Abstract
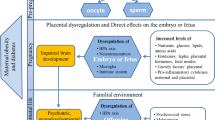
There is growing clinical and experimental evidence to suggest that maternal obesity increases children’s susceptibility to neurodevelopmental and neuropsychiatric disorders. Given the worldwide obesity epidemic, it is crucial that we acquire a thorough understanding of the available evidence, identify gaps in knowledge, and develop an agenda for intervention. This review synthesizes human and animal studies investigating the association between maternal obesity and offspring brain health. It also highlights key mechanisms underlying these effects, including maternal and fetal inflammation, alterations to the microbiome, epigenetic modifications of neurotrophic genes, and impaired dopaminergic and serotonergic signaling. Lastly, this review highlights several proposed interventions and priorities for future investigation.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Branum AM, Kirmeyer SE, Gregory ECW. Prepregnancy body mass index by maternal characteristics and state: data from the birth certificate, 2014. Natl Vital- Stat Rep. 2016;65:1–11.
Johnson JL, Farr SL, Dietz PM, Sharma AJ, Barfield WD, Robbins CL. Trends in gestational weight gain: the Pregnancy Risk Assessment Monitoring System, 2000—2009. Am J Obstet Gynecol. 2015;212:806.e1–e8.
Rowlands I, Graves N, de Jersey S, McIntyre HD, Callaway L. Obesity in pregnancy: outcomes and economics. Semin Fetal Neonatal Med. 2010;15:94–99.
Boney CM, Verma A, Tucker R, Vohr BR. Metabolic syndrome in childhood: association with birth weight, maternal obesity, and gestational diabetes mellitus. Pediatrics. 2005;115:290–6.
Godfrey KM, Reynolds RM, Prescott SL, Nyirenda M, Jaddoe VWV, Eriksson JG, et al. Influence of maternal obesity on the long-term health of offspring. Lancet Diabetes Endocrinol. 2017;5:53–64.
Coo H, Fabrigar L, Davies G, Fitzpatrick R, Flavin M. Are observed associations between a high maternal prepregnancy body mass index and offspring IQ likely to be causal? J Epidemiol Community Health. 2019;73:920–8.
Huang L, Yu X, Keim S, Li L, Zhang L, Zhang J. Maternal prepregnancy obesity and child neurodevelopment in the Collaborative Perinatal Project. Int J Epidemiol. 2014;43:783–92.
Pugh SJ, Richardson GA, Hutcheon JA, Himes KP, Brooks MM, Day NL, et al. Maternal Obesity and Excessive Gestational Weight Gain Are Associated with Components of Child Cognition. J Nutr. 2015;145:2562–9.
Pugh SJ, Hutcheon JA, Richardson GA, Brooks MM, Himes KP, Day NL, et al. Child academic achievement in association with pre-pregnancy obesity and gestational weight gain. J Epidemiol Community Health. 2016;70:534–40.
Tanda R, Salsberry PJ, Reagan PB, Fang MZ. The Impact of Prepregnancy Obesity on Children’s Cognitive Test Scores. Matern Child Health J. 2013;17:222–9.
Torres-Espinola FJ, Berglund SK, García-Valdés LM, Segura MT, Jerez A, Campos D, et al. Maternal Obesity, Overweight and Gestational Diabetes Affect the Offspring Neurodevelopment at 6 and 18 Months of Age – A Follow Up from the PREOBE Cohort. PLOS ONE. 2015;10:e0133010.
Casas M, Chatzi L, Carsin A-E, Amiano P, Guxens M, Kogevinas M, et al. Maternal pre-pregnancy overweight and obesity, and child neuropsychological development: two Southern European birth cohort studies. Int J Epidemiol. 2013;42:506–17.
Hinkle SN, Schieve LA, Stein AD, Swan DW, Ramakrishnan U, Sharma AJ. Associations between maternal prepregnancy body mass index and child neurodevelopment at 2 years of age. Int J Obes. 2012;36:1312–9.
Mann JR, McDermott SW, Hardin J, Pan C, Zhang Z. Pre-pregnancy body mass index, weight change during pregnancy, and risk of intellectual disability in children. BJOG Int J Obstet Gynaecol. 2013;120:309–19.
