Abstract
Objective
To determine normative values for heart rate patterns in healthy fetuses.
Methods
This research is from the Safe Passage Study conducted by the Prenatal Alcohol and SIDS and Stillbirth (PASS) Network. A standardized protocol assessed fetal heart rate (FHR), heart rate variability (HRV), and movement from 1655 fetuses at three-time points during gestation (20–24 weeks, 28–32 weeks, 34–38 weeks gestation).
Results
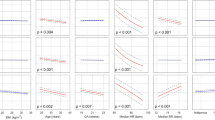
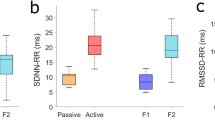
FHR decreased while HRV increased over gestation. At the latter two ages, males had significantly lower FHR than females while there were no sex differences in FHR at 20–24 weeks. When accounting for the fetal state during late gestation (34–28 weeks), we found that males had significantly lower FHR than females in the active fetal state only.
Conclusion
Results demonstrate significant state, gestational age, and sex-related changes in cardiac activity, somatic activity, and autonomic function as the fetus approaches birth.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
Amorim-Costa C, Costa-Santos C, Ayres-de-Campos D, Bernardes J. Longitudinal evaluation of computerized cardiotocographic parameters throughout pregnancy in normal fetuses: a prospective cohort study. Acta Obstet Gynecol Scand. 2016;95:1143–52.
Amorim-Costa C, Cruz J, Ayres-de-Campos D, Bernardes J. Gender-specific reference charts for cardiotocographic parameters throughout normal pregnancy: a retrospective cross-sectional study of 9701 fetuses. Eur J Obstet Gynecol Reprod Biol. 2016;199:102–7.
Park MI, Hwang JH, Cha KJ, Park YS, Koh SK. Computerized analysis of fetal heart rate parameters by gestational age. Int J Gynaecol Obstet. 2001;74:157–64.
Pillai M, James D. The development of fetal heart rate patterns during normal pregnancy. Obstet Gynecol. 1990;76(5 Pt 1):812–6.
Snijders RJ, McLaren R, Nicolaides KH. Computer-assisted analysis of fetal heart rate patterns at 20-41 weeks’ gestation. Fetal Diagn Ther. 1990;5:79–83.
Van Leeuwen P, Cysarz D, Edelhauser F, Gronemeyer D. Heart rate variability in the individual fetus. Auton Neurosci. 2013;178:24–8.
DiPietro JA, Costigan KA, Shupe AK, Pressman EK, Johnson TR. Fetal neurobehavioral development: associations with socioeconomic class and fetal sex. Dev Psychobiol. 1998;33:79–91.
Rajendra Acharya U, Paul Joseph K, Kannathal N, Lim CM, Suri JS. Heart rate variability: a review. Med Biol Eng Comput. 2006;44:1031–51.
Renou P, Newman W, Wood C. Autonomic control of fetal heart rate. Am J Obstet Gynecol. 1969;105:949–53.
Spyridou K, Chouvarda I, Hadjileontiadis L, Maglaveras N. The effect of cigarette smoking on fetal heart rate tracing during pregnancy. J Perinat Med. 2017;45:403–11.
Lucchini M, Pini N, Fifer WP, Burtchen N, Signorini MG. Entropy information of cardiorespiratory dynamics in neonates during sleep. Entropy (Basel). 2017;19:225.
Frasch MG, Zwiener U, Hoyer D, Eiselt M. Autonomic organization of respirocardial function in healthy human neonates in quiet and active sleep. Early Hum Dev. 2007;83:269–77.
Allister L, Lester BM, Carr S, Liu J. The effects of maternal depression on fetal heart rate response to vibroacoustic stimulation. Dev Neuropsychol. 2001;20:639–51.
Monk C, Fifer WP, Myers MM, Sloan RP, Trien L, Hurtado A. Maternal stress responses and anxiety during pregnancy: effects on fetal heart rate. Dev Psychobiol. 2000;36:67–77.
Zeskind PS, Gingras JL. Maternal cigarette-smoking during pregnancy disrupts rhythms in fetal heart rate. J Pediatr Psychol. 2006;31:5–14.
Lehtovirta P, Forss M, Kariniemi V, Rauramo I. Acute effects of smoking on fetal heart-rate variability. Br J Obstet Gynaecol. 1983;90:3–6.
Morrow RJ, Ritchie JW, Bull SB. Maternal cigarette smoking: the effects on umbilical and uterine blood flow velocity. Am J Obstet Gynecol. 1988;159:1069–71.
Quigley ME, Sheehan KL, Wilkes MM, Yen SS. Effects of maternal smoking on circulating catecholamine levels and fetal heart rates. Am J Obstet Gynecol. 1979;133:685–90.
Péterfi I, Kellényi L, Péterfi L, Szilágyi A. The short-term effect of smoking on fetal ECG. The Journal of Maternal-Fetal & Neonatal Medicine. 2019 Mar 4;32:724–33.
