Abstract
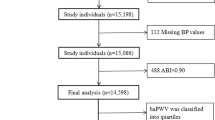
Recent analysis of systolic inter-arm differences in blood pressure from the INTERPRESS-IPD Collaboration suggest an association with increased all-cause mortality, cardiovascular mortality and cardiovascular events. Previous studies have demonstrated associations with other risk parameters. We aimed to reproduce these associations in a cohort of 199 treated, at-risk hypertensive patients with pulse wave velocity (PWV) as a surrogate marker of cardiovascular (CV) damage. Simultaneously measured inter-arm blood pressure (BP) differences, 24 hour ambulatory BP and PWV were measured in 199 treated patients from a tertiary hospital hypertension outpatient clinic. Associations between systolic inter-arm BP difference and PWV were analyzed with uni- and multi-variate regression models. Out of 199 participants, 90 showed an inter-arm BP difference of more than 5 mmHg. The inter-arm difference was not associated with PWV. Furthermore, neither observed single BP measurements nor 24 hour ambulatory BP was associated with inter-arm BP differences. In our clinical patient cohort we failed to observe an association between inter-arm BP differences and PWV. Mode of assessment, study design and the sample characteristics of this treated, hypertensive cohort may have contributed to the negative findings. The limited sample size of the study poses a challenge to the detection of smaller effects in our study.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 digital issues and online access to articles
$119.00 per year
only $9.92 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
Data availability
The data underlying this article cannot be shared publicly due to the privacy of individuals that participated in the study.
References
Canepa M, Milaneschi Y, Ameri P, AlGhatrif M, Leoncini G, Spallarossa P, et al. Relationship between inter-arm difference in systolic blood pressure and arterial stiffness in community-dwelling older adults. J Clin Hypertens. 2013;15:880–7. https://doi.org/10.1111/jch.12178.
Kim KB, Oh MK, Kim HG, Ki JH, Lee SH, Kim SM. Inter-arm differences in simultaneous blood pressure measurements in ambulatory patients without cardiovascular diseases. Korean J Fam Med. 2013;34:98–106. https://doi.org/10.4082/kjfm.2013.34.2.98.
Okada H, Fukui M, Tanaka M, Matsumoto S, Iwase H, Kobayashi K, et al. A difference in systolic blood pressure between arms is a novel predictor of the development and progression of diabetic nephropathy in patients with type 2 diabetes. Atherosclerosis. 2013;230:198–201.
Johansson JK, Puukka PJ, Jula AM. Interarm blood pressure difference and target organ damage in the general population. J Hypertens. 2014;32:260–6. https://doi.org/10.1097/HJH.0000000000000040.
Mehlsen J, Wiinberg N. Interarm difference in blood pressure: reproducibility and association with peripheral vascular disease. Int J Vasc Med. 2014;2014:841542. https://doi.org/10.1155/2014/841542.
Su H-M, Lin T-H, Hsu P-C, Lee W-H, Chu C-Y, Chen S-C, et al. Association of bilateral brachial-ankle pulse wave velocity difference with peripheral vascular disease and left ventricular mass index. Catapano A, editor. PLoS ONE. 2014;9:e88331. https://doi.org/10.1371/journal.pone.0088331.
Tanaka Y, Fukui M, Tanaka M, Fukuda Y, Mitsuhashi K, Okada H, et al. The inter-arm difference in systolic blood pressure is a novel risk marker for subclinical atherosclerosis in patients with type 2 diabetes. Hypertens Res. 2014;37:548–52. www.nature.com/hr.
Durrand JW, Batterham AM, O’Neill BR, Danjoux GR. Prevalence and implications of a difference in systolic blood pressure between one arm and the other in vascular surgical patients. Anaesthesia. 2013;68:1247–52. https://doi.org/10.1111/anae.12452.
Kim J, Song TJ, Song D, Lee HS, Nam CM, Nam HS, et al. Interarm blood pressure difference and mortality in patients with acute ischemic stroke. Neurology. 2013;80:1457–64. https://n.neurology.org/content/80/16/1457.
Sheng CS, Liu M, Zeng WF, Huang QF, Li Y, Wang JG. Four-limb blood pressure as predictors of mortality in elderly chinese. Hypertension. 2013;61:1155–60. https://doi.org/10.1161/HYPERTENSIONAHA.111.00969.
Weinberg I, Gona P, O’Donnell CJ, Jaff MR, Murabito JM. The systolic blood pressure difference between arms and cardiovascular disease in the Framingham Heart Study. Am J Med. 2014;127:209–15.
Clark CE, Steele AM, Taylor RS, Shore AC, Ukoumunne OC, Campbell JL. Interarm blood pressure difference in people with diabetes: measurement and vascular and mortality implications. Diabetes Care. 2014;37:1613–20. https://doi.org/10.2337/dc13-1576/-/DC1.
