Abstract
Objectives
To describe health-care spending and utilization for infants discharged from the neonatal intensive care unit (NICU).
Study design
Retrospective cohort analysis of 4973 NICU graduates in the Truven MarketScan Medicaid database, with follow-up to the third birthday. Health-care spending and utilization after NICU discharge were assessed. Using logistic regression, we assessed clinical characteristics associated with hospitalization and emergency department (ED) visits.
Results
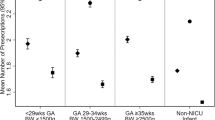
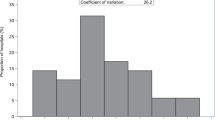
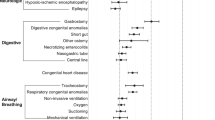
Most (69.5%) post-NICU spending occurred within the first year [$33,276 per member per year]. Inpatient care accounted for most (71.6%) of the 3-year spending. The percentages of infants with a 1-year readmission or ED visit were 36.8% and 63.7%, respectively. Medical technology was associated with the highest likelihoods of hospital [aOR 17.8 (95%CI 12.2–26.0)] and ED use [aOR 2.3 (95%CI 1.8–3.0)].
Conclusions
Hospital care accounts for the majority of spending for NICU graduates. Infants with medical technology have the highest risk of hospital and ED use.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Harrison W, Goodman D. Epidemiologic trends in neonatal intensive care, 2007-12. JAMA Pediatr. 2015;169:855–62.
Jarjour IT. Neurodevelopmental outcome after extreme prematurity: a review of the literature. Pediatr Neurol. 2015;52:143–52.
Serenius F, Kallen K, Blennow M, Ewald U, Fellman V, Holmstrom G, et al. Neurodevelopmental outcome in extremely preterm infants at 2.5 years after active perinatal care in Sweden. JAMA. 2013;309:1810–20.
McCormick MC, Litt JS, Smith VC, Zupancic JA. Prematurity: an overview and public health implications. Annu Rev Public Health. 2011;32:367–79.
Msall ME, Tremont MR. Measuring functional outcomes after prematurity: developmental impact of very low birth weight and extremely low birth weight status on childhood disability. Ment Retard Dev Disabil Res Rev. 2002;8:258–72.
Hack M, Taylor HG, Drotar D, Schluchter M, Cartar L, Andreias L, et al. Chronic conditions, functional limitations, and special health care needs of school-aged children born with extremely low-birth-weight in the 1990s. JAMA. 2005;294:318–25.
Behrman RE, Butler AS, editors. Preterm birth: causes, consequences, and prevention. Washington (DC): The National Academies Collection: Reports funded by National Institutes of Health; 2007.
Petrou S, Davidson LL. Economic issues in the follow-up of neonates. Semin Neonatol. 2000;5:159–69.
Johnston KM, Gooch K, Korol E, Vo P, Eyawo O, Bradt P, et al. The economic burden of prematurity in Canada. BMC Pediatr. 2014;14:93.
Lamarche-Vadel A, Blondel B, Truffer P, Burguet A, Cambonie G, Selton D, et al. Re-hospitalization in infants younger than 29 weeks’ gestation in the EPIPAGE cohort. Acta Paediatr. 2004;93:1340–5.
Russell RB, Green NS, Steiner CA, Meikle S, Howse JL, Poschman K, et al. Cost of hospitalization for preterm and low birth weight infants in the United States. Pediatrics. 2007;120:e1–9.
Lorch SA, Passarella M, Zeigler A. Challenges to measuring variation in readmission rates of neonatal intensive care patients. Acad Pediatr. 2014;14(5 Suppl):S47–53.
Wade KC, Lorch SA, Bakewell-Sachs S, Medoff-Cooper B, Silber JH, Escobar GJ. Pediatric care for preterm infants after NICU discharge: high number of office visits and prescription medications. J Perinatol. 2008;28:696–701.
Edwards ST, Abrams MK, Baron RJ, Berenson RA, Rich EC, Rosenthal GE, et al. Structuring payment to medical homes after the Affordable Care Act. J Gen Intern Med. 2014;29:1410–3.