Zhu Y, Yan H, Tang M, Fu Y, Hu X, Zhang F, et al. Impact of maternal prepregnancy body mass index on cognitive and metabolic profiles of singletons born after in vitro fertilization/intracytoplasmic sperm injection. Fertil Steril. 2019;112:1094–102.e2.
Widen EM, Nichols AR, Kahn LG, Factor-Litvak P, Insel BJ, Hoepner L, et al. Prepregnancy obesity is associated with cognitive outcomes in boys in a low-income, multiethnic birth cohort. BMC Pediatr. 2019;19:1–10.
Nichols AR, Rundle AG, Factor-Litvak P, Insel BJ, Hoepner L, Rauh V, et al. Prepregnancy obesity is associated with lower psychomotor development scores in boys at age 3 in a low-income, minority birth cohort. J Dev Orig Health Dis. 2020;11:49–57.
Rodriguez A, Miettunen J, Henriksen TB, Olsen J, Obel C, Taanila A, et al. Maternal adiposity prior to pregnancy is associated with ADHD symptoms in offspring: evidence from three prospective pregnancy cohorts. Int J Obes. 2008;32:550–7.
Chen Q, Sjölander A, Långström N, Rodriguez A, Serlachius E, D’Onofrio BM, et al. Maternal pre-pregnancy body mass index and offspring attention deficit hyperactivity disorder: a population-based cohort study using a sibling-comparison design. Int J Epidemiol. 2014;43:83–90.
Kong L, Norstedt G, Schalling M, Gissler M, Lavebratt C. The Risk of Offspring Psychiatric Disorders in the Setting of Maternal Obesity and Diabetes. Pediatrics. 2018; 142, https://doi.org/10.1542/peds.2018-0776.
Andersen CH, Thomsen PH, Nohr EA, Lemcke S. Maternal body mass index before pregnancy as a risk factor for ADHD and autism in children. Eur Child Adolesc Psychiatry. 2018;27:139–48.
Pugh SJ, Hutcheon JA, Richardson GA, Brooks MM, Himes KP, Day NL, et al. Gestational weight gain, prepregnancy body mass index and offspring attention-deficit hyperactivity disorder symptoms and behaviour at age 10. BJOG Int J Obstet Gynaecol. 2016;123:2094–103.
Daraki V, Roumeliotaki T, Koutra K, Georgiou V, Kampouri M, Kyriklaki A, et al. Effect of parental obesity and gestational diabetes on child neuropsychological and behavioral development at 4 years of age: the Rhea mother–child cohort, Crete, Greece. Eur Child Adolesc Psychiatry. 2017;26:703–14.
Mina TH, Lahti M, Drake AJ, Räikkönen K, Minnis H, Denison FC, et al. Prenatal exposure to very severe maternal obesity is associated with adverse neuropsychiatric outcomes in children. Psychol Med. 2017;47:353–62.
Fuemmeler BF, Zucker N, Sheng Y, Sanchez CE, Maguire R, Murphy SK et al. Pre-Pregnancy Weight and Symptoms of Attention Deficit Hyperactivity Disorder and Executive Functioning Behaviors in Preschool Children. Int J Environ Res Public Health. 2019; 16, https://doi.org/10.3390/ijerph16040667.
Robinson SL, Ghassabian A, Sundaram R, Trinh M-H, Lin T-C, Bell EM et al. Parental Weight Status and Offspring Behavioral Problems and Psychiatric Symptoms. J Pediatr. 2020, https://doi.org/10.1016/j.jpeds.2020.01.016.
Casas M, Forns J, Martínez D, Guxens M, Fernandez-Somoano A, Ibarluzea J, et al. Maternal pre-pregnancy obesity and neuropsychological development in pre-school children: a prospective cohort study. Pediatr Res. 2017;82:596–606.
Li M, Fallin MD, Riley A, Landa R, Walker SO, Silverstein M et al. The Association of Maternal Obesity and Diabetes With Autism and Other Developmental Disabilities. Pediatrics. 2016; 137, https://doi.org/10.1542/peds.2015-2206.
