Abstract
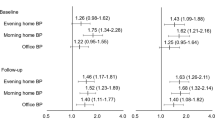
Ambulatory blood pressure (BP) is associated with mortality, but it is also interesting to expand its association with cardiovascular morbidity. This study sought to evaluate association with cardiovascular morbidity and cardiovascular mortality. Patients without cardiovascular disease who had a first 24-hour ambulatory BP monitoring were followed-up until the onset of the first event (a combined variable of cardiovascular mortality, coronary heart disease, cerebrovascular disease, peripheral arteriopathy, or hospital admission for heart failure). Changes in antihypertensive treatment couldn’t be collected. Cox regression analysis was adjusted for risk factors and office BP. We included 3907 patients (mean age, 58.0, SD 13.8 years), of whom 85.5% were hypertensive. The follow up period was 6.6 (95% CI 5.0–8.5) years. A total of 496 (12.7%) events were recorded. The incidence rate was 19.3 (95% CI 17.7–21.1) cases per 1000 person-years. The patients with an event compared to the rest of patients were mostly men, older, with higher office and ambulatory systolic BP, higher prevalence of diabetes, chronic kidney disease, dyslipidemia, and non-dipper or riser circadian profile. In the fully adjusted model, office BP loses its significant association with the main variable. Ambulatory BP association remained significant with cardiovascular morbidity and mortality, HR 1.494 (1.326–1.685) and 0.767 (0.654–0.899) for 24-hour systolic and diastolic BP, respectively. Nighttime systolic BP also maintained this significant association, 1.270 (1.016–1.587). We conclude that nighttime systolic BP and 24-hour BP are significantly associated with cardiovascular events and cardiovascular mortality in patients without cardiovascular disease attended under conditions of routine clinical practice.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 digital issues and online access to articles
$119.00 per year
only $9.92 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
Data availability
The data are not publicly available because of ethical restrictions related to protecting patient confidentiality.
References
Banegas JR, Graciani A, de la Cruz JJ, Leon-Muñoz LM, Guallar-Castillon P, Coca A, et al. Achievement of cardiometabolic goals in aware hypertensive patients in Spain: a nationwide population-based study. Hypertension. 2012;60:898–905.
Whelton PK, Carey RM, Aronow WS, Casey DE Jr, Collins KJ, Dennison Himmelfarb C, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/apha/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension. 2018;71:e13–e115.
Williams B, Mancia G, Spiering W, Agabiti Rosei E, Azizi M, Burnier M, et al. 2018 ESC/ESH guidelines for the management of arterial hypertension: the Task Force for the management of arterial hypertension of the European Society of Cardiology and the European Society of Hypertension: the Task Force for the management of arterial hypertension of the European Society of Cardiology and the European Society of Hypertension. J Hypertens. 2018;36:1953–2041.
Thomopoulos C, Parati G, Zanchetti A. Effects of blood pressure lowering on outcome incidence in hypertension. 1. Overview, meta-analyses, and metaregression analyses of randomized trials. J Hypertens. 2014;32:2285–95.
Kikuya M, Ohkubo T, Asayama K, Metoki H, Obara T, Saito S, et al. Ambulatory blood pressure and 10-year risk of cardiovascular and noncardiovascular mortality: the Ohasama study. Hypertension. 2005;45:240–5.
Sega R, Facchetti R, Bombelli M, Cesana G, Corrao G, Grassi G, et al. Prognostic value of ambulatory and home blood pressures compared with office blood pressure in the general population: follow-up results from the PAMELA study. Circulation. 2005;111:1777–83.
Dolan E, Stanton A, Thijs L, Hinedi K, Atkins N, McClory S, et al. Superiority of ambulatory over clinic blood pressure measurement in predicting mortality: the Dublin outcome study. Hypertension. 2005;46:156–61.
Verdecchia P, Porcellati C, Schillaci G, Borgioni C, Ciucci A, Battistelli M, et al. ABP, An independent predictor of prognosis in essential hypertension. Hypertension. 1994;24:793–801.
Staessen JA, Thijs L, Fagard R, O’Brien ET, Clement D, de Leeuw PW, et al. Predicting cardiovascular risk using conventional vs ambulatory blood pressure in older patients with systolic hypertension. Syst-Eur Investigators. JAMA. 1999;282:539–46.
