Abstract
Objective(s)
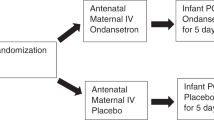
To compare short-term treatment outcomes of opioid pharmacotherapy for neonatal opioid withdrawal syndrome (NOWS).
Study design
PubMed/MEDLINE, Embase, PsycINFO, and The Cochrane Library were searched from inception through September 30, 2018. Primary outcome was treatment duration (LOT). Secondary outcomes included hospitalization duration (LOS) and rate of adjunct drug needed (RAD).
Results
Of 753 publications, 11 studies met inclusion criteria. There was no difference in LOT (WMD −1.39 [−5.79 to –3.01] days, I2 82%) or LOS (WMD −1.48 [−5.75 to –2.79] days, I2 92%) between morphine and methadone. RAD with morphine was higher (RR 1.51 [1.35–1.69], I2 0%). Buprenorphine was associated with shorter LOT (WMD 7.70 [0.88–14.53] days, I2 76%) and LOS (WMD 5.61 [−0.01 to –11.24] days, I2 60%) compared with morphine, in addition to methadone according to two cohort studies.
Conclusions
Methadone had superior primary treatment success compared with morphine. Buprenorphine was associated with the shortest overall durations of treatment and hospitalization.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Tolia VN, Patrick SW, Bennett MM, Murthy K, Sousa J, Smith PB, et al. Increasing incidence of the neonatal abstinence syndrome in U.S. neonatal ICUs. N Engl J Med. 2015;372:2118–26.
Patrick SW, Davis MM, Lehman CU, Cooper WO. Increasing incidence and geographic distribution of neonatal abstinence syndrome: United States 2009 to 2012. J Perinatol: Off J Calif Perinat Assoc. 2015;35:667.
Kocherlakota P. Neonatal abstinence syndrome. Pediatrics. 2014;134:e547–61.
Osborn DA, Jeffery HE. Cole MJ, Opiate treatment for opiate withdrawal in newborn infants. Cochrane Datab Syst Rev. 2010;10:Cd002059.
Osborn DA, Jeffery HE, Cole MJ. Sedatives for opiate withdrawal in newborn infants. Cochrane Datab Syst Rev. 2010;10:Cd002053.
Hudak ML, Tan RC. Neonatal drug withdrawal. Pediatrics. 2012;129:e540–60.
Bogen DL, Whalen BL, Kair LR, Vining M, King BA. Wide variation found in care of opioid-exposed newborns. Acad Pedia. 2017;17:374–80.
Crocetti MT, Amin DD, Jansson LM. Variability in the evaluation and management of opiate-exposed newborns in Maryland. Clin Pediatr. 2007;46:632–5.
Sarkar S, Donn SM. Management of neonatal abstinence syndrome in neonatal intensive care units: a national survey. J Perinatol: Off J Calif Perinat Assoc. 2006;26:15–7.
Mehta A, Forbes KD, Kuppala VS. Neonatal abstinence syndrome management from prenatal counseling to postdischarge follow-up care: results of a national survey. Hosp Pediatr. 2013;3:317–23.
Disher T, Gullickson C, Singh B, Cameron C, Boulos L, Beaubien L, et al. Pharmacological treatments for neonatal abstinence syndrome: a systematic review and network meta-analysis. JAMA Pediatr. 2019;173:234–43.
Wan X, Wang W, Liu J, Tong T. Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. BMC Med Res Method. 2014;14:135.
Sutter MB. Morphine versus methadone for opiate exposed infants with neonatal abstinence syndrome. NLM identifier: NCT02851303 https://clinicaltrials.gov/ct2/show/NCT02851303?type=Intr&cond=Neonatal+Abstinence+Syndrome&rank=14.
Martin G. Comparison of buprenorphine to morphine in treatment of neonatal abstinence Syndrome (NAS). NLM identifier: NCT01708707 https://clinicaltrials.gov/ct2/show/NCT01708707?type=Intr&cond=Neonatal+Abstinence+Syndrome&rank=11.