Varcin KJ, Newnham JP, Whitehouse AJO. Maternal pre-pregnancy weight and autistic-like traits among offspring in the general population. Autism Res. 2019;12:80–88.
Getz KD, Anderka MT, Werler MM, Jick SS. Maternal Pre-pregnancy Body Mass Index and Autism Spectrum Disorder among Offspring: A Population-Based Case–Control Study. Paediatr Perinat Epidemiol. 2016;30:479–87.
Windham GC, Anderson M, Lyall K, Daniels JL, Kral TVE, Croen LA, et al. Maternal Pre-pregnancy Body Mass Index and Gestational Weight Gain in Relation to Autism Spectrum Disorder and other Developmental Disorders in Offspring. Autism Res. 2019;12:316–27.
Dodds L, Fell DB, Shea S, Armson BA, Allen AC, Bryson S. The Role of Prenatal, Obstetric and Neonatal Factors in the Development of Autism. J Autism Dev Disord. 2011;41:891–902.
Shen Y, Dong H, Lu X, Lian N, Xun G, Shi L, et al. Associations among maternal pre-pregnancy body mass index, gestational weight gain and risk of autism in the Han Chinese population. BMC Psychiatry. 2018;18:1–7.
Bilder DA, Bakian AV, Viskochil J, Clark EAS, Botts EL, Smith KR, et al. Maternal Prenatal Weight Gain and Autism Spectrum Disorders. Pediatrics. 2013;132:e1276–83.
Reynolds LC, Inder TE, Neil JJ, Pineda RG, Rogers CE. Maternal obesity and increased risk for autism and developmental delay among very preterm infants. J Perinatol. 2014;34:688–92.
Gardner RM, Lee BK, Magnusson C, Rai D, Frisell T, Karlsson H, et al. Maternal body mass index during early pregnancy, gestational weight gain, and risk of autism spectrum disorders: Results from a Swedish total population and discordant sibling study. Int J Epidemiol. 2015;44:870–83.
Rodriguez A. Maternal pre-pregnancy obesity and risk for inattention and negative emotionality in children. J Child Psychol Psychiatry. 2010;51:134–43.
Van Lieshout RJ, Robinson M, Boyle MH. Maternal Pre-Pregnancy Body Mass Index and Internalizing and Externalizing Problems in Offspring. Can J Psychiatry. 2013;58:151–9.
Robinson M, Zubrick SR, Pennell CE, Lieshout RJV, Jacoby P, Beilin LJ, et al. Pre-pregnancy maternal overweight and obesity increase the risk for affective disorders in offspring. J Dev Orig Health Dis. 2013;4:42–48.
Nohr EA, Vaeth M, Baker JL, Sørensen TI, Olsen J, Rasmussen KM. Combined associations of prepregnancy body mass index and gestational weight gain with the outcome of pregnancy. Am J Clin Nutr. 2008;87:1750–9.
Wang S, Sun Q, Zhai L, Bai Y, Wei W, Jia L. The Prevalence of Depression and Anxiety Symptoms among Overweight/Obese and Non-Overweight/Non-Obese Children/Adolescents in China: A Systematic Review and Meta-Analysis. Int J Environ Res Public Health. 2019;16. https://doi.org/10.3390/ijerph16030340.
Crisham Janik MD, Newman TB, Cheng YW, Xing G, Gilbert WM, Wu YW. Maternal Diagnosis of Obesity and Risk of Cerebral Palsy in the Child. J Pediatr. 2013;163:1307–12.
Villamor E, Tedroff K, Peterson M, Johansson S, Neovius M, Petersson G, et al. Association Between Maternal Body Mass Index in Early Pregnancy and Incidence of Cerebral Palsy. JAMA. 2017;317:925–36.
Pan C, Deroche CB, Mann JR, McDermott S, Hardin JW. Is Prepregnancy Obesity Associated With Risk of Cerebral Palsy and Epilepsy in Children? J Child Neurol. 2014;29:NP196–201.
Razaz N, Tedroff K, Villamor E, Cnattingius S. Maternal Body Mass Index in Early Pregnancy and Risk of Epilepsy in Offspring. JAMA Neurol. 2017;74:668–76.