Clement DL, De Buyzere ML, De Bacquer DA, de Leeuw PW, Duprez DA, Fagard RH, et al. Office versus Ambulatory Pressure Study Investigators. Prognostic Value of Ambulatory Blood-Pressure Recordings in Patients with Treated Hypertension. N. Engl J Med. 2003;348:2407–15.
de la Sierra A, Banegas JR, Segura J, Gorostidi M, Ruilope LM, CARDIORISC Event Investigators. ABPM and development of cardiovascular events in high-risk patients included in the Spanish ABPM registry: the CARDIORISC Event study. J Hypertens. 2012;30:713–9.
Hansen TW, Kikuya M, Thijs L, Björklund-Bodegård K, Kuznetsova T, Ohkubo T, et al. Prognostic superiority of daytime ambulatory over conventional blood pressure in four populations: a meta-analysis of 7,030 individuals. J Hypertens. 2007;25:1554–64.
Franklin SS, Thijs L, Hansen TW, Li Y, Boggia J, Kiyuya M, et al. International Database on ABP in Relation to Cardiovascular Outcomes Investigators. Significance of white-coat hypertension in older persons with isolated systolic hypertension: a meta-analysis using the International Database on ABPM in Relation to Cardiovascular Outcomes population. Hypertension. 2012;59:564–71.
Investigators ABC-H, Roush GC, Fagard RH, Salles GF, Pierdomenico SD, Reboldi G, et al. Prognostic impact from clinic, daytime, and night-time systolic blood pressure in nine cohorts of 13,844 patients with hypertension. J Hypertens. 2014;32:2332–40.
Yang WY, Melgarejo JD, Thijs L, Zhang ZY, Boggia J, Wei FF, et al. Association of office and ambulatory blood pressure with mortality and cardiovascular outcomes. JAMA 2019;322:409–20.
Wing LMH, Chowdhury EK, Reid CM, Beilin LJ, Brown MA. ANBP2 Management Committee. Night-time ambulatory blood pressure is the best pretreatment blood pressure predictor of 11-year mortality in treated older hypertensives. Blood Press Monit. 2018;23:237–43.
Li Y, Thijs L, Zhang ZY, Asayama K, Hansen TW, Boggia J, et al. International Database on Ambulatory and Home Blood Pressure in Relation to Cardiovascular Outcome Investigators. Opposing Age-Related Trends in Absolute and Relative Risk of Adverse Health Outcomes Associated With Out-of-Office Blood Pressure. Hypertension 2019;74:1333–42.
Rahman M, Wang X, Bundy JD, Charleston J, Cohen D, Cohen J, et al. CRIC Study Investigators. prognostic significance of ambulatory bp monitoring in ckd: a report from the chronic renal insufficiency cohort (CRIC) study. J Am Soc Nephrol. 2020;31:2609–21.
Kario K, Hoshide S, Mizuno H, Kabutoya T, Nishizawa M, Yoshida T, et al. Nighttime blood pressure phenotype and cardiovascular prognosis: practitioner-based nationwide JAMP study. Circulation. 2020;142:1810–20.
Gorostidi M, Sobrino J, Segura J, Sierra C, de la Sierra A, Hernández del Rey R, et al. Ambulatory blood pressure monitoring in hypertensive patients with high cardiovascular risk: a cross-sectional analysis of a 20 000-patient database in Spain. J Hypertens. 2007;25:977–84.
Banegas JR, Segura J, Sobrino J, Rodríguez-Artalejo F, de la Sierra A, de la Cruz JJ, et al. Effectiveness of blood pressure control outside the medical setting. Hypertension. 2007;49:62–68.
Vinyoles E, Felip A, Pujol E, de la Sierra A, Dura R, del Rey RH, et al. Clinical characteristics of isolated clinic hypertension. J Hypertens. 2008;26:438–45.
Vinyoles E, Rodriguez-Blanco T, de la Sierra A, Felip A, Banegas JR, de la Cruz JJ, et al. Isolated clinic hypertension: diagnostic criteria based on 24-h blood pressure definition. J Hypertens. 2010;28:2407–13.
O’Brien E, Mee F, Atkins N, O’Malley K. Accuracy of the SpaceLabs 90207 determined by the British Hypertension Society Protocol. J Hypertens. 1991;9:S25–S31.
Ragazzo F, Saladini F, Palatini P. Validation of the Microlife WatchBP 03 device for clinic, home and ambulatory blood pressure measurement, according to the International Protocol. Blood Press Monit. 2010;15:59–62.
Gijón-Conde T, Gorostidi M, Banegas JR, de la Sierra A, Segura J, Vinyoles E, et al. Position statement on ambulatory blood pressure monitoring (ABPM) by the Spanish Society of Hypertension (2019). Hipertens Riesgo Vasc. 2019;36:199–212.
