Abstract
Objective
To characterize the risk of bloodstream (BSI) and urinary tract infection (UTI) and describe antibiotic use in infants with congenital diaphragmatic hernia (CDH) requiring extracorporeal membrane oxygenation (ECMO).
Study design
The Children’s Hospitals Neonatal Database was queried for infants with CDH and ECMO treatment from 2010 to 2016. The outcomes included BSI, UTI, and antimicrobial medication. Member institutions completed a survey on infection practices.
Result
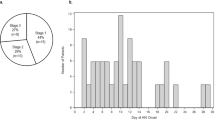
Eighteen of the 338 patients identified (5.3%) had ≥1 BSI during their ECMO course. The likelihood of BSI increased with time: 1.2/1000 ECMO days; 0.6% (2/315) in the first week and rising to 14.6/1000; 8.6% (5/58) after 21 days (p = 0.002). More than 95% of patients received antibiotics each week on ECMO.
Conclusions
Confirmed BSI is rare in infants with CDH treated with ECMO in the first week, but increases with the duration of ECMO. Use of antibiotics was extensive and did not correspond to infection frequency.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Biffi S, Di Bella S, Scaravilli V, Peri AM, Grasselli G, Alagna L, et al. Infections during extracorporeal membrane oxygenation: epidemiology, risk factors, pathogenesis and prevention. Int J Antimicrob Agents. 2017;50:9–16.
Cashen K, Reeder R, Dalton HJ, Berg RA, Shanley TP, Newth CJL, et al. Acquired infection during neonatal and pediatric extracorporeal membrane oxygenation. Perfusion. 2018;33:472–82.
Bizzarro MJ, Conrad SA, Kaufman DA, Rycus P. Extracorporeal life support organization task force on infections EMO. Infections acquired during extracorporeal membrane oxygenation in neonates, children, and adults. Pediatr Critic Care Med. 2011;12:277–81.
Barbaro RP, Paden ML, Guner YS, Raman L, Ryerson LM, Alexander P, et al. Pediatric Extracorporeal Life Support Organization Registry International Report 2016. ASAIO J 2017;63:456–63.
Thiagarajan RR, Barbaro RP, Rycus PT, McMullan DM, Conrad SA, Fortenberry JD, et al. Extracorporeal Life Support Organization Registry International Report 2016. ASAIO J. 2017;63:60–7.
Prodhan P, Stroud M, El-Hassan N, Peeples S, Rycus P, Brogan TV, et al. Prolonged extracorporeal membrane oxygenator support among neonates with acute respiratory failure: a review of the Extracorporeal Life Support Organization Registry. ASAIO J. 2014;60:63–9.
Butler DF, Lee B, Molitor-Kirsch E, Newland JG. Extracorporeal membrane oxygenation-associated bloodstream infections in children. Pediatr Infect Dis J. 2017;36:346–7.
Castagnola E, Gargiullo L, Loy A, Tatarelli P, Caviglia I, Bandettini R, et al. Epidemiology of infectious complications during extracorporeal membrane oxygenation in children: a single-center experience in 46 runs. Pediatr Infect Dis J. 2018;37:624–6.
Paden ML, Rycus PT, Thiagarajan RR, Registry E. Update and outcomes in extracorporeal life support. Semin Perinatol. 2014;38:65–70.
Rehder KJ, Turner DA, Cheifetz IM. Extracorporeal membrane oxygenation for neonatal and pediatric respiratory failure: an evidence-based review of the past decade (2002-2012). Pediatr Critic Care Med. 2013;14:851–61.
Vogel AM, Lew DF, Kao LS, Lally KP. Defining risk for infectious complications on extracorporeal life support. J Pediatr Surg. 2011;46:2260–4.
Haricharan RN, Barnhart DC, Cheng H, Delzell E. Identifying neonates at a very high risk for mortality among children with congenital diaphragmatic hernia managed with extracorporeal membrane oxygenation. J Pediatr Surg. 2009;44:87–93.
O’Horo JC, Cawcutt KA, De Moraes AG, Sampathkumar P, Schears GJ. The evidence base for prophylactic antibiotics in patients receiving extracorporeal membrane oxygenation. ASAIO J. 2016;62:6–10.
Glater-Welt LB, Schneider JB, Zinger MM, Rosen L, Sweberg TM. Nosocomial bloodstream infections in patients receiving extracorporeal life support: variability in prevention practices: a survey of the extracorporeal life support organization members. J Intensive Care Med. 2015;31:654–69.
Kao LS, Fleming GM, Escamilla RJ, Lew DF, Lally KP. Antimicrobial prophylaxis and infection surveillance in extracorporeal membrane oxygenation patients: a multi-institutional survey of practice patterns. ASAIO J. 2011;57:231–8.
Dalton HJ, Raman L. Management of pediatric respiratory failure patient on ECMO. In: Brogan TV, Lequier L, Lorusso R, MacLaren G, Peek GJ The ELSO red book. 5th ed. Michigan: Extracorporeal Life Support Organization Ann Arbor; 2017. p. 272
Canadian Congenital Diaphragmatic Hernia C, Puligandla PS, Skarsgard ED, Offringa M, Adatia I, Baird R, et al. Diagnosis and management of congenital diaphragmatic hernia: a clinical practice guideline. CMAJ. 2018;190:E103–E12.