Schaefer CA, Brown AS, Wyatt RJ, Kline J, Begg MD, Bresnahan MA, et al. Maternal Prepregnant Body Mass and Risk of Schizophrenia in Adult Offspring. Schizophr Bull. 2000;26:275–86.
Kawai M, Minabe Y, Takagai S, Ogai M, Matsumoto H, Mori N, et al. Poor maternal care and high maternal body mass index in pregnancy as a risk factor for schizophrenia in offspring. Acta Psychiatr Scand. 2004;110:257–63.
Mackay E, Dalman C, Karlsson H, Gardner RM. Association of Gestational Weight Gain and Maternal Body Mass Index in Early Pregnancy With Risk for Nonaffective Psychosis in Offspring. JAMA Psychiatry. 2017;74:339–49.
Ou X, Thakali KM, Shankar K, Andres A, Badger TM. Maternal Adiposity Negatively Influences Infant Brain White Matter Development. Obes Silver Spring Md. 2015;23:1047–54.
Verdejo-Román J, Björnholm L, Muetzel RL, Torres-Espínola FJ, Lieslehto J, Jaddoe V, et al. Maternal prepregnancy body mass index and offspring white matter microstructure: results from three birth cohorts. Int J Obes. 2019;43:1995–2006.
Li X, Andres A, Shankar K, Pivik RT, Glasier CM, Ramakrishnaiah RH, et al. Differences in brain functional connectivity at resting state in neonates born to healthy obese or normal-weight mothers. Int J Obes 2005. 2016;40:1931–4.
Salzwedel AP, Gao W, Andres A, Badger TM, Glasier CM, Ramakrishnaiah RH et al. Maternal Adiposity Influences Neonatal Brain Functional Connectivity. Front Hum Neurosci. 2019; 12, https://doi.org/10.3389/fnhum.2018.00514.
Song JW, Chung KC. Observational studies: cohort and case-control studies. Plast Reconstr Surg. 2010;126:2234–42.
Kong L, Chen X, Gissler M, Lavebratt C. Relationship of prenatal maternal obesity and diabetes to offspring neurodevelopmental and psychiatric disorders: a narrative review. Int J Obes. 2020, https://doi.org/10.1038/s41366-020-0609-4.
Hariri N, Thibault L. High-fat diet-induced obesity in animal models. Nutr Res Rev. 2010;23:270–99.
Page KC, Jones EK, Anday EK. Maternal and postweaning high-fat diets disturb hippocampal gene expression, learning, and memory function. Am J Physiol-Regul Integr Comp Physiol. 2014;306:R527–37.
White CL, Pistell PJ, Purpera MN, Gupta S, Fernandez-Kim S-O, Hise TL, et al. Effects of high fat diet on Morris maze performance, oxidative stress, and inflammation in rats: contributions of maternal diet. Neurobiol Dis. 2009;35:3–13.
Fusco S, Spinelli M, Cocco S, Ripoli C, Mastrodonato A, Natale F et al. Maternal insulin resistance multigenerationally impairs synaptic plasticity and memory via gametic mechanisms. Nat Commun. 2019; 10, https://doi.org/10.1038/s41467-019-12793-3.
Kim DW, Glendining KA, Grattan DR, Jasoni CL. Maternal obesity leads to increased proliferation and numbers of astrocytes in the developing fetal and neonatal mouse hypothalamus. Int J Dev Neurosci. 2016;53:18–25.
Mucellini AB, Laureano DP, Silveira PP, Sanvitto GL. Maternal and post-natal obesity alters long-term memory and hippocampal molecular signaling of male rat. Brain Res. 2019;1708:138–45.
Wolfrum C, Peleg-Raibstein D. Maternal overnutrition leads to cognitive and neurochemical abnormalities in C57BL/6 mice. Nutr Neurosci. 2019;22:688–99.
Ding Q, Zhao Y, Yang Y, Chen Z. Cognitive Impairment Due to Leptin Withdrawal in Rat Offspring of Dams with Maternal Diet-Induced Obesity. Med Sci Monit Int Med J Exp Clin Res. 2018;24:6208–17.