McLeod W, Brien J, Loomis C, Carmichael L, Probert C, Patrick J. Effect of maternal ethanol ingestion on fetal breathing movements, gross body movements, and heart rate at 37 to 40 weeks’ gestational age. Am J Obstet Gynecol. 1983;145:251–7.
Silva PD, Miller KD, Madden J, Keegan KA Jr. Abnormal fetal heart rate pattern associated with severe intrapartum maternal ethanol intoxication. A case report. J Reprod Med. 1987;32:144–6.
Mulder EJ, Morssink LP, van der Schee T, Visser GH. Acute maternal alcohol consumption disrupts behavioral state organization in the near-term fetus. Pediatr Res. 1998;44:774–9.
Pruett D, Waterman EH, Caughey AB. Fetal alcohol exposure: consequences, diagnosis, and treatment. Obstet Gynecol Surv. 2013;68:62–9.
May LE, Glaros A, Yeh HW, Clapp JF 3rd, Gustafson KM. Aerobic exercise during pregnancy influences fetal cardiac autonomic control of heart rate and heart rate variability. Early Hum Dev. 2010;86:213–7.
Myers MM, Fifer W, Haiken J, Stark RI. Relationships between breathing activity and heart rate in fetal baboons. Am J Physiol. 1990;258(6 Pt 2):R1479–85.
Stark RI, Daniel SS, Kim YI, Leung K, Myers MM, Tropper PJ. Patterns of fetal breathing in the baboon vary with EEG sleep state. Early Hum Dev. 1994;38:11–26.
DiPietro JA, Costigan KA, Voegtline KM. Studies in Fetal Behavior: Revisited, Renewed, and Reimagined. Monogr Soc Res Child Dev. 2015;80:1–94. vii
Williams IA, Tarullo AR, Grieve PG, Wilpers A, Vignola EF, Myers MM, et al. Fetal cerebrovascular resistance and neonatal EEG predict 18-month neurodevelopmental outcome in infants with congenital heart disease. Ultrasound Obstet Gynecol. 2012;40:304–9.
Dipietro JA, Irizarry RA, Hawkins M, Costigan KA, Pressman EK. Cross-correlation of fetal cardiac and somatic activity as an indicator of antenatal neural development. Am J Obstet Gynecol. 2001;185:1421–8.
Nijhuis JG, Prechtl HF, Martin CB Jr. Bots RS. Are there behavioural states in the human fetus? Early Hum Dev. 1982;6:177–95.
Fleisher LA, Dipietro JA, Johnson TR, Pincus S. Complementary and non-coincident increases in heart rate variability and irregularity during fetal development. Clin Sci (Lond). 1997;92:345–9.
Lange S, Van Leeuwen P, Geue D, Hatzmann W, Gronemeyer D. Influence of gestational age, heart rate, gender and time of day on fetal heart rate variability. Med Biol Eng Comput. 2005;43:481–6.
Nijhuis IJ, ten Hof J, Mulder EJ, Nijhuis JG, Narayan H, Taylor DJ, et al. Fetal heart rate in relation to its variation in normal and growth retarded fetuses. Eur J Obstet Gynecol Reprod Biol. 2000;89:27–33.
DiPietro JA, Voegtline KM. The gestational foundation of sex differences in development and vulnerability. Neuroscience. 2017;342:4–20.
Patrick J, Campbell K, Carmichael L, Natale R, Richardson B. Patterns of human fetal breathing during the last 10 weeks of pregnancy. Obstet Gynecol. 1980;56:24–30.
Roodenburg PJ, Wladimiroff JW, van Es A, Prechtl HF. Classification and quantitative aspects of fetal movements during the second half of normal pregnancy. Early Hum Dev. 1991;25:19–35.
ten Hof J, Nijhuis IJ, Nijhuis JG, Narayan H, Taylor DJ, Visser GH, et al. Quantitative analysis of fetal general movements: methodological considerations. Early Hum Dev. 1999;56:57–73.
Sobell LCSM. Timeline follow-back. New York: Springer Science; 1992.
Brown RABE, Sales SD, Whiteley JA, Evans DM, Miller IW. Reliability and validity of a smoking timeline follow-back interview. Psychol Addict Behav. 1998;12:101.