Snoek KG, Reiss IK, Greenough A, Capolupo I, Urlesberger B, Wessel L, et al. Standardized postnatal management of infants with congenital diaphragmatic hernia in Europe: The CDH EURO Consortium Consensus - 2015 Update. Neonatology. 2016;110:66–74.
Murthy K, Porta NFM, Pallotto EK, Rintoul N, Keene S, Chicoine L, et al. Predicting risk of infection in infants with congenital diaphragmatic hernia. J Pediatr. 2018;203:101–7.
Cotten CM. Adverse consequences of neonatal antibiotic exposure. Curr Opin Pediatr. 2016;28:141–9.
Cantey JB, Wozniak PS, Pruszynski JE, Sanchez PJ. Reducing unnecessary antibiotic use in the neonatal intensive care unit (SCOUT): a prospective interrupted time-series study. Lancet Infect Dis. 2016;16:1178–84.
Keene S, Murthy K, Pallotto E, Brozanski B, Gien J, Zaniletti I. et al. Acquired infection and antimicrobial utilization during initial NICU hospitalization in infants with congenital diaphragmatic hernia. Pediatr Infect Dis J. 2018;37:469–74.
Murthy K, Dykes FD, Padula MA, Pallotto EK, Reber KM, Durand DJ, et al. The Children’s Hospitals Neonatal Database: an overview of patient complexity, outcomes and variation in care. J Perinatol. 2014;34:582–6.
Massaro AN, Murthy K, Zaniletti I, Cook N, DiGeronimo R, Dizon ML, et al. Intercenter Cost Variation for Perinatal Hypoxic-Ischemic Encephalopathy in the Era of Therapeutic Hypothermia. J Pediatr. 2016;173:76–83.
Horbar JD, Carpenter JH, Badger GJ, Kenny MJ.Soll RF, Morrow KA, et al. Mortality and neonatal morbidity among infants 501 to 1500 grams from 2000 to 2009. 2012;129:1019–26.
Simonsen KA, Anderson-Berry AL, Delair SF, Davies HD. Early-onset neonatal sepsis. Clin Microbiol Rev. 2014;27:21–47.
Stockmann C, Spigarelli MG, Campbell SC, Constance JE, Courter JD, Thorell EA, et al. Considerations in the pharmacologic treatment and prevention of neonatal sepsis. Paediatr Drugs. 2014;16:67–81.
Kuzniewicz MW, Puopolo KM, Fischer A, Walsh EM, Li S, Newman TB, et al. A quantitative, risk-based approach to the management of neonatal early-onset sepsis. JAMA Pediatr. 2017;171:365–71.
Escobar GJ, Puopolo KM, Wi S, Turk BJ, Kuzniewicz MW, Walsh EM, et al. Stratification of risk of early-onset sepsis in newborns ≥34 weeks’ gestation. Pediatrics. 2014;133:30–6.
ELSO ID TASK FORCE Recommendation Summary 2012. https://www.elso.org/Portals/0/Files/ELSO-ID-Task-Force-Recommendations-Summary.pdf.
Kutlesa M, Santini M, Krajinovic V, Papic N, Novokmet A, Josipovic Mraovic R, et al. Nosocomial blood stream infections in patients treated with venovenous extracorporeal membrane oxygenation for acute respiratory distress syndrome. Minerva Anestesiol. 2017;83:493–501.
Piazza AJ, Brozanski B, Provost L, Grover TR, Chuo J, Smith JR, et al. SLUG bug: quality improvement with orchestrated testing leads to NICU CLABSI reduction. Pediatrics. 2016;137. https://doi.org/10.1542/peds.2014-3642.
Fisher D, Cochran KM, Provost LP, Patterson J, Bristol T, Metzguer K, et al. Reducing central line-associated bloodstream infections in North Carolina NICUs. Pediatrics. 2013;132:e1664–71.
van den Anker JN. How to optimize the evaluation and use of antibiotics in neonates. Early Hum Dev. 2014;90(Suppl 1):S10–2.
Murthy K, Pallotto EK, Gien J, Brozanski BS, Porta NF, Zaniletti I, et al. Predicting death or extended length of stay in infants with congenital diaphragmatic hernia. J Perinatol. 2016;36:654–9.
Acknowledgements
JA, DD (ex officio), FD (ex officio), JE, KM, MP, EP, TG, and BB, and AP, KR, and BS are members of the Children’s Hospitals Neonatal Consortium, Inc. (www.thechnc.org). For more information, please contact: support@thechnc.org. We are indebted to the following institutions that serve the infants and their families, and these institutions also have invested in and continue to participate in the Children’s Hospital’s Neonatal Database (CHND). The site sponsors/contributors for the CHND are also included.
