Abstract
Objective
Discrepancies between physician and parent neonatal prognostic expectations are common. Optimism bias is a possible explanation.
Study design
Parents interpreted hypothetical neonatal prognoses in an online survey.
Results
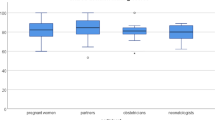
Good prognoses tended to be interpreted accurately, while poor prognoses were interpreted as less than the stated value. One-third of participants consistently overstated survival for the three lowest prognoses, compared to the sample as a whole. Three significant predictors of such optimistic interpretations were single-parent status (OR 0.39; 95% CI 0.2–0.75; p = 0.005), African-American descent (OR 3.78; 95% CI 1.63–8.98; p = 0.002) and the belief that physicians misrepresented prognoses (OR 3.11; 95% CI 1.47–6.65; p = 0.003). Participants’ explanations echoed research on optimism bias in clinical and decision science studies.
Conclusion
Participants accepted positive prognoses for critically ill neonates, but reinterpreted negative ones as being unduly pessimistic demonstrating optimism bias.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Boyd EA, Lo B, Evans LR, Malvar G, Apatira L, Luce JM, et al. “It’s not just what the doctor tells me:” factors that influence surrogate decision-makers’ perceptions of prognosis. Crit Care Med. 2010;38:1270–5.
Bastek TK, Richardson DK, Zupancic JA, Burns JP. Prenatal consultation practices at the border of viability: a regional survey. Pediatrics. 2005;116:407–13.
Haward MF, Gaucher N, Payot A, Robson K, Janvier A. Personalized decision making: practical recommendations for antenatal counseling for fragile neonates. Clin Perinatol. 2017;44:429–45.
Boss RD, Hutton N, Sulpar LJ, West AM, Donohue PK. Values parents apply to decision-making regarding delivery room resuscitation for high-risk newborns. Pediatrics. 2008;122:583–9.
Janvier A, Lorenz JM, Lantos JD. Antenatal counselling for parents facing an extremely preterm birth: limitations of the medical evidence. Acta Paediatr. 2012;101:800–4.
Haward MF, Janvier A, Lorenz JM, Fischhoff B. Counseling parents at risk of delivery of an extremely premature infant: differing strategies. AJOB Empir Bioeth. 2017;8:243–52.
Wolfe J, Klar N, Grier HE, Duncan J, Salem-Schatz S, Emanuel EJ, et al. Understanding of prognosis among parents of children who died of cancer: impact on treatment goals and integration of palliative care. JAMA. 2000;284:2469–75.
Cox CE, Martinu T, Sathy SJ, Clay AS, Chia J, Gray AL, et al. Expectations and outcomes of prolonged mechanical ventilation. Crit Care Med. 2009;37:2888–904.
Sung L, Klaassen RJ, Dix D, Pritchard S, Yanofsky R, Ethier M, et al. Parental optimism in poor prognosis pediatric cancers. Psychooncology. 2009;18:783–8.
Mack JW, Cook EF, Wolfe J, Grier HE, Cleary PD, Weeks JC. Understanding of prognosis among parents of children with cancer: parental optimism and the parent-physician interaction. J Clin Oncol. 2007;25:1357–62.
Ford D, Zapka JG, Gebregziabher M, Hennessy W, Yang C. Investigating critically ill patients’ and families’ perceptions of likelihood of survival. J Palliat Med. 2009;12:45–52.
White DB, Ernecoff N, Buddadhumaruk P, Hong S, Weissfeld L, Curtis JR, et al. Prevalence of and factors related to discordance about prognosis between physicians and surrogate decision makers of critically Ill patients. JAMA. 2016;315:2086–94.
de Wit S, Donohue PK, Shepard J, Boss RD. Mother-clinician discussions in the neonatal intensive care unit: agree to disagree? J Perinatol. 2013;33:278–81.