White J, Mortensen LH, Kivimäki M, Gale CR, Batty GD. Interarm differences in systolic blood pressure and mortality among US army veterans: aetiological associations and risk prediction in the Vietnam experience study. Eur J Prev Cardiol. 2014;21:1394–400. https://doi.org/10.1177/2047487313496193.
Tokitsu T, Yamamoto E, Hirata Y, Fujisue K, Sugamura K, Maeda H, et al. Relationship between inter-arm blood pressure differences and future cardiovascular events in coronary artery disease. J Hypertens. 2015;33:1780–90. http://journals.lww.com/00004872-201509000-00010.
Grossman A, Prokupetz A, Gordon B, Morag-Koren N, Grossman E. Inter-arm blood pressure differences in young, healthy patients. J Clin Hypertens. 2013;15:575–8. https://doi.org/10.1111/jch.12125.
Clark CE, Warren FC, Boddy K, McDonagh STJ, Moore SF, Goddard J. et al. Associations between systolic interarm differences in blood pressure and cardiovascular disease outcomes and mortality. Hypertension. 2020;77:650–61. https://doi.org/10.1161/HYPERTENSIONAHA.120.15997.
Williams B, Mancia G, Spiering W, Rosei EA, Azizi M, Burnier M, et al. 2018 ESC/ESH guidelines for themanagement of arterial hypertension. J Hypertens. 2018;36:1956–2041. https://www.ncbi.nlm.nih.gov/pubmed/30234752.
van der Hoeven NV, Lodestijn S, Nanninga S, van Montfrans GA, van den Born B-JH. Simultaneous compared with sequential blood pressure measurement results in smaller inter-arm blood pressure differences. J Clin Hypertens. 2013;15:839–44. https://doi.org/10.1111/jch.12203.
Verberk WJ, Kessels AGH, Thien T. Blood pressure measurement method and inter-arm differences: a meta-analysis. Am J Hypertens. 2011;24:1201–8. https://doi.org/10.1038/ajh.2011.125.
Nadir MA. Interarm blood pressure diff erence and vascular disease. Lancet. 2012;380:23. http://ees.elsevier.com/.
Verberk WJ, Kroon AA, Thien T, Lenders JW, van Montfrans GA, Smit AJ, et al. Prevalence of the white-coat effect at multiple visits before and during treatment. J Hypertens. 2006;24:2357–63. http://journals.lww.com/00004872-200612000-00008.
Clark CE, Taylor RS, Campbell JL, Shore AC. Prevalence of systolic inter-arm differences in blood pressure for different primary care populations: systematic review and meta-analysis. Br J Gen Pract. 2016;66:e838–47. https://bjgp.org/content/66/652/e838.
Nolde JM, Kiuchi MG, Carnagarin R, Frost S, Kannenkeril D, Lugo‐Gavidia LM, et al. Supine blood pressure—a clinically relevant determinant of vascular target organ damage in hypertensive patients. J Clin Hypertens. 2020. https://onlinelibrary.wiley.com/doi/10.1111/jch.14114.
Nolde JM, Kiuchi MG, Lugo-Gavidia LM, Ho JK, Chan J, Matthews VB, et al. Nocturnal hypertension: a commonphenotype in a tertiary clinical setting associatedwith increased arterial stiffness and central blood pressure. J Hypertens. 2021;39:250–258
Nolde JM, Lugo-Gavidia LM, Kannenkeril D, Chan J, Matthews VB, Carnagarin R, et al. Increased pulse wave velocity in patients with an orthostatic blood pressure rise independent of other cardiovascular risk factors. J Hypertens. 2021;Publish Ah:1–9.
Frost S, Nolde JM, Chan J, Joyson A, Gregory C, Carnagarin R, et al. Retinal capillary rarefaction is associated with arterial and kidney damage in hypertension. Sci Rep. 2021;1–10. https://doi.org/10.1038/s41598-020-79594-3.
Vlachopoulos C, Terentes-Printzios D, Laurent S, Nilsson PM, Protogerou AD, Aznaouridis K, et al. Association of estimated pulse wave velocity with survival: a secondary analysis of SPRINT. JAMA Netw Open. 2019;2:e1912831. https://jamanetwork.com/.
Butlin M, Qasem A. Large artery stiffness assessment using SphygmoCor technology. Pulse. 2016;4:180–92. https://www.karger.com/Article/FullText/452448.
Mancia G, Fagard R, Narkiewicz K, Redon J, Zanchetti A, Bohm M, et al. 2013 ESH/ESC guidelines for the management of arterial hypertension: the Task Force for the Management of Arterial Hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). Eur Hear J. 2013;34:2159–219. https://www.ncbi.nlm.nih.gov/pubmed/23771844.
