Abstract
Objective
To evaluate clinical outcomes associated with extubation timing among extremely preterm neonates.
Design/Methods
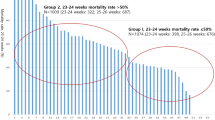
Neonates <26 weeks’ GA admitted to four tertiary neonatal centers were included if they met predetermined extubation criteria within first postnatal week and classified into early extubation (≤24 h; exposure group) and delayed extubation (>24 h; control group) after meeting extubation criteria. Patients with known severe IVH and/or significant PDA prior to meeting extubation criteria were excluded.
Results
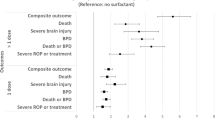
Of 197 included infants, 75 were in exposure group. Survival without BPD (aOR 1.26; 95% CI 0.62–2.56; P = 0.52) and survival without severe IVH (aOR 1.98; 95% CI 0.93–4.23; P = 0.08) were not different, adjusted for GA, SNAP, number of surfactant doses and center.
Conclusions
Extubation within 24 h of meeting extubation criteria in neonates <26 weeks’ GA was not associated with survival without BPD or survival without severe IVH. However, confounding by indication cannot be ruled out without a prospective trial.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Stoll BJ, Hansen NI, Bell EF, Shankaran S, Laptook AR, Walsh MC, et al. Neonatal outcomes of extremely preterm infants from the NICHD Neonatal Research Network. Pediatrics. 2010;126:443–56.
Walsh MC, Morris BH, Wrage LA, Vohr BR, Poole WK, Tyson JE, et al. Extremely low birthweight neonates with protracted ventilation: mortality and 18-month neurodevelopmental outcomes. J Pediatr. 2005;146:798–804.
Chawla S, Natarajan G, Shankaran S, Carper B, Brion LP, Keszler M, et al. Markers of successful extubation in extremely preterm infants, and morbidity after failed extubation. J Pediatr. 2017;189:113–9.
Berger J, Mehta P, Bucholz E, Dziura J, Bhandari V. Impact of early extubation and reintubation on the incidence of bronchopulmonary dysplasia in neonates. Am J Perinatol. 2014;31:1063–72.
Perlman JM, Volpe JJ. Intraventricular hemorrhage in extremely small premature infants. Am J Dis Child. 1986;140:1122–4.
McNamara PJ, Sehgal A. Towards rational management of the patent ductus arteriosus: the need for disease staging. Arch Dis Child Fetal Neonatal Ed. 2007;92:F424–7.
Robbins M, Trittmann J, Martin E, Reber KM, Nelin L, Shepherd E. Early extubation attempts reduce length of stay in extremely preterm infants even if re-intubation is necessary. J Neonatal Perinat Med. 2015;8:91–7.
Jensen EA, DeMauro SB, Kornhauser M, Aghai ZH, Greenspan JS, Dysart KC. Effects of multiple ventilation courses and duration of mechanical ventilation on respiratory outcomes in extremely low-birth-weight infants. JAMA Pediatr. 2015;169:1011–7.
Dumpa V, Northrup V, Bhandari V. Type and timing of ventilation in the first postnatal week is associated with bronchopulmonary dysplasia/death. Am J Perinatol. 2011;28:321–30.
Danan C, Durrmeyer X, Brochard L, Decobert F, Benani M, Dassieu G. A randomized trial of delayed extubation for the reduction of reintubation in extremely preterm infants. Pediatr Pulmonol. 2008;43:117–24.
Ballabh P. Intraventricular hemorrhage in premature infants: mechanism of disease. Pediatr Res. 2010;67:1–8.
Funding
None specific to this study. Dr Amit Mukerji is supported by a Research Early Career Award from Hamilton Health Sciences Foundation (2019–2021). Dr Prakesh Shah is supported by an Applied Research Chair funding from the Canadian Institutes of Health Research.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Mukerji, A., Razak, A., Aggarwal, A. et al. Early versus delayed extubation in extremely preterm neonates: a retrospective cohort study. J Perinatol 40, 118–123 (2020). https://doi.org/10.1038/s41372-019-0495-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41372-019-0495-6
This article is cited by
-
Peri-extubation settings in preterm neonates: a systematic review and meta-analysis
Journal of Perinatology (2024)
-
Weaning and extubation from neonatal mechanical ventilation: an evidenced-based review
BMC Pulmonary Medicine (2022)