Abstract
Objective
To determine if neonatal serum biomarkers representing different pathways of injury differ for cases of HIE of unknown cause to gain insight into timing and mechanism of injury.
Study design
In this cohort of all neonates with HIE admitted to our NICU, newborns with sentinel events were compared to those without during the 1st 3 days of life. Discard neonatal blood during the 1st 3 days of life was used for analysis.
Results
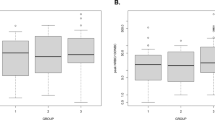
Of 277 babies with HIE treated with whole-body hypothermia, 190 (68.6%) had blood available for biomarker analysis. In total, 71 (37.4%) were born within our system, and 119 (62.6%) were transferred in from outside hospitals. Of these babies, 77 (40.5%) had a sentinel event and 113 (59.6%) had no sentinel event. Although the degree of metabolic acidosis was similar, repeated measures analysis showed that during the initial 3 days of life neonates born with HIE in the absence of sentinel events had 41.4% decreased VEGF (p = 0.027) and 62.5% increased IL-10 serum concentrations (p = 0.005).
Conclusion
These changes indicate that neonatal HIE in the absence of sentinel events is not related to an unrecognized acute intrapartum event and is possibly related to chronic hypoxia of lower severity or recovery from a remote event.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Peebles PJ, Duello TM, Eickhoff JC, McAdams RM. Antenatal and intrapartum risk factors for neonatal hypoxic ischemic encephalopathy. J Perinatol. 2020;40:63–9.
American College of Obstetricians and Gynecologists, American Academy of Pediatrics. Neonatal encephalopathy and neurologic outcome, 2nd ed. Washington DC: American College of Obstetricians and Gynecologists (ACOG); 2014.
Novak CM, Eke AC, Ozen M, Burd I, Graham EM. Risk factors for neonatal hypoxic-ischemic encephalopathy in the absence of sentinel events. Am J Perinatol. 2019;36:27–33.
Kurinczuk JJ, White-Koning M, Badawi N. Epidemiology of neonatal encephalopathy and hypoxic-ischaemic encephalopathy. Early Hum Dev. 2010;86:329–38.
GBD 2013 Mortality and Causes of Death Collaborators. Global, regional, and national age-sex specific all-cause and cause-specific mortality for 240 causes of death, 1990-2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2015;385:117–71.
Martinez-Biarge M, Madero R, Gonzalez A, Quero J, Garcia-Alix A. Perinatal morbidity and risk of hypoxic-ischemic encephalopathy associated with intrapartum sentinel events. Am J Obstet Gynecol. 2012;206:148.e1–e7.
Pfister RH, Bingham P, Edwards EM, Horbar JD, Kenny MJ, Inder T. et al. The Vermont Oxford Neonatal Encephalopathy Registry: rationale, methods, and initial results. BMC Pediatr. 2012;12:84.
Higgins RD, Raju TN, Perlman J, Azzopardi DV, Blackmon LR, Clark RH, et al. Hypothermia and perinatal asphyxia: executive summary of the National Institute of Child Health and Human Development workshop. J Pediatr. 2006;148:170–5.
Graham EM, Ruis KA, Hartman AL, Northington FJ, Fox HE. A systematic review of the role of intrapartum hypoxia-ischemia in the causation of neonatal encephalopathy. Am J Obstet Gynecol. 2008;199:587–95.
Graham EM, Everett AD, Delpech JC, Northington FJ. Blood biomarkers for evaluation of perinatal encephalopathy: state of the art. Curr Opin Pediatr. 2018;30:199–203.
Murray DM. Biomarkers in neonatal hypoxic-ischemic encephalopathy-Review of the literature to date and future directions for research. Handb Clin Neurol. 2019;162:281–93.
Hadlock FP, Harrist RB, Martinez-Poyer J. In utero analysis of fetal growth: a sonographic weight standard. Radiology. 1991;181:129–33.
Shankaran S, Barnes PD, Hintz SR, Laptook AR, Zaterka-Baxter KM, McDonald SA, et al. Brain injury following trial of hypothermia for neonatal hypoxic-ischaemic encephalopathy. Arch Dis Child Fetal Neonatal Ed. 2012;97:F398–404.
Dietrick B, Molloy E, Massaro AN, Strickland T, Zhu J, Slevin M, et al. Plasma and CSF candidate biomarkers of neonatal encephalopathy severity and neurodevelopmental outcomes. J Pediatr. 2020;S0022-3476(20)30832-5. https://doi.org/10.1016/j.jpeds.2020.06.078. [Online ahead of print].
Cheung CY. Vascular endothelial growth factor: possible role in fetal development and placental function. J Soc Gynecol Investig. 1997;4:169–77.
Semenza GL. HIF-1: mediator of physiological and pathophysiological responses to hypoxia. J Appl Physiol. 2000;88:1474–80.
Lv H, Wang Q, Wu S, Yang L, Ren P, Yang Y, et al. Neonatal hypoxic ischemic encephalopathy-related biomarkers in serum and cerebrospinal fluid. Clin Chim Acta. 2015;450:282–97.
Brownbill P, Mills TA, Soydemir DF, Sibley CP. Vasoactivity to and endogenous release of vascular endothelial growth factor in the in vitro perfused human placental lobule from pregnancies complicated by preeclampsia. Placenta. 2008;29:950–5.
