancy, and early childhood. Clin Obstet Gynecol. 1993;36:319–37.
Bertrand KA, Hanan NJ, Honerkamp-Smith G, Best BM, Chambers CD. Marijuana use by breastfeeding mothers and cannabinoid concentrations in breast milk. Pediatrics. 2018;142.
Broyd SJ, van Hell HH, Beale C, Yucel M, Solowij N. Acute and chronic effects of cannabinoids on human cognition—a systematic review. Biol Psychiatry. 2016;79:557–67.
Skosnik PD, Krishnan GP, D’Souza DC, Hetrick WP, O’Donnell BF. Disrupted gamma-band neural oscillations during coherent motion perception in heavy cannabis users. Neuropsychopharmacology. 2014;39:3087–99.
Cheng H, Skosnik PD, Pruce BJ, Brumbaugh MS, Vollmer JM, Fridberg DJ, et al. Resting state functional magnetic resonance imaging reveals distinct brain activity in heavy cannabis users - a multi-voxel pattern analysis. J Psychopharmacol. 2014;28:1030–40.
Gates P, Albertella L, Copeland J. Cannabis withdrawal and sleep: a systematic review of human studies. Subst Abus. 2016;37:255–69.
Cranford JA, Arnedt JT, Conroy DA, Bohnert KM, Bourque C, Blow FC, et al. Prevalence and correlates of sleep-related problems in adults receiving medical cannabis for chronic pain. Drug Alcohol Depend. 2017;180:227–33.
Conroy DA, Arnedt JT. Sleep and substance use disorders: an update. Curr Psychiatry Rep. 2014;16:487.
Herning RI, Better W, Tate K, Cadet JL. EEG deficits in chronic marijuana abusers during monitored abstinence: preliminary findings. Ann NY Acad Sci. 2003;993:75–8. discussion 9-81
Volkow ND, Compton WM, Weiss SR. Adverse health effects of marijuana use. N Engl J Med. 2014;371:879.
Morris CV, DiNieri JA, Szutorisz H, Hurd YL. Molecular mechanisms of maternal cannabis and cigarette use on human neurodevelopment. Eur J Neurosci. 2011;34:1574–83.
Fride E. Multiple roles for the endocannabinoid system during the earliest stages of life: pre- and postnatal development. J Neuroendocrinol. 2008;20(Suppl 1):S75–S81.
Bonnin A, de Miguel R, Castro JG, Ramos JA, Fernandez-Ruiz JJ. Effects of perinatal exposure to delta 9-tetrahydrocannabinol on the fetal and early postnatal development of tyrosine hydroxylase-containing neurons in rat brain. J Mol Neurosci. 1996;7:291–308.
Wang X, Dow-Edwards D, Keller E, Hurd YL. Preferential limbic expression of the cannabinoid receptor mRNA in the human fetal brain. Neuroscience. 2003;118:681–94.
Thompson R, DeJong K, Lo J. Marijuana use in pregnancy: a review. Obstet Gynecol Surv. 2019;74:415–28.
Beggiato S, Borelli AC, Tomasini MC, Morgano L, Antonelli T, Tanganelli S, et al. Long-lasting alterations of hippocampal GABAergic neurotransmission in adult rats following perinatal Delta(9)-THC exposure. Neurobiol Learn Mem. 2017;139:135–43.
Shellhaas RA, Burns JW, Hassan F, Carlson MD, Barks JDE, Chervin RD. Neonatal sleep-wake analyses predict 18-month neurodevelopmental outcomes. LID—https://doi.org/10.1093/sleep/zsx144. (1550-9109 (Electronic)).
Barbeau DY, Weiss MD. Sleep disturbances in newborns. Children. 2017;4.
Shellhaas RA, Burns Jw Fau - Barks JDE, Barks Jd Fau - Chervin RD, Chervin RD. Quantitative sleep stage analyses as a window to neonatal neurologic function. (1526-632X (Electronic)).
Cseko AJ, Bango M, Lakatos P, Kardasi J, Pusztai L, Szabo M. Accuracy of amplitude-integrated electroencephalography in the prediction of neurodevelopmental outcome in asphyxiated infants receiving hypothermia treatment. Acta Paediatr. 2013;102:707–11.
Weisman O, Magori-Cohen R, Louzoun Y, Eidelman AI, Feldman R. Sleep-wake transitions in premature neonates predict early development. Pediatrics. 2011;128:706–14.
Hellstrom-Westas L, Klette H, Thorngren-Jerneck K, Rosen I. Early prediction of outcome with aEEG in preterm infants with large intraventricular hemorrhages. Neuropediatrics. 2001;32:319–24.
Kidokoro H, Inder T, Okumura A, Watanabe K. What does cyclicity on amplitude-integrated EEG mean? J Perinatol. 2012;32:565–9.
Suk D, Krauss AN, Engel M, Perlman JM. Amplitude-integrated electroencephalography in the NICU: frequent artifacts in premature infants may limit its utility as a monitoring device. Pediatrics. 2009;123:e328–32.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Pollack, R., Rana, D., Purvis, J. et al. Effect of prenatal marijuana exposure on sleep wake cycles and amplitude-integrated electroencephalogram (aEEG). J Perinatol 41, 1355–1363 (2021). https://doi.org/10.1038/s41372-020-00911-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41372-020-00911-9