Zhu C, Han T-L, Zhao Y, Zhou X, Mao X, Qi H, et al. A mouse model of pre-pregnancy maternal obesity combined with offspring exposure to a high-fat diet resulted in cognitive impairment in male offspring. Exp Cell Res. 2018;368:159–66.
Winther G, Elfving B, Müller HK, Lund S, Wegener G. Maternal High-fat Diet Programs Offspring Emotional Behavior in Adulthood. Neuroscience. 2018;388:87–101.
Sullivan EL, Grayson B, Takahashi D, Robertson N, Maier A, Bethea CL, et al. Chronic Consumption of a High-Fat Diet during Pregnancy Causes Perturbations in the Serotonergic System and Increased Anxiety-Like Behavior in Nonhuman Primate Offspring. J Neurosci. 2010;30:3826–30.
Thompson JR, Valleau JC, Barling AN, Franco JG, DeCapo M, Bagley JL et al. Exposure to a High-Fat Diet during Early Development Programs Behavior and Impairs the Central Serotonergic System in Juvenile Non-Human Primates. Front Endocrinol. 2017; 8, https://doi.org/10.3389/fendo.2017.00164.
Desai RA, Manley M, Desai MM, Potenza MN. Gender differences in the association between body mass index and psychopathology. CNS Spectr. 2009;14:372–83.
Winther G, Eskelund A, Bay-Richter C, Elfving B, Müller HK, Lund S, et al. Grandmaternal high-fat diet primed anxiety-like behaviour in the second-generation female offspring. Behav Brain Res. 2019;359:47–55.
Sarker G, Litwan K, Kastli R, Peleg-Raibstein D. Maternal overnutrition during critical developmental periods leads to different health adversities in the offspring: relevance of obesity, addiction and schizophrenia. Sci Rep. 2019; 9, https://doi.org/10.1038/s41598-019-53652-x.
Braff DL, Geyer MA. Sensorimotor gating and schizophrenia. Human and animal model studies. Arch Gen Psychiatry. 1990;47:181–8.
Peleg-Raibstein D, Sarker G, Litwan K, Krämer SD, Ametamey SM, Schibli R, et al. Enhanced sensitivity to drugs of abuse and palatable foods following maternal overnutrition. Transl Psychiatry. 2016;6:e911.
Buffington SA, Prisco GVD, Auchtung TA, Ajami NJ, Petrosino JF, Costa-Mattioli M. Microbial Reconstitution Reverses Maternal Diet-Induced Social and Synaptic Deficits in Offspring. Cell. 2016;165:1762–75.
Derntl B, Habel U. Deficits in social cognition: a marker for psychiatric disorders? Eur Arch Psychiatry Clin Neurosci. 2011;261(Suppl 2):S145–9.
Kang SS, Kurti A, Fair DA, Fryer JD. Dietary intervention rescues maternal obesity induced behavior deficits and neuroinflammation in offspring. J Neuroinflammation. 2014;11:1–12.
Niculescu MD, Lupu DS. High fat diet-induced maternal obesity alters fetal hippocampal development. Int J Dev Neurosci. 2009;27:627–33.
Tozuka Y, Wada E, Wada K. Diet-induced obesity in female mice leads to peroxidized lipid accumulations and impairment of hippocampal neurogenesis during the early life of their offspring. FASEB J. 2009;23:1920–34.
Stachowiak EK, Srinivasan M, Stachowiak MK, Patel MS. Maternal obesity induced by a high fat diet causes altered cellular development in fetal brains suggestive of a predisposition of offspring to neurological disorders in later life. Metab Brain Dis. 2013;28:721–5.
Graf AE, Lallier SW, Waidyaratne G, Thompson MD, Tipple TE, Hester ME, et al. Maternal high fat diet exposure is associated with increased hepcidin levels, decreased myelination, and neurobehavioral changes in male offspring. Brain Behav Immun. 2016;58:369–78.
Janthakhin Y, Rincel M, Costa A-M, Darnaudéry M, Ferreira G. Maternal high-fat diet leads to hippocampal and amygdala dendritic remodeling in adult male offspring. Psychoneuroendocrinology. 2017;83:49–57.