Kushnir A. Treatment of neonatal abstinence syndrome with clonidine versus morphine as primary therapy. NLM identifier: NCT03092011 https://clinicaltrials.gov/ct2/show/NCT03092011?type=Intr&cond=Neonatal+Abstinence+Syndrome&draw=2&rank=1.
Gauda E. Sublingual buprenorphine treatment for neonatal abstinence syndrome - Pilot Study. NLM identifier: NCT02249026 https://clinicaltrials.gov/ct2/show/NCT02249026?type=Intr&cond=Neonatal+Abstinence+Syndrome&rank=25.
Davis JM, Lester B. Improving outcomes in neonatal abstinence syndrome. NLM identifier: NCT01958476 https://clinicaltrials.gov/ct2/show/NCT01958476type=Intr&cond=Neonatal+Abstinence+Syndrome&rank=6.
Brooks S. Methadone Demonstration Project. NLM identifier: NCT03134703 https://clinicaltrials.gov/ct2/show/NCT03134703?type=Intr&cond=Neonatal+Abstinence+Syndrome&rank=20.
Bada HS. Non-opiate treatment after prenatal opiate exposure to prevent postnatal injury to the young brain (No-POPPY). NLM identifier: NCT03396588 https://clinicaltrials.gov/ct2/show/NCT03396588?type=Intr&cond=Neonatal+Abstinence+Syndrome&rank=18.
Hall ES, Rice WR, Folger AT, Wexelblatt SL. Comparison of neonatal abstinence syndrome treatment with sublingual buprenorphine versus conventional opioids. Am J Perinatol. 2018;35:405–12.
Burke S, Beckwith AM. Morphine versus methadone treatment for neonatal withdrawal and impact on early infant development. Glob Pediatr health. 2017;4:2333794x17721128.
Brown MS, Hayes MJ, Thornton LM. Methadone versus morphine for treatment of neonatal abstinence syndrome: a prospective randomized clinical trial. J Perinatol: Off J Calif Perinat Assoc. 2015;35:278–83.
Young ME, Hager SJ, Spurlock D Jr. Retrospective chart review comparing morphine and methadone in neonates treated for neonatal abstinence syndrome. Am J Health-Syst Pharm: AJHP: Off J Am Soc Health-Syst Pharm. 2015;72(23Suppl 3):S162–7.
Hall ES, Wexelblatt SL, Crowley M, Grow JL, Jasin LR, Klebanoff MA, et al. A multicenter cohort study of treatments and hospital outcomes in neonatal abstinence syndrome. Pediatrics. 2014;134:e527–34.
Patrick SW, Kaplan HC, Passarella M, Davis MM, Lorch SA. Variation in treatment of neonatal abstinence syndrome in US children’s hospitals, 2004–2011. J Perinatol: Off J Calif Perinat Assoc. 2014;34:867–72.
Lainwala S, Brown ER, Weinschenk NP, Blackwell MT, Hagadorn JI. A retrospective study of length of hospital stay in infants treated for neonatal abstinence syndrome with methadone versus oral morphine preparations. Adv Neonatal Care: Off J Natl Assoc Neonatal Nurses. 2005;5:265–72.
Kraft WK, Adeniyi-Jones SC, Chervoneva I, Greenspan JS, Abatemarco D, Kaltenbach K, et al. Buprenorphine for the treatment of the neonatal abstinence syndrome. New Engl J Med. 2017;376:2341–8.
Kraft WK, Dysart K, Greenspan JS, Gibson E, Kaltenbach K, Ehrlich ME. Revised dose schema of sublingual buprenorphine in the treatment of the neonatal opioid abstinence syndrome. Addiction. 2011;106:574–80.
Kraft WK, Gibson E, Dysart K, Damle VS, Larusso JL, Greenspan JS, et al. Sublingual buprenorphine for treatment of neonatal abstinence syndrome: a randomized trial. Pediatrics. 2008;122:e601–7.
Hall ES, Isemann BT, Wexelblatt SL, Meinzen-Derr J, Wiles JR, Harvey S, et al. A cohort comparison of buprenorphine versus methadone treatment for neonatal abstinence syndrome. J Pediatr. 2016;170:39–44.e1.