Lee Char SJ, Evans LR, Malvar GL, White DB. A randomized trial of two methods to disclose prognosis to surrogate decision makers in intensive care units. Am J Respir Crit Care Med. 2010;182:905–9.
Sisk BA, Kang TI, Mack JW. How parents of children with cancer learn about their children’s prognosis. Pediatrics. 2018;141:e20172241.
Boss RD, Lemmon ME, Arnold RM, Donohue PK. Communicating prognosis with parents of critically ill infants: direct observation of clinician behaviors. J Perinatol. 2017;37:1224–9.
White DB, Carson S, Anderson W, Steingrub J, Bird G, Curtis JR, et al. A multicenter study of the causes and consequences of optimistic expectations about prognosis by surrogate decision-makers in ICUs. Crit Care Med. 2019;47:1184–93.
Zier LS, Sottile PD, Hong SY, Weissfield LA, White DB. Surrogate decision makers’ interpretation of prognostic information: a mixed-methods study. Ann Intern Med. 2012;156:360–6.
Fischhoff B, Broomell SB. Judgment and decision making. Annu Rev Psychol. 2020;71:331–55.
Kahneman D. Thinking, fast and slow. New York: Farrar Straus & Giroux; 2011.
Lerner JS, Li Y, Valdesolo P, Kassam KS. Emotion and decision making. Annu Rev Psychol. 2015;66:799–823.
Feudtner C, Walter JK, Faerber JA, Hill DL, Carroll KW, Mollen CJ, et al. Good-parent beliefs of parents of seriously ill children. JAMA Pediatr. 2015;169:39–47.
Fischhoff B, Barnato AE. Value awareness: a new goal for end-of-life decision making. MDM Policy Pract. 2019;4:2381468318817523.
Weinstein ND. Optimistic biases about personal risks. Science. 1989;246:1232–3.
Weinstein ND. Unrealistic optimism about future life events. J Pers Soc Psychol. 1980;39:806–20.
Weinstein ND. Unrealistic optimism about susceptibility to health problems. J Behav Med. 1982;5:441–60.
Radcliffe NM, Klein WMP. Dispositional, comparative and unrealistic optimism. differential relations with the knowledge and processing of risk information and beliefs about person risk. Pers Soc Psychol Bull. 2002;28:836–46.
Quadrel MJ, Fischhoff B, Davis W. Adolescent (in)vulnerability. Am Psychol. 1993;48:102–16.
Weeks JC, Cook EF, O’Day SJ, Peterson LM, Wenger N, Reding D, et al. Relationship between cancer patients’ predictions of prognosis and their treatment preferences. JAMA. 1998;279:1709–14.
Haward MF, Murphy RO, Lorenz JM. Message framing and perinatal decisions. Pediatrics. 2008;122:109–18.
Gamble VN. Under the shadow of Tuskegee: African Americans and health care. Am J Public Health. 1997;87:1773–8.
Institute of Medicine. Unequal treatment: confronting racial and ethnic disparities in health care. Washington, DC: National Academics Press; 2003.
Walker RJ, Strom Williams J, Egede LE. Influence of race, ethnicity and social determinants of health on diabetes outcomes. Am J Med Sci. 2016;351:366–73.
Patel D, Cohen ED, Barnato AE. The effect of framing on surrogate optimism bias: a simulation study. J Crit Care. 2016;32:85–8.
Reder EA, Serwint JR. Until the last breath: exploring the concept of hope for parents and health care professionals during a child’s serious illness. Arch Pediatr Adolesc Med. 2009;163:653–7.
Arnolds M, Xu L, Hughes P, McCoy J, Meadow W. Worth a try? describing the experiences of families during the course of care in the neonatal intensive care unit when the prognosis is poor. J Pediatr. 2018;196:116–22.e3.
Geros-Willfond KN, Ivy SS, Montz K, Bohan SE, Torke AM. Religion and spirituality in surrogate decision making for hospitalized older adults. J Relig Health. 2016;55:765–77.