Arikkath J. Molecular mechanisms of dendrite morphogenesis. Front Cell Neurosci. 2012; 6, https://doi.org/10.3389/fncel.2012.00061.
Hatanaka Y, Wada K, Kabuta T. Maternal high-fat diet leads to persistent synaptic instability in mouse offspring via oxidative stress during lactation. Neurochem Int. 2016;97:99–108.
Contu L, Nizari S, Heath CJ, Hawkes CA. Pre- and Post-natal High Fat Feeding Differentially Affects the Structure and Integrity of the Neurovascular Unit of 16-Month Old Male and Female Mice. Front Neurosci. 2019; 13, https://doi.org/10.3389/fnins.2019.01045.
Stolp HB, Dziegielewska KM. Review: Role of developmental inflammation and blood–brain barrier dysfunction in neurodevelopmental and neurodegenerative diseases. Neuropathol Appl Neurobiol. 2009;35:132–46.
Jiang NM, Cowan M, Moonah SN, Petri WA. The Impact of Systemic Inflammation on Neurodevelopment. Trends Mol Med. 2018;24:794–804.
Kim S, Kim H, Yim YS, Ha S, Atarashi K, Tan TG, et al. Maternal gut bacteria promote neurodevelopmental abnormalities in mouse offspring. Nature. 2017;549:528–32.
Knuesel I, Chicha L, Britschgi M, Schobel SA, Bodmer M, Hellings JA, et al. Maternal immune activation and abnormal brain development across CNS disorders. Nat Rev Neurol. 2014;10:643–60.
Kuban KCK, O’Shea TM, Allred EN, Fichorova RN, Heeren T, Paneth N, et al. The Breadth and Type of Systemic Inflammation and the Risk of Adverse Neurological Outcomes in Extremely Low Gestation Newborns. Pediatr Neurol. 2015;52:42–48.
Das UN. Is obesity an inflammatory condition? Nutrition. 2001;17:953–66.
Zaretsky MV, Alexander JM, Byrd W, Bawdon RE. Transfer of Inflammatory Cytokines Across the Placenta. Obstet Gynecol. 2004;103:546–50.
Challier JC, Basu S, Bintein T, Minium J, Hotmire K, Catalano PM, et al. Obesity in Pregnancy Stimulates Macrophage Accumulation and Inflammation in the Placenta. Placenta. 2008;29:274–81.
Edlow AG, Glass RM, Smith CJ, Tran PK, James K, Bilbo S. Placental macrophages: a window into fetal microglial function in maternal obesity. Int J Dev Neurosci. 2019;77:60–68.
Collado MC, Laitinen K, Salminen S, Isolauri E. Maternal weight and excessive weight gain during pregnancy modify the immunomodulatory potential of breast milk. Pediatr Res. 2012;72:77–85.
Panagos P, Vishwanathan R, Penfield-Cyr A, Matthan N, Shivappa N, Wirth M, et al. Breastmilk from obese mothers has pro-inflammatory properties and decreased neuroprotective factors. J Perinatol J Calif Perinat Assoc. 2016;36:284–90.
Lauritzen L, Brambilla P, Mazzocchi A, Harsløf LBS, Ciappolino V, Agostoni C. DHA Effects in Brain Development and Function. Nutrients 2016; 8, https://doi.org/10.3390/nu8010006.
Ozawa Y, Sasaki M, Takahashi N, Kamoshita M, Miyake S, Tsubota K. Neuroprotective Effects of Lutein in the Retina. Curr Pharm Des. 2012;18:51–56.
Cowan M, Petri WAJ. Microglia: immune regulators of neurodevelopment. Front Immunol. 2018; 9, https://doi.org/10.3389/fimmu.2018.02576.
Glendining KA, Fisher LC, Jasoni CL. Maternal high fat diet alters offspring epigenetic regulators, amygdala glutamatergic profile and anxiety. Psychoneuroendocrinology. 2018;96:132–41.
Grissom NM, Herdt CT, Desilets J, Lidsky-Everson J, Reyes TM. Dissociable Deficits of Executive Function Caused by Gestational Adversity are Linked to Specific Transcriptional Changes in the Prefrontal Cortex. Neuropsychopharmacology. 2015;40:1353–63.