Bada HS, Sithisarn T, Gibson J, Garlitz K, Caldwell R, Capilouto G, et al. Morphine versus clonidine for neonatal abstinence syndrome. Pediatrics. 2015;135:e383–91.
Esmaeili A, Keinhorst AK, Schuster T, Beske F, Schlosser R, Bastanier C. Treatment of neonatal abstinence syndrome with clonidine and chloral hydrate. Acta Paediatr. 2010;99:209–14.
Devlin LA, Lau T, Radmacher PG. Decreasing total medication exposure and length of stay while completing withdrawal for neonatal abstinence syndrome during the neonatal hospital stay. Front Pedia. 2017;5:216.
Surran B, Visintainer P, Chamberlain S, Kopcza K, Shah B, Singh R. Efficacy of clonidine versus phenobarbital in reducing neonatal morphine sulfate therapy days for neonatal abstinence syndrome. A prospective randomized clinical trial. J Perinatol: Off J Calif Perinat Assoc. 2013;33:954–9.
Coyle MG, Ferguson A, Lagasse L, Liu J, Lester B. Neurobehavioral effects of treatment for opiate withdrawal. Arch Dis Child Fetal neonatal Ed. 2005;90:F73–4.
Coyle MG, Ferguson A, Lagasse L, Oh W, Lester B. Diluted tincture of opium (DTO) and phenobarbital versus DTO alone for neonatal opiate withdrawal in term infants. J Pediatr. 2002;140:561–4.
Agthe AG, Kim GR, Mathias KB, Hendrix CW, Chavez-Valdez R, Jansson L, et al. Clonidine as an adjunct therapy to opioids for neonatal abstinence syndrome: a randomized, controlled trial. Pediatrics. 2009;123:e849–56.
Davis JM, Shenberger J, Terrin N, Breeze JL, Hudak M, Wachman EM, et al. Comparison of safety and efficacy of methadone vs morphine for treatment of neonatal abstinence syndrome: a randomized clinical trial. JAMA Pedia. 2018;172:741–8.
Tolia VN, Murthy K, Bennett MM, Greenberg RG, Benjamin DK, Smith PB, et al. Morphine vs methadone treatment for infants with neonatal abstinence syndrome. J Pediatr. 2018;203:185–9.
Jones HE, Kaltenbach K, Heil SH, Stine SM, Coyle MG, Arria AM, et al. Neonatal abstinence syndrome after methadone or buprenorphine exposure. N Engl J Med. 2010;363:2320–31.
Kraft WK, Stover MW, Davis JM. Neonatal abstinence syndrome: pharmacologic strategies for the mother and infant. Semin Perinatol. 2016;40:203–12.
Boumeester NJ, AB, Tibboel D, et al. Developmental pharmacokinetics of morphine and its metabolites in neonates, infants, ad young children. Br J Anaesth. 2004;92:208–17.
Kraft WK. Buprenorphine in neonatal abstinence syndrome. Clin Pharmacol Ther. 2018;103:112–9.
Blume HK, Garrison MM, Christakis DA. Neonatal seizures: treatment and treatment variability in 31 United States pediatric hospitals. J Child Neurol. 2009;24:148–54.
Trescot AM, Datta S, Lee M, Hansen H. Opioid pharmacology. Pain Physician. 2008;11(2 Suppl):S133–53.
Corr TE, Hollenbeak CS. The economic burden of neonatal abstinence syndrome in the United States. Addiction. 2017;112:1590–9.
MacMillan KDL, Rendon CP, Verma K, Riblet N, Washer DB, Volpe Holmes A. Association of rooming-in with outcomes for neonatal abstinence syndrome: a systematic review and meta-analysis. JAMA Pedia. 2018;172:345–51.
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Lee, J.J., Chen, J., Eisler, L. et al. Comparative effectiveness of opioid replacement agents for neonatal opioid withdrawal syndrome: a systematic review and meta-analysis. J Perinatol 39, 1535–1545 (2019). https://doi.org/10.1038/s41372-019-0437-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41372-019-0437-3