Abstract
Objective
To compare the characteristics and outcomes of neonates with mild hypoxic-ischemic encephalopathy (HIE) who received hypothermia versus standard care.
Study design
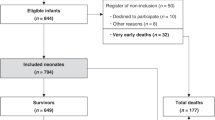
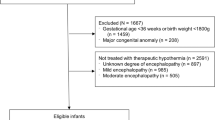
We conducted a retrospective cohort study of neonates ≥35 weeks’ gestation and ≥1800 g admitted with a diagnosis of Sarnat stage 1 encephalopathy. We evaluated length of hospital stay, duration of ventilation, evidence of brain injury on MRI, and neonatal morbidities.
Results
Of 1089 eligible neonates, 393 (36%) received hypothermia and 595 (55%) had neuroimaging. The hypothermia group was more likely to be outborn, born via C-section, had lower Apgar scores, and required extensive resuscitation. They had longer durations of stay (9 vs. 6 days, P < 0.001), respiratory support (3 vs. 2 days, P < 0.001), but lower odds of brain injury on MRI (adjusted odds ratio 0.33, 95% CI: 0.22–0.52) compared with standard care group.
Conclusion
Despite prolongation of hospital stay, hypothermia may be potentially beneficial in neonates with mild HIE; however, selection bias cannot be ruled out.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Executive summary: Neonatal encephalopathy and neurologic outcome, second edition. Report of the American College of Obstetricians and Gynecologists’ Task Force on Neonatal Encephalopathy. Obstet Gynecol. 2014;123:896–901.
Wassink G, Gunn ER, Drury PP, Bennet L, Gunn AJ. The mechanisms and treatment of asphyxial encephalopathy. Front Neurosci. 2014;8:40.
Polderman KH. Mechanisms of action, physiological effects, and complications of hypothermia. Crit Care Med. 2009;37 Suppl 7:S186–202.
Gunn AJ, Bennet L, Gunning MI, Gluckman PD, Gunn TR. Cerebral hypothermia is not neuroprotective when started after postischemic seizures in fetal sheep. Pediatr Res. 1999;46:274–80.
Shankaran S, Laptook AR, Pappas A, McDonald SA, Das A, Tyson JE, et al. Effect of depth and duration of cooling on death or disability at age 18 months among neonates with hypoxic-ischemic encephalopathy: a randomized clinical trial. JAMA. 2017;318:57–67.
Jacobs SE, Berg M, Hunt R, Tarnow-Mordi WO, Inder TE, Davis PG. Cooling for newborns with hypoxic ischaemic encephalopathy. Cochrane Database Syst Rev. 2013;1:Cd003311.
Edwards AD, Brocklehurst P, Gunn AJ, Halliday H, Juszczak E, Levene M, et al. Neurological outcomes at 18 months of age after moderate hypothermia for perinatal hypoxic ischaemic encephalopathy: synthesis and meta-analysis of trial data. BMJ. 2010;340:c363.
Tagin MA, Woolcott CG, Vincer MJ, Whyte RK, Stinson DA. Hypothermia for neonatal hypoxic ischemic encephalopathy: an updated systematic review and meta-analysis. Arch Pediatr Adolesc Med. 2012;166:558–66.
Zhang W, Ma J, Danzeng Q, Tang Y, Lu M, Kang Y. Safety of moderate hypothermia for perinatal hypoxic-ischemic encephalopathy: a meta-analysis. Pediatr Neurol. 2017;74:51–61.
Robertson CM, Finer NN, Grace MG. School performance of survivors of neonatal encephalopathy associated with birth asphyxia at term. J Pediatr. 1989;114:753–60.
Murray DM, O’Connor CM, Ryan CA, Korotchikova I, Boylan GB. Early EEG grade and outcome at 5 years after mild neonatal hypoxic ischemic encephalopathy. Pediatrics. 2016;138:e20160659.
van Handel M, Swaab H, de Vries LS, Jongmans MJ. Behavioral outcome in children with a history of neonatal encephalopathy following perinatal asphyxia. J Pediatr Psychol. 2010;35:286–95.
El-Dib M, Inder TE, Chalak LF, Massaro AN, Thoresen M, Gunn AJ. Should therapeutic hypothermia be offered to babies with mild neonatal encephalopathy in the first 6 h after birth? Pediatr Res. 2019;85:442–8.
Canadian Neonatal Network. The Canadian Neonatal Network Abstractor’s Manual v.3.4.1. Toronto:CNN; 2019.