Acknowledgements
The authors gratefully acknowledge the cooperation of the study participants, PASS investigators, the PASS Steering Committee Chairman Gary D.V. Hankins, MD, and members of the NICHD advisory safety monitoring board: Elizabeth Thom, PhD (Chair); Reverend Phillip Cato, PhD; James W. Collins, Jr, MD, MPH; Terry Dwyer, MD, MPH; George Macones, MD; Philip A. May, PhD; Jeff Murray, MD; Richard M. Pauli, MD, PhD; Raymond W. Redline, MD; and Michael Varner, MD. The PASS Research Network is supported by the National Institute on Alcohol Abuse and Alcoholism, Eunice Kennedy Shriver National Institute of Child Health and Human Development, and National Institute on Deafness and Other Communication Disorders through the Cooperative Agreement Mechanism (U01HD055154, U01 HD045935, U01 HD055155, U01HD045991, and U01 AA016501). The following institutions and researchers comprise the PASS Network (additional network members other than authors listed): DCAC: Co-Director: Lisa M. Sullivan, PhD; Biostatistics: Tara Tripp, MA; Project. Management/Regulatory Affairs: Julie M. Petersen, BA; Rebecca A. Young, MPH; Data. Management/Information Technology: Travis Baker, BS; Derek Petersen, BS; Gregory Toland MS. DBPC: Director: Hannah C. Kinney, MD, Assistant Director: Robin L. Haynes, PhD; Co- investigators: David S. Paterson, PhD; Kevin G. Broadbelt, PhD; Kyriacos Markianos, PhD, Ingrid A.Holm; MD, Theonia Boyd, MD; Drucilla Roberts, MD; Richard G. Goldstein, MD; Hanno Stein, PhD; Technicians: Claire Maggiotto, BS; Catherine Hassett, BS. CCS NP: Co-investigators: Donald Habbe, MD; H. Eugene Hoyme, MD; William Massello III, MD; Bradley Randall, MD; Mary Ann Sens, MD, PhD; Catherine Stoos, MD, Peter Van Eerden, MD; Project Management: Whitney Adler, BA; Elizabeth Berg, RN; Jessica Gromer, RN; Bethany Norton, MA; Liz Swenson, RN; Deb Tobacco, MA. CCS SA: Project Management: Erna Carstens, RN, Mandy Potter, RN, Lucy Brink, MSc, Sylvia Abrahams, RN; Allison Borchardt, RN; Noorjahan Bosman, RN; Ciska Botha, BSocSc; Lehana Breytenbach, RN; Lucy Brink, M.Sc.; Lucille Burger, RN; Carina Carstens, BCur (Nursing); Erna Carstens, RN; Weslin Charles, Hons BA (Psychol.); Milly de Jager, RN; Carlie du Plessis, RN; Sandra Felix, RN; Nicola James (Nel), MCur (Nursing); Ronnie Jurgens, RN; Belda Klukowski, RN; Mugeleigh Lakay, MCur (Nursing); Samacia Maloy, RN; Marilyn Mentor, RN; Petra Opperman, RN; Berenice Pillay, RN; Mandy Potter, RN; Earl Prinsloo, BA Hons (Sociology); Sonja Schell, RN; Marisa van der Spuy, BCur (Nursing); Mariëtta Warwick, RN. PAC: Project Management: Carmen Condon, BA; Daianna Rodriguez, BA; Albany Perez, BA; Data Processing: Margaret C. Shair, BA; Tracy Thai, BA. NIH: Project Scientists: Marian Willinger, PhD (NICHD); Dale Herald, PhD (NIAAA); Howard J. Hoffman, PhD (NIDCD); Chuan-Ming Li, MD, PhD (NIDCD); Program Officers: Bill Dunty, PhD (NIAAA); Tonse Raju, MD, DCH (NICHD); Gordon B. Hughes, MD (NIDCD). Further, the following individuals made significant contributions to the research and warrant recognition: DCAC: Idania Ramirez, MPH; Jamie Collins, MA; Laura Spurchise, MPH; DBPC: Richard A. Belliveau, BA; Kristin McMillan, BA; Megan Minter, MS; PAC: Johnston T. Grier, BA; Emilia F. Vignola, BA; Joseph J. Violaris, BA. The opinions expressed in this paper are those of the authors and do not necessarily reflect the views of the Indian Health Service (IHS) or the National Institutes of Health, the National Institute of Mental Health, the Eunice Kennedy Shriver National Institute of Child Health and Development (NICHD), the National Institute on Alcohol Abuse and Alcoholism (NIAAA), or the National Institute on Deafness and Other Communication Disorders (NIDCD).
Funding
This research was supported by grants T32MH016434-40 issued by the National Institute of Mental Health, U01HD055154, U01HD045935, U01HD055155, U01HD045991 and U01AA016501 issued by the National Institute on Alcohol Abuse and Alcoholism, Eunice Kennedy Shriver National Institute of Child Health and Human Development, and the National Institute on Deafness and Other Communication Disorders.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Shuffrey, L.C., Myers, M.M., Odendaal, H.J. et al. Fetal heart rate, heart rate variability, and heart rate/movement coupling in the Safe Passage Study. J Perinatol 39, 608–618 (2019). https://doi.org/10.1038/s41372-019-0342-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41372-019-0342-9
This article is cited by
-
Exploring the Influence of Fetal Sex on Heart Rate Dynamics Using Fetal Magnetocardiographic Recordings
Reproductive Sciences (2024)
-
Characterisation of neonatal cardiac dynamics using ordinal partition network
Medical & Biological Engineering & Computing (2022)
-
Biomechanics of Human Fetal Hearts with Critical Aortic Stenosis
Annals of Biomedical Engineering (2021)