Abstract
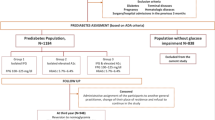
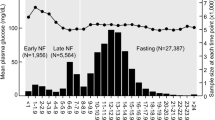
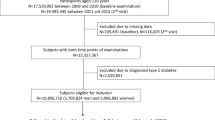
The impact of 3-year change in glycemic state on the risk of hypertension among Tehranian adults aged ≥20 years was assessed. The study population included 1679 men and 2348 women who were non-diabetic normotensive at enrollment. The following categories were defined both at baseline visit and three years later (second visit): normoglycemia [normal fasting glucose (NFG) and normal glucose tolerance (NGT)] and prediabetes [impaired fasting glucose (IFG) or impaired glucose tolerance (IGT)]. Changes in the categories, i.e., regression to normoglycemia, remaining in previous status, and progression to diabetes were assessed. Changes in fasting plasma glucose (FPG) and 2-hour plasma glucose (2hPG) categories were also considered separately. We used the Cox models adjusted for traditional hypertension risk factors to estimate hazard ratios (HRs) with 95% confidence intervals (CIs). During a median follow-up of 9.4 years, 485 men and 589 women developed hypertension. Among men, considering both FPG and 2hPG, compared to individuals remaining normoglycemic, changing from prediabetes to normoglycemia had a HR of 1.30 (95% CI: 0.98–1.71; P-value: 0.064). Defining changes by 2hPG showed that compared to remaining NGT, incident IGT (progression from NGT to IGT) had a significant association with increased risk of hypertension development by a HR of 1.61 (1.13–2.30). Among women, on the other hand, change in glycemic state generally didn’t show a significant association with incident hypertension. To sum up, change in glycemic state hadn’t a significant association with hypertension development among women; however, compared to remaining NGT, men with incident IGT had a significant higher risk.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 digital issues and online access to articles
$119.00 per year
only $9.92 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Organization WH. Global status report on noncommunicable diseases 2014. World Health Organization; 2014.
Ogurtsova K, da Rocha Fernandes J, Huang Y, Linnenkamp U, Guariguata L, Cho NH, et al. IDF Diabetes Atlas: Global estimates for the prevalence of diabetes for 2015 and 2040. Diabetes Res Clin Pract. 2017;128:40–50.
Schlesinger S, Neuenschwander M, Barbaresko J, Lang A, Maalmi H, Rathmann W, et al. Prediabetes and risk of mortality, diabetes-related complications and comorbidities: umbrella review of meta-analyses of prospective studies. Diabetologia. 2021:1–11.
Parizadeh D, Rahimian N, Akbarpour S, Azizi F, Hadaegh F. Sex-specific clinical outcomes of impaired glucose status: a long follow-up from the Tehran Lipid and Glucose Study. Eur J Preventive Cardiol. 2019;26:1080–91.
Association AD. 2. Classification and diagnosis of diabetes: standards of medical care in diabetes—2020. Diabetes Care. 2020;43:S14–31.
Nandhini LP, Kamalanathan S, Sahoo J. Definition, diagnostic criteria, screening, diagnosis, and classification of diabetes and categories of glucose intolerance. In: The Diabetes Textbook. Springer, 2019, pp 71–85.
Esteghamati A, Etemad K, Koohpayehzadeh J, Abbasi M, Meysamie A, Noshad S, et al. Trends in the prevalence of diabetes and impaired fasting glucose in association with obesity in Iran: 2005–2011. Diabetes Res Clin Pr. 2014;103:319–27.
Moazzeni SS, Ghafelehbashi H, Hasheminia M, Parizadeh D, Ghanbarian A, Azizi F, et al. Sex-specific prevalence of coronary heart disease among Tehranian adult population across different glycemic status: Tehran lipid and glucose study, 2008–2011. BMC Public Health. 2020;20:1510.
Organization WH. A global brief on hypertension: silent killer, global public health crisis: World Health Day 2013. World Health Organization, 2013.
Mohammadian Khonsari N, Shahrestanaki E, Ejtahed HS, Djalalinia S, Sheidaei A, Hakak-Zargar B, et al. Long-term trends in hypertension prevalence, awareness, treatment, and control rate in the Middle East and North Africa: a systematic review and meta-analysis of 178 population-based studies. Curr Hypertens Rep. 2021;23:41.
Asgari S, Moazzeni SS, Azizi F, Abdi H, Khalili D, Hakemi MS, et al. Sex-specific incidence rates and risk factors for hypertension during 13 years of follow-up: the tehran lipid and glucose study. Glob Heart. 2020;15:29–29.
Ferrannini E, Cushman WC. Diabetes and hypertension: the bad companions. Lancet. 2012;380:601–10.
De Boer IH, Bangalore S, Benetos A, Davis AM, Michos ED, Muntner P, et al. Diabetes and hypertension: a position statement by the American Diabetes Association. Diabetes Care. 2017;40:1273–84.
Bjørnholt JV, Erikssen G, Kjeldsen SE, Bodegård J, Thaulow E, Erikssen J. Fasting blood glucose is independently associated with resting and exercise blood pressures and development of elevated blood pressure. J Hypertension. 2003;21:1383–9.