Bockli K, Andrews B, Pellerite M, Meadow W. Trends and challenges in United States neonatal intensive care units follow-up clinics. J Perinatol. 2014;34:71–4.
Agency for Healthcare Research and Quality. Chronic Condition Indicator [Available from: http://www.hcup-us.ahrq.gov/toolssoftware/chronic/chronic.jsp.] Accessed December 31, 2017.
Chi MJ, Lee CY, Wu SC. The prevalence of chronic conditions and medical expenditures of the elderly by chronic condition indicator (CCI). Arch Gerontol Geriatr. 2011;52:284–9.
Friedman B, Jiang HJ, Elixhauser A, Segal A. Hospital inpatient costs for adults with multiple chronic conditions. Med Care Res Rev. 2006;63:327–46.
Feudtner C, Hays RM, Haynes G, Geyer JR, Neff JM, Koepsell TD. Deaths attributed to pediatric complex chronic conditions: national trends and implications for supportive care services. Pediatrics. 2001;107:E99.
Feudtner C, Feinstein JA, Zhong W, Hall M, Dai D. Pediatric complex chronic conditions classification system version 2: updated for ICD-10 and complex medical technology dependence and transplantation. BMC Pediatr. 2014;14:199.
Cohen E, Berry JG, Camacho X, Anderson G, Wodchis W, Guttmann A. Patterns and costs of health care use of children with medical complexity. Pediatrics. 2012;130:e1463–70.
Palfrey JS, Haynie M, Porter S, Fenton T, Cooperman-Vincent P, Shaw D, et al. Prevalence of medical technology assistance among children in Massachusetts in 1987 and 1990. Public Health Rep. 1994;109:226–33.
Berry JG, Hall DE, Kuo DZ, Cohen E, Agrawal R, Feudtner C, et al. Hospital utilization and characteristics of patients experiencing recurrent readmissions within children’s hospitals. JAMA. 2011;305:682–90.
Agrawal R, Hall M, Cohen E, Goodman DM, Kuo DZ, Neff JM, et al. Trends in health care spending for children in Medicaid with high resource use. Pediatrics. 2016;138. pii: e20160682. Epub 2016 Sep 15.
Kuo DZ, Hall M, Agrawal R, Cohen E, Feudtner C, Goodman DM, et al. Comparison of health care spending and utilization among children with Medicaid insurance. Pediatrics. 2015;136:1521–9.
McAllister JW, Cooley WC, Van Cleave J, Boudreau AA, Kuhlthau K. Medical home transformation in pediatric primary care--what drives change? Ann Fam Med. 2013;11(Suppl 1):S90–8.
Clemans-Cope L, Holahan J, Garfield R. Medicaid spending growth compared to other payers: a look at the evidence. Menlo Park, CA: The Henry J. Kaiser Family Foundation; 2016.
Acknowledgements
DZK and CJS were supported by the Health Resources and Services Administration (HRSA) of the U.S. Department of Health and Human Services (HHS) under grant number R40MC23626. This information or content and conclusions are those of the author and should not be construed as the official position or policy of, nor should any endorsements be inferred by HRSA, HHS, or the U.S. Government.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Kuo, D.Z., Berry, J.G., Hall, M. et al. Health-care spending and utilization for children discharged from a neonatal intensive care unit. J Perinatol 38, 734–741 (2018). https://doi.org/10.1038/s41372-018-0055-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41372-018-0055-5
This article is cited by
-
Risk factors for hospital readmission among infants with prolonged neonatal intensive care stays
Journal of Perinatology (2022)
-
Medicaid and moms: the potential impact of extending medicaid coverage to mothers for 1 year after delivery
Journal of Perinatology (2022)
-
The financial burden experienced by families of preterm infants after NICU discharge
Journal of Perinatology (2022)
-
Healthcare Utilization for Medicaid-Insured Children with Medical Complexity: Differences by Sociodemographic Characteristics
Maternal and Child Health Journal (2022)
-
Association of gastrostomy placement on hospital readmission in premature infants
Journal of Perinatology (2019)