Abstract
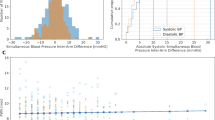
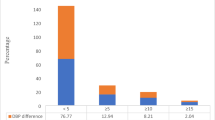
We investigated inter-arm systolic blood pressure (sIAD) difference, reproducibility, and incident cardiovascular disease (CVD). We hypothesized that higher sIAD values have low prevalence and nonpersistence over years, but that CVD risk is higher starting from the time of first high absolute sIAD. In Multi-Ethnic Study of Atherosclerosis participants (n = 6725, 53% female, 45–84 years old), Doppler systolic blood pressure (SBP) measurements were made in both arms (10-minute interval) thrice over 9.5 years. Proportional hazards for CVD (coronary heart disease, heart failure, stroke, peripheral arterial disease (PAD)) over 16.4 years were tested according to time-varying absolute inter-arm difference with covariates: (1) age, gender, race, and clinic; (2) model 1 plus height, heart rate, BP, antihypertensives, BMI, smoking status, lipids, lipid lowering medication, and diabetes. High sIAD was not persistent across exams. Maximum absolute sIAD ≥ 15 mmHg was found at least once in 815 persons. Maximum absolute sIAD had a graded relationship with incident stroke or PAD: 6.2% events; model 2 hazard ratio per 10 mmHg 1.34 (95% CI, 1.15–1.56) and this risk was approximately doubled for maximum absolute sIAD ≥ 15 mmHg vs 0–4 mmHg. Total CVD risk (18.4% events) was increased only for maximum absolute sIAD ≥25 mmHg. Associations with incident CVD did not differ for higher SBP in left vs right arm. A higher maximum absolute sIAD at any exam was associated with greater risk for stroke and PAD especially for values ≥ 15 mmHg, and ≥25 mmHg for other CVD. Measuring SBP between arms may help identify individuals at risk for CVD.

This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 digital issues and online access to articles
$119.00 per year
only $9.92 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
Data availability
Data are available on reasonable request to the MESA Coordinating Center (https://www.mesa-nhlbi.org/).
References
Weinberg I, Gona P, O’Donnell CJ, Jaff MR, Murabito JM. The systolic blood pressure difference between arms and cardiovascular disease in the Framingham Heart Study. Am J Med. 2014;127:209–15.
Arnett DK, Tang W, Province MA, Oberman A, Ellison RC, Morgan D, et al. Interarm differences in seated systolic and diastolic blood pressure: the Hypertension Genetic Epidemiology Network study. J Hypertens. 2005;23:1141–47.
Clark CE, Taylor RS, Shore AC, Campbell JL. Prevalence of systolic inter-arm differences in blood pressure for different primary care populations: systematic review and meta-analysis. Br J Gen Pr. 2016;66:e838–47.
Harrison EG Jr, Roth GM, Hines EA Jr. Bilateral indirect and direct arterial pressures. Circulation. 1960;22:419–36.
Kim JY, Kim EJ, Namgung J, Cho BR, Nam CW, Kim YK, et al. Between-visit reproducibility of inter-arm systolic blood pressure differences in treated hypertensive patients: the coconet study. Hypertens Res. 2017;40:483–86.
Grossman A, Weiss A, Beloosesky Y, Morag-Koren N, Green H, Grossman E. Inter-arm blood pressure difference in hospitalized elderly patients-is it consistent? J Clin Hypertens. 2014;16:518–23.
Eguchi K, Yacoub M, Jhalani J, Gerin W, Schwartz JE, Pickering TG. Consistency of blood pressure differences between the left and right arms. Arch Intern Med. 2007;167:388–93.
Kleefstra N, Houweling ST, Meyboom-de Jong B, Bilo HJ. Measuring the blood pressure in both arms is of little use; longitudinal study into blood pressure differences between both arms and its reproducibility in patients with diabetes mellitus type 2.Ned Tijdschr Geneeskd. 2007;151:1509–14. (in Dutch, English abstract)
Huibers A, Hendrikse J, Brown MM, Pegge SA, Arnold M, Moll FL, et al. Upper extremity blood pressure difference in patients undergoing carotid revascularisation. Eur J Vasc Endovasc Surg. 2017;53:153–57.
Clark CE, Taylor RS, Shore AC, Ukoumunne OC, Campbell JL. Association of a difference in systolic blood pressure between arms with vascular disease and mortality: a systematic review and meta-analysis. Lancet. 2012;379:905–14.
Clark CE, Campbell JL, Powell RJ, Thompson JF. The inter-arm blood pressure difference and peripheral vascular disease: cross-sectional study. Fam Pr. 2007;24:420–26.
Clark CE, Steele AM, Taylor RS, Shore AC, Ukoumunne OC, Campbell JL. Interarm blood pressure difference in people with diabetes: measurement and vascular and mortality implications: a cohort study. Diabetes Care. 2014;37:1613–20.
Kranenburg G, Spiering W, de Jong PA, Kappelle LJ, de Borst GJ, Cramer MJ, et al. Inter-arm systolic blood pressure differences, relations with future vascular events and mortality in patients with and without manifest vascular disease. Int J Cardiol. 2017;244:271–76.
Tomiyama H, Ohkuma T, Ninomiya T, Mastumoto C, Kario K, Hoshide S. et al. Simultaneously measured interarm blood pressure difference and stroke: an individual participants data meta-analysis. Hypertension. 2018;71:1030–38.