Robinson MR, Thiel MM, Backus MM, Meyer EC. Matters of spirituality at the end of life in the pediatric intensive care unit. Pediatrics. 2006;118:e719–29.
Sharot T. The optimism bias. Curr Biol. 2011;21:R941–5.
Blumenthal-Barby JS, Ubel PA. In defense of “Denial”: difficulty knowing when beliefs are unrealistic and whether unrealistic beliefs are bad. Am J Bioeth. 2018;18:4–15.
Janvier A, Leblanc I, Barrington KJ. Nobody likes premies: the relative value of patients’ lives. J Perinatol. 2008;28:821–6.
Janvier A, Mercurio MR. Saving vs creating: perceptions of intensive care at different ages and the potential for injustice. J Perinatol. 2013;33:333–5.
Barnato AE, Arnold RM. The effect of emotion and physician communication behaviors on surrogates’ life-sustaining treatment decisions: a randomized simulation experiment. Crit Care Med. 2013;41:1686–91.
Haward MF, Murphy RO, Lorenz JM. Default options and neonatal resuscitation decisions. J Med Ethics. 2012;38:713–8.
Guillén Ú, Mackley A, Laventhal N, Kukuro S, Christ L, Derrick M, et al. Evaluating the use of a decision aid for parents facing extremely premature delivery: a randomized trial. J Pediatr. 2019;209:52–60.e1.
Moore GP, Lemyre B, Daboval T, Ding S, Dunn S, Akiki S, et al. Field testing of decision coaching with a decision aid for parents facing extreme prematurity. J Perinatol. 2017;37:728–34.
Guillen U, Kirpalani H. Ethical implications of the use of decision aids for antenatal counseling at the limits of gestational viability. Semin Fetal Neonatal Med. 2018;23:25–9.
Peerzada JM, Richardson DK, Burns JP. Delivery room decision-making at the threshold of viability. J Pediatr. 2004;145:492–8.
Blanco F, Suresh G, Howard D, Soll R. Ensuring accurate knowledge of prematurity outcomes for prenatal counseling. Pediatrics. 2005;115:e478–87.
Zupancic J, Kirpalani H, Barrett J, Stewart S, Gafni A, Streiner D. et al. Characterising doctor–patient communication in counselling for impending preterm delivery. Arch Dis Child Fetal Neonatal Ed. 2002;87:F113–7.
Dupont-Thibodeau A, Barrington KJ, Farlow B, Janvier A. End-of-life decisions for extremely low-gestational-age infants: why simple rules for complicated decisions should be avoided. Semin Perinatol. 2014;38:31–7.
Lemmon ME, Huffstetler H, Barks MC, Kirby C, Katz M, Ubel P, et al. Neurologic outcome after prematurity: perspectives of parents and clinicians. Pediatrics. 2019;144:e20183819.
Acknowledgements
The authors would like to thank Deborah Campbell, MD and the Division of Neonatology at Montefiore Children’s Hospital Albert Einstein College of Medicine for their support of this research.
Funding
Division of Neonatology fellow research funds.
Author information
Authors and Affiliations
Contributions
All authors contributed in the design, data analysis, and paper development and revision.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Nayak, B., Moon, JY., Kim, M. et al. Optimism bias in understanding neonatal prognoses. J Perinatol 41, 445–452 (2021). https://doi.org/10.1038/s41372-020-00773-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41372-020-00773-1
This article is cited by
-
Elternzentrierte ethische Entscheidungsfindung für Frühgeborene im Grenzbereich der Lebensfähigkeit – Reflexion über die Bedeutung probabilistischer Prognosen als Entscheidungsgrundlage
Ethik in der Medizin (2022)
-
Relationship between physician prognosis bias and parental optimism bias
Journal of Perinatology (2021)
-
Response to comment on “Optimism bias in understanding neonatal prognoses”
Journal of Perinatology (2021)