Abstract
Objective
To develop and test an Objective Structured Clinical Examination to evaluate the use of shared decision-making (SDM) in periviable counseling among fourth-year OB/GYN residents.
Methods
Residents counseled a standardized patient presenting with preterm premature rupture of membranes at 23 weeks’ gestation. Braddock’s 9-item measure of SDM was adapted to a 10-item scoring rubric; rating each: 0 (absent), 1 (partial), or 2 (complete).
Results
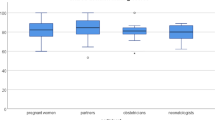
Twenty-six residents participated. All provided “complete” discussions of the clinical issue and “complete” or ‘partial’ ratings for informing the woman of her prognosis (62 and 38%, respectively) and addressing her role in decision-making (42 and 50%). Discussions of her goals and preferences were often absent (69 and 62%). Only 42% discussed uncertainties.
Conclusion
Critical elements of SDM related to a woman’s values, goals and preferences were not explored when counseling about periviable delivery. Training in SDM is needed to advance communication skills for complex clinical decision-making.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Meadow W, Lagatta J, Andrews B, Lantos J. The mathematics of morality for neonatal resuscitation. Clin Perinatol. 2012;39:941–56.
Eden LM, Callister LC. Parent involvement in end-of-life care and decision making in the newborn intensive care unit. An integrative review. J Perinat Educ. 2010;19:29–39.
Moro TT, Kavanaugh K, Savage TA, Reyes MR, Kimura RE, Bhat R. Parent decision making for life support decisions for extremely premature infants. From the prenatal through end-of-life period. J Perinat Neonatal Nurs. 2011;25:52–60.
Raju TN, Mercer BM, Burchfield DJ, Joseph GF. Periviable birth: Executive summary of a joint workshop by the Eunice Kennedy Shriver National Institute of Child Health and Human Development, Society for Maternal-Fetal Medicine, American Academy of Pediatrics, and American College of Obstetricians and Gynecologists. J Perinatol. 2014;34:333–42.
Deregnier RA, Ballard R, O’shea TM, Piecuch R, Walsh M, Aschner JL. Neonatal—perinatal medicine fellowship training in long-term outcomes of neonatal intensive care unit graduates. J Perinatol. 2005;25:423–25.
The Obstetrics and Gynecology Milestone Project. J Grad Med Educ. 2014;6:129–43.
Zayyan M. Objective structured clinical examination: the assessment of choice. Oman Med J. 2011;26:219–22.
Winkel AF, Gillespie C, Hiruma MT, Goepfert AR, Zabar S, Szyld D. Test of integrated professional skills: objective structured clinical examination/simulation hybrid assessment of obstetrics-gynecology residents’ skill integration. J Grad Med Educ. 2014;6:117–22.
Thomson O’Brien MA, Freemantle N, Oxman AD, Wolf F, Davis DA, Herrin J. Continuing education meetings and workshops: effects on professional practice and health care outcomes. Cochrane Database Syst Rev. 2001;2:CD003030.
Prislin MD, Fitzpatrick CF, Lie D, Giglio M, Radecki S, Lewis E. Use of an objective structured clinical examination in evaluating student performance. Fam Med. 1998;30:338–44.
Braddock CH III, Edwards KA, Hasenberg NM, Laidley TL, Levinson W. Informed decision making in outpatient practice: time to get back to basics. J Amer Med Assoc. 1999;282:2313–20.
Braddock CH III, Hudak PL, Feldman JJ, Bereknyei S, Frankel RM, Levinson W. Surgery is certainly one good option: quality and time-efficiency of informed decision-making in surgery. J Bone Joint Surg Am. 2008;90:1830–38.
Salyers MP, Matthias MS, Fukui S, Holter MC, Collins L, Rose N, et al. A coding system to measure elements of shared decision making during psychiatric visits. Psychiatr Serv. 2012;63:779–84.
Back AL, Arnold RM, Baile WF, Tulsky JA, Fryer-Edwards K. Approaching difficult communication tasks in oncology. CA Cancer J Clin. 2005;55:164–77.
Austin CA, Mohottige D, Sudore RL, Smith AK, Hanson LC. Tools to promote shared decision making in serious illness: a systematic review. JAMA Intern Med. 2015;175:1213–21.
O’Connor AM, Bennett CL, Stacey D, Barry M, Col NF, Eden KB, et al. Decision aids for people facing health treatment or screening decisions. Cochrane Database Syst Rev. 2009;8:CD001431.
Guillén Ú, Suh S, Munson D, et al. Development and pretesting of a decision-aid to use when counseling parents facing imminent extreme premature delivery. J Pediatr. 2012;160:382–7.
Moore GP, Lemyre B, Daboval T, Ding S, Dunn S, Akiki S, et al. Field testing of decision coaching with a decision aid for parents facing extreme prematurity. J Perinatol. 2017;37:728–34.
Elwyn G, Frosch D, Thomson R, Joseph-Williams N, Lloyd A, Kinnersley P, et al. Shared decision making: a model for clinical practice. J Gen Intern Med. 2012;27:1361–67.
Epstein RM, Alper BS, Quill TE. Communicating evidence for participatory decision making. JAMA. 2004;291:2359–66.
McKeown RE, Reininger BM, Martin M, Hoppmann RA. Shared decision making: views of first-year residents and clinic patients. Acad Med. 2002;77:438–45.
Heath J, Kohn R, Sargsyan Z, Alba G, Miloslavsky E, Barbash I, et al. Simulation curriculum in internal medicine: decision-making training for interns focusing on acute clinical scenarios in critical care. MedEdPORTAL. 2015;11:10061.
Posner G, Worth K, Nakajima A. An introduction to the management of labor and delivery—a simulation-based obstetrics workshop for medical students. MedEdPORTAL. 2012;8:9128.
Rodriguez A, Fisher J, Broadfoot K, Hurt K. A challenging obstetric communication experience for undergraduate medical education using standardized patients and student self-reflection. MedEdPORTAL. 2015;11:10121.
Moore G, Ferretti E, Rohde K, Muirhead P, Daboval T. Neonatal ethics teaching program—scenario-oriented learning in ethics: critically ill newborn in the neonatal intensive care unit. MedEdPORTAL. 2015;11:10083.
Zheng A, Macauley K, Namba J, Hutchins S, Sweeney K, Wallace P, et al. A large scale interprofessional simulation experience for medical, nursing, and pharmacy students. MedEdPORTAL. 2015;11:10018.
Acknowledgements
This work can be attributed to the Department of Obstetrics & Gynecology, Indiana University School of Medicine, Indianapolis, USA
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Tucker Edmonds, B., McKenzie, F., Panoch, J. et al. Evaluating shared decision-making in periviable counseling using objective structured clinical examinations. J Perinatol 39, 857–865 (2019). https://doi.org/10.1038/s41372-019-0366-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41372-019-0366-1