Shah PS, Seidlitz W, Chan P, Yeh S, Musrap N, Lee SK. Internal audit of the Canadian Neonatal Network Data Collection System. Am J Perinatol. 2017;34:1241–9.
Sarnat HB, Sarnat MS. Neonatal encephalopathy following fetal distress. A clinical and electroencephalographic study. Arch Neurol. 1976;33:696–705.
Kracer B, Hintz SR, Van Meurs KP, Lee HC. Hypothermia therapy for neonatal hypoxic ischemic encephalopathy in the state of California. J Pediatr. 2014;165:267–73.
Massaro AN, Murthy K, Zaniletti I, Cook N, DiGeronimo R, Dizon M, et al. Short-term outcomes after perinatal hypoxic ischemic encephalopathy: a report from the Children’s Hospitals Neonatal Consortium HIE focus group. J Perinatol. 2015;35:290–6.
Gagne-Loranger M, Sheppard M, Ali N, Saint-Martin C, Wintermark P. Newborns referred for therapeutic hypothermia: association between initial degree of encephalopathy and severity of brain injury (what about the newborns with mild encephalopathy on admission?). Am J Perinatol. 2016;33:195–202.
Oliveira V, Singhvi DP, Montaldo P, Lally PJ, Mendoza J, Manerkar S, et al. Therapeutic hypothermia in mild neonatal encephalopathy: a national survey of practice in the UK. Arch Dis Child Fetal Neonatal Ed. 2018;103:F388–90.
Wusthoff CJ, Clark CL, Glass HC, Shimotake TK, Schulman J, Bonifacio SL. Cooling in neonatal hypoxic-ischemic encephalopathy: practices and opinions on minimum standards in the state of California. J Perinatol. 2018;38:54–8.
Soll RF. Cooling for newborns with hypoxic ischemic encephalopathy. Neonatology. 2013;104:260–2.
Saw CL, Rakshasbhuvankar A, Rao S, Bulsara M, Patole S. Current practice of therapeutic hypothermia for mild hypoxic ischemic encephalopathy. J Child Neurol. 2019;34:402–9.
DuPont TL, Chalak LF, Morriss MC, Burchfield PJ, Christie L, Sanchez PJ. Short-term outcomes of newborns with perinatal acidemia who are not eligible for systemic hypothermia therapy. J Pediatr. 2013;162:35–41.
Mehta S, Joshi A, Bajuk B, Badawi N, McIntyre S, Lui K. Eligibility criteria for therapeutic hypothermia: from trials to clinical practice. J Paediatr Child Health. 2017;53:295–300.
Takenouchi T, Cuaycong M, Ross G, Engel M, Perlman JM. Chain of brain preservation–a concept to facilitate early identification and initiation of hypothermia to infants at high risk for brain injury. Resuscitation. 2010;81:1637–41.
Walsh BH, Neil J, Morey J, Yang E, Silvera MV, Inder TE, et al. The frequency and severity of magnetic resonance imaging abnormalities in infants with mild neonatal encephalopathy. J Pediatr. 2017;187:26–33.e21.
Prempunpong C, Chalak LF, Garfinkle J, Shah B, Kalra V, Rollins N, et al. Prospective research on infants with mild encephalopathy: the PRIME study. J Perinatol. 2018;38:80–5.
Lally PJ, Montaldo P, Oliveira V, Soe A, Swamy R, Bassett P, et al. Magnetic resonance spectroscopy assessment of brain injury after moderate hypothermia in neonatal encephalopathy: a prospective multicentre cohort study. Lancet Neurol. 2019;18:35–45.
Thompson CM, Puterman AS, Linley LL, Hann FM, van der Elst CW, Molteno CD, et al. The value of a scoring system for hypoxic ischaemic encephalopathy in predicting neurodevelopmental outcome. Acta Paediatr. 1997;86:757–61.
Chalak LF, Adams-Huet B, Sant’Anna G. A total sarnat score in mild hypoxic-ischemic encephalopathy can detect infants at higher risk of disability. J Pediatr. 2019. https://doi.org/10.1016/j.jpeds.2019.06.026.
Graham EM, Everett AD, Delpech JC, Northington FJ. Blood biomarkers for evaluation of perinatal encephalopathy: state of the art. Curr Opin Pediatr. 2018;30:199–203.
Lorch SA. Determining the optimal neonatal care for preterm infants in the era of personalized medicine. Pediatrics. 2017.https://doi.org/10.1542/peds.2016-2442.