Unger T, Borghi C, Charchar F, Khan NA, Poulter NR, Prabhakaran D, et al. 2020 International Society of Hypertension global hypertension practice guidelines. J Hypertens. 2020;38:982–1004. http://journals.lww.com/10.1097/HJH.0000000000002453.
Kario K, Shin J, Chen CH, Buranakitjaroen P, Chia YC, Divinagracia R, et al. Expert panel consensus recommendations for ambulatory blood pressure monitoring in Asia: the HOPE Asia Network. J Clin Hypertens. 2019;21:1250–83.
O’Brien E, Parati G, Stergiou G. Ambulatory blood pressure measurement what is the international consensus? Hypertension. 2013;62:988–94.
Seabold S, Perktold J. Statsmodels: econometric and statistical modeling with Python. PROC. OF THE 9th PYTHON IN SCIENCE CONF. 2010. http://statsmodels.sourceforge.net/.
Clark CE, Taylor RS, Butcher I, Stewart MC, Price J, Fowkes FGR, et al. Inter-arm blood pressure difference and mortality: a cohort study in an asymptomatic primary care population at elevated cardiovascular risk. Br J Gen Pract. 2016;66:e297–308. https://bjgp.org/content/66/646/e297.
Clark CE, Taylor RS, Shore AC, Campbell JL. The difference in blood pressure readings between arms and survival: Primary care cohort study. BMJ. 2012;344. http://www.bmj.com/.
Eguchi K, Yacoub M, Jhalani J, Gerin W, Schwartz JE, Pickering TG. Consistency of blood pressure differences between the left and right arms. Arch Intern Med. 2007;167:388–93. www.archinternmed.com.
Martin U, Holder R, Hodgkinson J, McManus R. Inter-arm blood pressure differences compared with ambulatory monitoring: a manifestation of the “white-coat” effect? Br J Gen Pract. 2013;63. https://pubmed.ncbi.nlm.nih.gov/23561681/.
Su H-M, Lin T-H, Hsu P-C, Chu C-Y, Lee W-H, Chen S-C, et al. Association of interarm systolic blood pressure difference with atherosclerosis and left ventricular hypertrophy. Lavie CJ, editor. PLoS ONE. 2012;7:e41173. https://doi.org/10.1371/journal.pone.0041173.
Ma W, Zhang B, Yang Y, Qi L, Meng L, Zhang Y, et al. Correlating the relationship between interarm systolic blood pressure and cardiovascular disease risk factors. J Clin Hypertens. 2017;19:466–71. https://pubmed.ncbi.nlm.nih.gov/28295936/.
Milan A, Zocaro G, Leone D, Tosello F, Buraioli I, Schiavone D, et al. Current assessment of pulse wave velocity. J Hypertens. 2019;37:1547–57. https://journals.lww.com/00004872-201908000-00003.
Acknowledgements
The authors acknowledge Mrs. Derrin Brockman and the Royal Perth Hospital Research Foundation for their administrative and technical support. This work was supported by resources provided by the Pawsey Supercomputing Center with funding from the Australian Government and the Government of Western Australia.
Author information
Authors and Affiliations
Contributions
JMN: Conceptualization, data collection, data curation, formal analysis, visualization, writing—original draft, writing—review and editing. LMLG: Data collection, data curation, writing—review and editing. DK: Data collection, writing—review and editing. JC: Data collection, writing—review and editing. SR: Data collection, writing—review and editing. AJOSE: Data collection, writing—review and editing. AJOYSON: Data collection, writing—review and editing. LS: Data collection, writing—review and editing. RC: Data collection, writing—review and editing. OA: Data collection, writing—review and editing. MGK: Data collection, writing—review and editing. MPS: Supervision, conceptualization, data collection, formal analysis, visualization, writing—review and editing.
Corresponding author
Ethics declarations
Competing interests
JMN and the other authors declare that they have no competing interests. LMLG has received a scholarship from the National Council on Science and Technology, Mexico (CONACYT). RC is supported by the Australian National Heart Foundation post doc fellowship. MPS is supported by an NHMRC Research Fellowship and has received consulting fees, and/or travel and research support from Medtronic, Abbott, Novartis, Servier, Pfizer, and Boehringer-Ingelheim.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Nolde, J.M., Lugo-Gavidia, L.M., Kannenkeril, D. et al. Simultaneously measured inter-arm blood pressure difference is not associated with pulse wave velocity in a clinical dataset of at-risk hypertensive patients. J Hum Hypertens 36, 811–818 (2022). https://doi.org/10.1038/s41371-021-00588-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41371-021-00588-3
This article is cited by
-
Inter-arm blood pressure difference, when is it a useful risk marker for cardiovascular events?
Journal of Human Hypertension (2022)