Maynard SE, Min JY, Merchan J, Lim KH, Li J, Mondal S, et al. Excess placental soluble fms-like tyrosine kinase 1 (sFlt1) may contribute to endothelial dysfunction, hypertension, and proteinuria in preeclampsia. J Clin Investig. 2003;111:649–58.
Aly H, Hassanein S, Nada A, Mohamed MH, Atef SH, Atiea W. Vascular endothelial growth factor in neonates with perinatal asphyxia. Brain Dev. 2009;31:600–4.
Temburni MK, Jacob MH. New functions for glia in the brain. Proc Natl Acad Sci USA. 2001;98:3631–2.
Mackenzie F, Ruhrberg C. Diverse roles for VEGF-A in the nervous system. Development. 2012;139:1371–80.
McConnell HL, Kersch CN, Woltjer RL, Neuwelt EA. The translational significance of the neurovascular unit. J Biol Chem. 2017;292:762–70.
Dzietko M, Derugin N, Wendland MF, Vexler ZS, Ferriero DM. Delayed VEGF treatment enhances angiogenesis and recovery after neonatal focal rodent stroke. Transl Stroke Res. 2013;4:189–200.
Dvorak HF. Vascular permeability factor/vascular endothelial growth factor: a critical cytokine in tumor angiogenesis and a potential target for diagnosis and therapy. J Clin Oncol. 2002;20:4368–80.
Ni Y, May V, Braas K, Osol G. Pregnancy augments uteroplacental vascular endothelial growth factor gene expression and vasodilator effects. Am J Physiol. 1997;273:H938–44.
Bouloumie A, Schini-Kerth VB, Busse R. Vascular endothelial growth factor up-regulates nitric oxide synthase expression in endothelial cells. Cardiovasc Res. 1999;41:773–80.
Marti HJ, Bernaudin M, Bellail A, Schoch H, Euler M, Petit E, et al. Hypoxia-induced vascular endothelial growth factor expression precedes neovascularization after cerebral ischemia. Am J Pathol. 2000;156:965–76.
Argaw AT, Asp L, Zhang J, Navrazhina K, Pham T, Mariani JN, et al. Astrocyte-derived VEGF-A drives blood-brain barrier disruption in CNS inflammatory disease. J Clin Investig. 2012;122:2454–68.
Carr DJ, Wallace JM, Aitken RP, Milne JS, Mehta V, Martin JF, et al. Uteroplacental adenovirus vascular endothelial growth factor gene therapy increases fetal growth velocity in growth-restricted sheep pregnancies. Hum Gene Ther. 2014;25:375–84.
Swanson AM, Rossi CA, Ofir K, Mehta V, Boyd M, Barker H, et al. Maternal therapy with Ad.VEGF-A165 increases fetal weight at term in a guinea-pig model of fetal growth restriction. Hum Gene Ther. 2016;27:997–1007.
Spencer R, Ambler G, Brodszki J, Diemert A, Figueras F, Gratacos E, et al. EVERREST prospective study: a 6-year prospective study to define the clinical and biological characteristics of pregnancies affected by severe early onset fetal growth restriction. BMC Pregnancy Childbirth. 2017;17:43.
Lennmyr F, Ata KA, Funa K, Olsson Y, Terent A. Expression of vascular endothelial growth factor (VEGF) and its receptors (Flt-1 and Flk-1) following permanent and transient occlusion of the middle cerebral artery in the rat. J Neuropathol Exp Neurol. 1998;57:874–82.
Howell KR, Armstrong J. Vascular Endothelial Growth Factor (VEGF) in neurodevelopmental disorders. Curr Behav Neurosci Rep. 2017;4:299–308.
Licht T, Goshen I, Avital A, Kreisel T, Zubedat S, Eavri R, et al. Reversible modulations of neuronal plasticity by VEGF. Proc Natl Acad Sci USA. 2011;108:5081–6.
Wang YC, Shi CC, Ni H. Clinical significance of serum interleukin 10 levels in neonatal hypoxic ischemic encephalopathy. J Appl Clin Pediatr. 2003;18:442–3.
Garcia JM, Stillings SA, Leclerc JL, Phillips H, Edwards NJ, Robicsek SA, et al. Role of interleukin-10 in acute brain injuries. Front Neurol. 2017;8:244.
Ergenekon E, Gucuyener K, Erbas D, Aral S, Koc E, Atalay Y. Cerebrospinal fluid and serum vascular endothelial growth factor and nitric oxide levels in newborns with hypoxic ischemic encephalopathy. Brain Dev. 2004;26:283–6.
Funding
Funded by NICHD R01HD086058 “Adult Biomarkers in Neonatal Brain Injury and Development”.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Under a license agreement between ImmunArray Ltd. and the Johns Hopkins University, the University and ADE are entitled to royalties on an invention described in this study and discussed in this publication. This arrangement has been reviewed and approved by the Johns Hopkins University in accordance with its conflict of interest policies.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Broni, E.K., Eke, A.C., Vaidya, D. et al. Blood biomarkers for neonatal hypoxic–ischemic encephalopathy in the presence and absence of sentinel events. J Perinatol 41, 1322–1330 (2021). https://doi.org/10.1038/s41372-020-00850-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41372-020-00850-5
This article is cited by
-
Serum brain injury biomarkers are gestationally and post-natally regulated in non-brain injured neonates
Pediatric Research (2023)
-
Biomarkers in neonatal encephalopathy: new approaches and ongoing questions
Pediatric Research (2022)