Edlow AG, Guedj F, Pennings JLA, Sverdlov D, Neri C, Bianchi DW. Males are from Mars, and females are from Venus: sex-specific fetal brain gene expression signatures in a mouse model of maternal diet-induced obesity. Am J Obstet Gynecol. 2016;214:623.e1–623.e10.
McKee SE, Zhang S, Chen L, Rabinowitz JD, Reyes TM. Perinatal high fat diet and early life methyl donor supplementation alter one carbon metabolism and DNA methylation in the brain. J Neurochem. 2018;145:362–73.
Autry AE, Monteggia LM. Brain-Derived Neurotrophic Factor and Neuropsychiatric Disorders. Pharm Rev. 2012;64:238–58.
Tozuka Y, Kumon M, Wada E, Onodera M, Mochizuki H, Wada K. Maternal obesity impairs hippocampal BDNF production and spatial learning performance in young mouse offspring. Neurochem Int. 2010;57:235–47.
Wu A, Ying Z, Gomez-Pinilla F. The interplay between oxidative stress and brain-derived neurotrophic factor modulates the outcome of a saturated fat diet on synaptic plasticity and cognition. Eur J Neurosci. 2004;19:1699–707.
Santacruz A, Collado MC, García-Valdés L, Segura MT, Martín-Lagos JA, Anjos T, et al. Gut microbiota composition is associated with body weight, weight gain and biochemical parameters in pregnant women. Br J Nutr. 2010;104:83–92.
Soderborg TK, Borengasser SJ, Barbour LA, Friedman JE. Microbial transmission from mothers with obesity or diabetes to infants: an innovative opportunity to interrupt a vicious cycle. Diabetologia. 2016;59:895–906.
Galley JD, Bailey M, Dush CK, Schoppe-Sullivan S, Christian LM. Maternal Obesity Is Associated with Alterations in the Gut Microbiome in Toddlers. PLOS ONE. 2014;9:e113026.
Ma J, Prince AL, Bader D, Hu M, Ganu R, Baquero K, et al. High-fat maternal diet during pregnancy persistently alters the offspring microbiome in a primate model. Nat Commun. 2014;5:1–11.
Kennedy PJ, Murphy AB, Cryan JF, Ross PR, Dinan TG, Stanton C. Microbiome in brain function and mental health. Trends Food Sci Technol. 2016;57:289–301.
Parracho HM, Bingham MO, Gibson GR, McCartney AL. Differences between the gut microflora of children with autistic spectrum disorders and that of healthy children. J Med Microbiol. 2005;54:987–91.
Jiang H, Zhang X, Yu Z, Zhang Z, Deng M, Zhao J, et al. Altered gut microbiota profile in patients with generalized anxiety disorder. J Psychiatr Res. 2018;104:130–6.
Prehn-Kristensen A, Zimmermann A, Tittmann L, Lieb W, Schreiber S, Baving L et al. Reduced microbiome alpha diversity in young patients with ADHD. PLoS ONE. 2018; 13, https://doi.org/10.1371/journal.pone.0200728.
Sanguinetti E, Guzzardi MA, Tripodi M, Panetta D, Selma-Royo M, Zega A, et al. Microbiota signatures relating to reduced memory and exploratory behaviour in the offspring of overweight mothers in a murine model. Sci Rep. 2019;9:1–12.
Money KM, Stanwood GD. Developmental origins of brain disorders: roles for dopamine. Front Cell Neurosci. 2013; 7, https://doi.org/10.3389/fncel.2013.00260.
Gugusheff JR, Bae SE, Rao A, Clarke IJ, Poston L, Taylor PD, et al. Sex and age-dependent effects of a maternal junk food diet on the mu-opioid receptor in rat offspring. Behav Brain Res. 2016;301:124–31.
Kepser L-J, Homberg JR. The neurodevelopmental effects of serotonin: a behavioural perspective. Behav Brain Res. 2015;277:3–13.
Kim T-W, Park H-S. Physical exercise improves cognitive function by enhancing hippocampal neurogenesis and inhibiting apoptosis in male offspring born to obese mother. Behav Brain Res. 2018;347:360–7.