Cheung BM, Wat NM, Tso AW, Tam S, Thomas GN, Leung GM, et al. Association between raised blood pressure and dysglycemia in Hong Kong Chinese. Diabetes Care. 2008;31:1889–91.
Geva M, Shlomai G, Berkovich A, Maor E, Leibowitz A, Tenenbaum A, et al. The association between fasting plasma glucose and glycated hemoglobin in the prediabetes range and future development of hypertension. Cardiovasc Diabetol. 2019;18:53.
Kuwabara M, Chintaluru Y, Kanbay M, Niwa K, Hisatome I, Andres-Hernando A, et al. Fasting blood glucose is predictive of hypertension in a general Japanese population. J Hypertension. 2019;37:167–74.
Jung JY, Oh C-M, Choi J-M, Ryoo J-H, Park SK. Long-term risk of hypertension in normoglycemia and prediabetes, and their relation to the change of glycemic state. Am J Hypertension. 2018;31:1042–8.
Britton KA, Pradhan AD, Gaziano JM, Manson JE, Ridker PM, Buring JE, et al. Hemoglobin A1c, body mass index, and the risk of hypertension in women. Am J Hypertension. 2011;24:328–34.
Mohan V, Anjana RM, Unnikrishnan R, Venkatesan U, Sankari GU, Rahulashankiruthiyayan T, et al. Incidence of hypertension among Asian Indians: 10 year follow up of the Chennai Urban Rural Epidemiology Study (CURES-153). J Diabetes Complications. 2020;34:107652.
Kabootari M, Hasheminia M, Azizi F, Mirbolouk M, Hadaegh F. Change in glucose intolerance status and risk of incident cardiovascular disease: Tehran Lipid and Glucose Study. Cardiovascular Diabetol. 2020;19:1–11.
Lee G, Kim SM, Choi S, Kim K, Jeong S-M, Son JS, et al. The effect of change in fasting glucose on the risk of myocardial infarction, stroke, and all-cause mortality: a nationwide cohort study. Cardiovascular Diabetol. 2018;17:1–10.
Azizi F, Ghanbarian A, Momenan AA, Hadaegh F, Mirmiran P, Hedayati M, et al. Prevention of non-communicable disease in a population in nutrition transition: Tehran Lipid and Glucose Study phase II. Trials. 2009;10:1–15.
Momenan AA, Delshad M, Sarbazi N, Rezaei Ghaleh N, Ghanbarian A, Azizi F. Reliability and validity of the Modifiable Activity Questionnaire (MAQ) in an Iranian urban adult population. Arch Iran Med. 2012;15:279–82.
Diagnosis ECot. Mellitus* CoD. Follow-up report on the diagnosis of diabetes mellitus. Diabetes Care. 2003;26:3160–7.
Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL Jr., et al. The seventh report of the joint national committee on prevention, detection, evaluation, and treatment of high blood pressure: the JNC 7 report. JAMA. 2003;289:2560–71.
Cordero A, Alegria-Ezquerra E. TG/HDL ratio as surrogate marker for insulin resistance. EJ Cardiol Pr [Internet]. 2009;8:16.
Derakhshan A, Tohidi M, Hajebrahimi M, Saadat N, Azizi F, Hadaegh F. Sex‐specific incidence rates and risk factors of insulin resistance and β–cell dysfunction: a decade follow‐up in a Middle Eastern population. Diabet Med. 2017;34:245–52.
Perreault L. Prediabetes. In: Feingold KR, Anawalt B, Boyce A, Chrousos G, de Herder WW, Dhatariya K, et al. (eds). Endotext. South Dartmouth (MA): MDText.com, Inc. Copyright © 2000-2022; 2000.
Tramunt B, Smati S, Grandgeorge N, Lenfant F, Arnal JF, Montagner A, et al. Sex differences in metabolic regulation and diabetes susceptibility. Diabetologia. 2020;63:453–61.
Goossens GH, Jocken JW, Blaak EE. Sexual dimorphism in cardiometabolic health: the role of adipose tissue, muscle and liver. Nat Rev Endocrinol. 2021;17:47–66.
Sullivan GM, Feinn R. Using effect size-or why the P value is not enough. J Grad Med Educ. 2012;4:279–82.
Acknowledgements
The authors would like to express their appreciation to the TLGS participants and staff for their kind cooperation.
Author information
Authors and Affiliations
Contributions
Study conception and design: SSM and FH. Analysis and interpretation of data: MH and FH. Drafting of the manuscript: SSM, SD and FH. Critical revision: RHA, FA and FH. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval
The ethics committee of the Research Institute for Endocrine Sciences of the Shahid Beheshti University of Medical Sciences approved the study proposal (IR.SBMU.ENDOCRINE.REC.1400.138).
Informed consent
Written informed consent was also obtained from all participants.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Moazzeni, S.S., Dehghani, S., Hasheminia, M. et al. Three-year change in glycemic state and the future risk of incident hypertension among Iranian adults: Tehran Lipid and Glucose Study. J Hum Hypertens 37, 944–949 (2023). https://doi.org/10.1038/s41371-022-00788-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41371-022-00788-5