Children’s Hospitals Neonatal Consortium’s (CHNC) Congenital Diaphragmatic Hernia Focus Group
Jeanette Asselin, David Durand (ex officio), Francine Dykes (ex officio), Jacquelyn Evans, Karna Murthy, Michael Padula, Eugenia Pallotto, Theresa Grover, Beverly Brozanski, and Anthony Piazza, Kristina Reber and Billie Short are members of the Children’s Hospitals Neonatal Consortium, Inc., (site: thechnc.org). For more information, please contact: support@thechnc.org
We are indebted to the following institutions that serve the infants and their families, and these institutions also have invested in and continue to participate in the Children’s Hospital’s Neonatal Database (CHND). The site sponsors/contributors for the CHND are also included:
Children's Healthcare of Atlanta, Atlanta, GA (Francine Dykes, Anthony Piazza); Children’s Healthcare of Atlanta at Scottish Rite (Gregory Sysyn); Children’s Hospital of Alabama, Birmingham, AL (Carl Coghill, Allison Black); Le Bonheur Children’s Hospital, Memphis, TN (Ramasubbareddy Dhanireddy); Children’s Hospital Boston, Boston, MA (Anne Hansen, Tanzeema Houssain); Ann & Robert H. Lurie Children’s Hospital of Chicago, Chicago, IL (Karna Murthy, Gustave Falciglia); Cincinnati Children’s Hospital, Cincinnati, OH (Beth Haberman, Brenda Poindexter, Amy Nathan, Kristin Nelson, Paul Kingma, Stefanie Riddle, Stephanie Merhar, Heather Kaplan); Nationwide Children’s Hospital, Columbus, OH (Kristina Reber); Children's Medical Center, Dallas, TX (Rashmin Savani, Luc Brion, Noorjahan Ali); Children’s Hospital Colorado, Aurora, CO (Theresa Grover); Children’s Hospital of Michigan, Detroit, MI (Girija Natarajan); Cook Children’s Health Care System, Fort Worth, TX (Jonathan Nedrelow, Annie Chi, Yvette Johnson); Texas Children's Hospital, Houston, TX (Gautham Suresh); Riley Children’s Hospital, Indianapolis, IN (William Engle, Lora Simpson, Gregory Sokol); Children’s Mercy Hospitals & Clinics, Kansas City, MO (Eugenia Pallotto); Arkansas Children's Hospital, Little Rock, AR (Robert Lyle, Becky Rogers); Children’s Hospital Los Angeles, Los Angeles, CA (Steven Chin, Rachel Chapman); American Family Children’s Hospital, Madison, WI (Jamie Limjoco, Lori Haack); Children's Hospital & Research Center Oakland, Oakland, CA (David Durand, Jeanette Asselin, Art D’Harlingue, Priscilla Joe) ; The Children's Hospital of Philadelphia, Philadelphia, PA (Jacquelyn Evans, Michael Padula, David Munson); St. Christopher’s Hospital for Children, Philadelphia, PA (Suzanne Touch); Children’s Hospital of Pittsburgh of UPMC, Pittsburgh, PA (Beverly Brozanski); St. Louis Children's Hospital, St Louis, MO (Tasmin Najaf, Rakesh Rao, Amit Mathur); All Children's Hospital, St. Petersburg, FL (Victor McKay); Rady Children’s Hospital, San Diego, CA (Mark Speziale, Brian Lane, Laural Moyer); Children's National Medical Center, Washington, DC (Billie Short); AI DuPont Hospital for Children, Wilmington, DE (Kevin Sullivan); Primary Children’s Medical Center, Salt Lake City, UT (Con Yee Ling, Shrena Patel); Children’s Hospital of Wisconsin, Milwaukee, WI (Michael Uhing, Ankur Datta); Children’s Hospital of Omaha (Lynne Willett, Nicole Birge); Florida Hospital for Children (Rajan Wadhawan); Seattle Children’s Hospital, Seattle, WA (Elizabeth Jacobsen-Misbe, Robert DiGeronimo, Zeenia Billimoria); Hospital for Sick Children, Toronto, ON (Kyong-Soon Lee); Children’s Hospital Orange County, Los Angeles, CA (Michel Mikhael, Irfan Ahmad).
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Conflict of interest
The authors have no competing financial interests to declare in relation to the work described. The authors have no sources of funding to report for this work. One author, KM is a member and Chair of the Board of the Childrens’ Hospital Neonatal Consortium (CHNC), a 501-3-c organization. Other than statistical support and consultation, the Childrens’ Hospital Association (CHA) had no input in the design of the project, the aims, or the decision whether to submit this paper for publication. The remaining authors delare that they have no conflicts of interest.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Members of the Children’s Hospitals Neonatal Consortium’s (CHNC) Congenital Diaphragmatic Hernia Focus Group are listed below the Acknowledgements.
Rights and permissions
About this article
Cite this article
Keene, S., Grover, T.R., Murthy, K. et al. Extracorporeal membrane oxygenation and bloodstream infection in congenital diaphragmatic hernia. J Perinatol 39, 1384–1391 (2019). https://doi.org/10.1038/s41372-019-0435-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41372-019-0435-5