BMI-based Vitamins in Obese Pregnant Women - Full Text View - ClinicalTrials.gov. https://clinicaltrials.gov/ct2/show/NCT02802566 (accessed 14 Apr 2020).
Haghiac M, Yang X, Presley L, Smith S, Dettelback S, Minium J, et al. Dietary Omega-3 Fatty Acid Supplementation Reduces Inflammation in Obese Pregnant Women: A Randomized Double-Blind Controlled Clinical Trial. PLOS ONE. 2015;10:e0137309.
Penfield-Cyr A, Monthe-Dreze C, Smid MC, Sen S. Maternal BMI, Mid-pregnancy Fatty Acid Concentrations, and Perinatal Outcomes. Clin Ther. 2018;40:1659–1667.e1.
Lu D-Y, Tsao Y-Y, Leung Y-M, Su K-P. Docosahexaenoic Acid Suppresses Neuroinflammatory Responses and Induces Heme Oxygenase-1 Expression in BV-2 Microglia: Implications of Antidepressant Effects for Omega-3 Fatty Acids. Neuropsychopharmacology. 2010;35:2238–48.
Patrick RP, Ames BN. Vitamin D and the omega-3 fatty acids control serotonin synthesis and action, part 2: relevance for ADHD, bipolar disorder, schizophrenia, and impulsive behavior. FASEB J. 2015;29:2207–22.
Matsui F, Hecht P, Yoshimoto K, Watanabe Y, Morimoto M, Fritsche K, et al. DHA Mitigates Autistic Behaviors Accompanied by Dopaminergic Change in a Gene/Prenatal Stress Mouse Model. Neuroscience. 2018;371:407–19.
Brei C, Stecher L, Brunner S, Ensenauer R, Heinen F, Wagner PD, et al. Impact of the n-6:n-3 long-chain PUFA ratio during pregnancy and lactation on offspring neurodevelopment: 5-year follow-up of a randomized controlled trial. Eur J Clin Nutr. 2017;71:1114–20.
Ostadrahimi A, Salehi-Pourmehr H, Mohammad-Alizadeh-Charandabi S, Heidarabady S, Farshbaf-Khalili A. The effect of perinatal fish oil supplementation on neurodevelopment and growth of infants: a randomized controlled trial. Eur J Nutr. 2018;57:2387–97.
Asemi Z, Samimi M, Tabassi Z, Naghibi Rad M, Rahimi Foroushani A, Khorammian H, et al. Effect of daily consumption of probiotic yoghurt on insulin resistance in pregnant women: a randomized controlled trial. Eur J Clin Nutr. 2013;67:71–74.
Brantsaeter AL, Myhre R, Haugen M, Myking S, Sengpiel V, Magnus P, et al. Intake of probiotic food and risk of preeclampsia in primiparous women: the Norwegian Mother and Child Cohort Study. Am J Epidemiol. 2011;174:807–15.
Halkjaer SI, Nilas L, Carlsen EM, Cortes D, Halldórsson TI, Olsen SF, et al. Effects of probiotics (Vivomixx®) in obese pregnant women and their newborn: study protocol for a randomized controlled trial. Trials. 2016;17:491.
Acknowledgements
Figure 1 was created using www.biorender.com under a license with Harvard Medical School.
Author information
Authors and Affiliations
Contributions
LT performed the literature review. LT and BTK co-wrote the paper. LT created the Table and Figure.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Tong, L., Kalish, B.T. The impact of maternal obesity on childhood neurodevelopment. J Perinatol 41, 928–939 (2021). https://doi.org/10.1038/s41372-020-00871-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41372-020-00871-0
This article is cited by
-
ABCB1 expression is increased in human first trimester placenta from pregnant women classified as overweight or obese
Scientific Reports (2023)
-
A nationwide, prospective, cohort study on exogenous oxytocin and delays in early child development: the Japan environment and children’s study
European Journal of Pediatrics (2023)
-
Establishment of tissue-resident immune populations in the fetus
Seminars in Immunopathology (2022)
-
Maternal pre-pregnancy BMI associates with neonate local and distal functional connectivity of the left superior frontal gyrus
Scientific Reports (2021)