Yue JK, Vassar MJ, Lingsma HF, Cooper SR, Okonkwo DO, Valadka AB, et al. Transforming research and clinical knowledge in traumatic brain injury pilot: multicenter implementation of the common data elements for traumatic brain injury. J Neurotrauma. 2013;30:1831–44.
Acknowledgements
The authors gratefully acknowledge all site investigators and data abstractors of the Canadian Neonatal Network (CNN). We thank the staff at the Maternal-infant Care (MiCare) Research Centre at Mount Sinai Hospital, Toronto, Ontario, for organizational support of CNN. We also thank EWY, of MiCare, for assistance with the statistical analyses; Heather McDonald-Kinkaid, PhD, of MiCare, for editorial support in preparing this manuscript; and Ms Rosanna Yankanah, MSc, CCRP Manager, Clinical Research for assistance with the ethics submission.
Canadian Neonatal Network Investigators
Prakesh S. Shah8, Jaideep Kanungo9, Joseph Ting10, Zenon Cieslak11, Rebecca Sherlock12, Ayman Abou Mehrem13, Jennifer Toye14, Carlos Fajardo15, Zarin Kalapesi16, Jaya Bodani16, Koravangattu Sankaran17, Sibasis Daspal17, Mary Seshia18, Deepak Louis18, Ruben Alvaro19, Amit Mukerji20, Orlando Da Silva21, Mohammad Adie22, Kyong-Soon Lee23, Michael Dunn24, Brigitte Lemyre25, Faiza Khurshid26, Ermelinda Pelausa27, Keith Barrington28, Anie Lapoint28, Guillaume Ethier28, Christine Drolet29, Bruno Piedboeuf29, Martine Claveau30, Marc Beltempo30, Valerie Bertelle31, Edith Masse31, Roderick Canning32, Hala Makary33, Cecil Ojah34, Luis Monterrosa34, Julie Emberley35, Jehier Afifi36, Andrzej Kajetanowicz37, Shoo K. Lee38
Funding
Organizational support for the Canadian Neonatal Network was provided by the Maternal-infant Care (MiCare) Research Centre at Mount Sinai Hospital in Toronto, Ontario, Canada. MiCare is supported by a team grant from the Canadian Institutes of Health Research (CIHR) (CTP 87518), by the Ontario Ministry of Health and Long-Term Care, and by the participating hospitals. PSS holds an Applied Research Chair in Reproductive and Child Health Services and Policy Research from the CIHR (APR-126340).
Author information
Authors and Affiliations
Consortia
Contributions
IRG conceptualized and designed the study, designed the data collection instruments, collected data, carried out the initial analyses, and drafted, reviewed, and revised the paper. HW reviewed the initial study proposal and research ethics application, contributed to the acquisition and interpretation of data, and reviewed and revised the paper. PW, KM, SS, and DL contributed to the interpretation of data and critically reviewed and revised the paper. EWY contributed to the analysis and interpretation of data and revised the paper. PSS conceptualized and designed the study, coordinated and supervised the data collection, and critically reviewed and revised the paper for important intellectual content. As corresponding author, PSS confirms that he has had full access to the data in the study and final responsibility for the decision to submit for publication.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The members of the Canadian Neonatal Network Investigators are listed below the Acknowledgements.
Supplementary information
Rights and permissions
About this article
Cite this article
Goswami, I.R., Whyte, H., Wintermark, P. et al. Characteristics and short-term outcomes of neonates with mild hypoxic-ischemic encephalopathy treated with hypothermia. J Perinatol 40, 275–283 (2020). https://doi.org/10.1038/s41372-019-0551-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41372-019-0551-2
This article is cited by
-
Unconjugated bilirubin is correlated with the severeness and neurodevelopmental outcomes in neonatal hypoxic-ischemic encephalopathy
Scientific Reports (2023)
-
Variations in care of neonates during therapeutic hypothermia: call for care practice bundle implementation
Pediatric Research (2023)
-
Mild hypoxic-ischemic encephalopathy (HIE): timing and pattern of MRI brain injury
Pediatric Research (2022)
-
Brain injury following mild hypoxic-ischemic encephalopathy in neonates–Ten-year experience in a tertiary perinatal center
Journal of Perinatology (2022)
-
Outcomes of infants with hypoxic-ischemic encephalopathy during COVID-19 pandemic lockdown in Canada: a cohort study
Child's Nervous System (2022)