American Diabetes Association. 2. Classification and diagnosis of diabetes: standards of medical care in diabetes-2018. Diabetes Care. 2018;41:S13–S27.
Maiques-Galán A, Villar-Álvarez F, Brotons-Cuixart C, Torcal-Laguna J, Orozco-Beltrán D, Navarro-Paerez J, et al. Grupo de Prevención Cardiovascular del PAPPS. [Preventive cardiovascular recommendations]. Aten Primaria. 2007;39:15–26.
Ramos R, Balló E, Marrugat J, Elosua R, Sala J, Grau M, et al. Validity for use in research on vascular diseases of the SIDIAP (Information System for the Development of Research in Primary Care): the EMMA study. Rev Esp Cardiol (Engl Ed). 2012;65:29–37.
CatSalut. CMBD. Generalitat de Catalunya. https://catsalut.gencat.cat/ca/proveidors-professionals/registres-catalegs/registres/cmbd/normativa-manual/#bloc1 (Website consulted on 3 August 2021).
Gu-Mei G, Thijs L, Li Y, Asayama K, Boggia J, Hansen TW, et al. Outcome-driven thresholds for ambulatory pulse pressure in 9938 participants recruited from 11 populations. Hypertension. 2014;63:229–37.
Boggia J, Li Y, Thijs L, Hansen TW, Kikuya M, Björklund-Bodegård K, et al. International Database on Ambulatory blood pressure monitoring in relation to Cardiovascular Outcomes (IDACO) Investigators. Prognostic accuracy of day versus night ambulatory blood pressure: a cohort study. Lancet. 2007;370:1219–29.
Ohkubo T, Kikuya M, Metoki H, Asayama K, Obara T, Hashimoto J, et al. Prognosis of “masked” hypertension and “white-coat” hypertension detected by 24-h ambulatory blood pressure monitoring 10-year follow-up from the Ohasama study. J Am Coll Cardiol. 2005;46:508–15.
Fagard RH, Cornelissen VA. Incidence of cardiovascular events in white coat, masked and sustained hypertension versus true normotension: a meta-analysis. J Hypertens. 2007;25:2193–8.
Pierdomenico SD, Cuccurullo F. Prognostic value of white-coat and masked hypertension diagnosed by ambulatory monitoring in initially untreated subjects: an updated meta-analysis. Am J Hypertens. 2011;24:52–58.
Stenestrand U, Wijkman M, Fredrikson M, Nystrom FH. Association between admission supine systolic blood pressure and 1-year mortality in patients admitted to the intensive care unit for acute chest pain. JAMA. 2010;303:1167–72.
Martín-Rioboó E, Pérula de Torres LA, Banegas JR, Lobos-Bejarano JM, Brotons Cuixart C, García, et al. Knowledge, availability, and use of ambulatory and home blood pressure monitoring in primary care in Spain: The MAMPA study. J Hypertens. 2018;36:1051–8.
Acknowledgements
We thank all the investigators of the Spanish Ambulatory Blood Pressure Registry. A list with their names is available at www.cardiorisc.com/archivos/investigadores_CARDIORISC_SEH-LELHA.pdf
Funding
Supported by the Spanish Society of Hypertension and by an unrestricted grant from Lacer Laboratories, Spain. Specific funding for this analysis was obtained from a grant (PERIS SLT002/16/00061) from the Ministry of Health, Catalan Government (Generalitat de Catalunya).
Author information
Authors and Affiliations
Contributions
EV, CP, NS, MG, AS, LMR, JAD, MAM, JS were responsible for designing the protocol, writing the protocol, conducting the search, screening potentially eligible studies, interpreting results and writing the manuscript. AR was responsible for extracting and analyzing data, interpreting results, and creating’Summary of findings’ tables.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
This study was specifically approved by the IDIAP Jordi Gol Research Ethics Committee (resolution P17 / 078). All included patients signed the informed consent.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Vinyoles, E., Puig, C., Roso-Llorach, A. et al. Role of ambulatory blood pressure on prediction of cardiovascular disease. A cohort study. J Hum Hypertens 37, 279–285 (2023). https://doi.org/10.1038/s41371-022-00679-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41371-022-00679-9
This article is cited by
-
Echocardiographic Phenotypes of Subclinical Organ Damage: Clinical and Prognostic Value in the General Population. Findings from the Pamela Study
High Blood Pressure & Cardiovascular Prevention (2023)