Clark CE, Warren FC, Boddy K, McDonagh STJ, Moore SF, Goddard J. et al. Associations between systolic interarm differences in blood pressure and cardiovascular disease outcomes and mortality: individual participant data meta-analysis, development and validation of a prognostic algorithm: the INTERPRESS-IPD (Inter-arm Blood Pressure Difference- individual Participant Data) Collaboration. Hypertension. 2021;77:650–61.
Shadman R, Criqui MH, Bundens WP, Fronek A, Denenberg JO, Gamst AC, et al. Subclavian artery stenosis: prevalence, risk factors, and association with cardiovascular diseases. J Am Coll Cardiol. 2004;44:618–23.
Aboyans V, Criqui MH, McDermott MM, Allison MA, Denenberg JO, Shadman R, et al. The vital prognosis of subclavian stenosis. J Am Coll Cardiol. 2007;49:1540–45.
Aboyans V, Kamineni A, Allison MA, McDermott MM, Crouse JR, Ni H. et al. The epidemiology of subclavian stenosis and its association with markers of subclinical atherosclerosis: the Multi-Ethnic Study of Atherosclerosis (MESA). Atherosclerosis. 2010;211:266–70.
Bild DE, Bluemke DA, Burke GL, Detrano R, Diez Roux AV, Folsom AR, et al. Multi-Ethnic Study of Atherosclerosis: objectives and design. Am J Epidemiol. 2002;156:871–81.
Duprez DA, Jacobs DR Jr, Lutsey PL, Bluemke DA, Brumback LC, Polak JF, et al. Association of small artery elasticity with incident cardiovascular disease in older adults: the multi-ethnic study of atherosclerosis. Am J Epidemiol. 2011;174:528–36.
Grassi G, Bombelli M, Brambilla G, Trevano FQ, Dell’oro R, Mancia G. Total cardiovascular risk, blood pressure variability and adrenergic overdrive in hypertension: evidence, mechanisms and clinical implications. Curr Hypertens Rep. 2012;14:333–8.
Rothwell PM. Limitations of the usual blood-pressure hypothesis and importance of variability, instability, and episodic hypertension. Lancet. 2010;375:938–48.
Rothwell PM, Howard SC, Dolan E, O’Brien E, Dobson JE, Dahlöf B, et al. Prognostic significance of visit-to-visit variability, maximum systolic blood pressure, and episodic hypertension. Lancet. 2010;375:895–905.
Stevens SL, Wood S, Koshiaris C, Law K, Glasziou P, Stevens RJ, et al. Blood pressure variability and cardiovascular disease: systematic review and meta- analysis. BMJ. 2016;354:i4098.
Yeh CH, Yu HC, Huang TY, Huang PF, Wang YC, Chen TP et al. High systolic and diastolic blood pressure variability is correlated with the occurrence of peripheral arterial disease in the first decade following a diagnosis of Type 2 Diabetes mellitus: a new biomarker from old measurement. Biomed Res Int. 2016; 2016:9872945.
Yano Y, Reis JP, Lewis CE, Sidney S, Pletcher MJ, Bibbins-Domingo K, et al. Association of blood pressure patterns in young adulthood with cardiovascular disease and mortality in middle age. JAMA Cardiol. 2020;5:382–9.
Nwabuo CC, Yano Y, Moreira HT, Appiah D, Vasconcellos HD, Aghaji QN, et al. Between visit-to-visit blood pressure variability in early adulthood and myocardial structure and function in later life. JAMA Cardiol. 2020;5:795–801.
Nwabuo CC, Yano Y, Moreira HT, Appiah D, Vasconcellos HD, Aghaji QN. Long-term blood pressure variability in young adulthood and coronary artery calcium and carotid intima-media thickness in midlife: the CARDIA study. Hypertension. 2020;76:404–9.
Tedla YG, Yano Y, Carnethon M, Greenland P. Association between long-term blood pressure variability and 10-year progression in arterial stiffness: the multiethnic study of atherosclerosis. Hypertension. 2017;69:118–27.
Muntner P, Levitan EB, Reynolds K, Mann DM, Tonelli M, Oparil S, et al. Within-visit variability of blood pressure and all-cause and cardiovascular mortality among US adults. J Clin Hypertens. 2012;14:165–71.
Funding
This research project was supported by R01 HL142283-01A1. The Multi-ethnic Study of Atherosclerosis was supported by contracts N01-HC-95159, N01-HC-95160, N01-HC- 95161, N01-HC-95162, N01-HC-95163, N01-HC-95164, N01-HC-95165, N01-HC-95166, N01-HC-95167, N01-HC-95168, and N01-HC-95169 from the National Heart, Lung and Blood Institute(NHLBI) and by grants UL1-TR-000040 and UL1-TR-001079 from the National Center for Research Resources.
Author information
Authors and Affiliations
Contributions
Conception and design, DAD, DRJ, MHC, MAA. Analysis and interpretation DRJ, DAD, LCB, LIBA. Drafting the manuscript: DAD, DRJ. Review for important intellectual content: DAD, DRJ, LIBA, LCB, JOD, RLM, ICT, MHC, MAA.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Duprez, D.A., Jacobs, D.R., Andrews, L.I.B. et al. Inter-arm systolic blood pressure difference: non-persistence and association with incident cardiovascular disease in the Multi-ethnic Study of Atherosclerosis. J Hum Hypertens 37, 197–204 (2023). https://doi.org/10.1038/s41371-022-00669-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41371-022-00669-x
This article is cited by
-
Association between inter-arm blood pressure difference and cardiovascular disease: result from baseline Fasa Adults Cohort Study
Scientific Reports (2023)
-
Blood pressure changes during tenofovir-based antiretroviral therapy among people living with HIV in Lilongwe, Malawi: results from the prospective LighTen Cohort Study
Clinical Research in Cardiology (2023)