Abstract
This randomized crossover trial sought to determine whether wearing a high-efficiency particulate-filtering respirator (PFR) improves cardiovascular function over 48 h among healthy college students in Tehran. This trial was conducted from February 14th to 23rd, 2019 and twenty-six participants completed two 48-h intervention periods. Brachial blood pressure (BP) measured by 24-h ambulatory monitoring was the primary health outcome. Secondary outcomes included 48-h heart rate variability (HRV) indices, high-sensitive cardiac troponin (hs-TnT) and other biomarkers. The participants wore the PFR between 10.2 and 11.1 h while awake during the interventions. More than 80% of participants reported increased respiratory resistance while wearing the PFR due to a lack of an exhalation valve. There were no significant differences in brachial BP levels between subjects who wore PFR respirator and those did not. Except for high frequency (HF) power and heart rate (HR), no significant differences between interventions were observed for other HRV metrics. Wearing the PFR led to an increase of 66.0 ms2 (95% confidence interval [CI], 9.6–110.5) and 79.6 ms2 (95% CI, 19.0–140.1) in HF power during the first day when the two groups of participants wore the PFR. Night-time HR was significantly increased during the PFR intervention period. Other secondary outcomes were not significantly different between interventions. It is plausible that incomplete exposure reduction due to wearing the PFR less than half of the time or increased respiratory resistance mitigated potential health benefits. Additional trials are warranted to validate the CV protection of wearing PFRs in heavily-polluted cities.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 digital issues and online access to articles
$119.00 per year
only $9.92 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout






Similar content being viewed by others
References
Hadley MB, Baumgartner J, Vedanthan R. Developing a clinical approach to air pollution and cardiovascular health. Circulation. 2018;137:725–42.
Lelieveld J, Klingmüller K, Pozzer A, Pöschl U, Fnais M, Daiber A et al. Cardiovascular disease burden from ambient air pollution in Europe reassessed using novel hazard ratio functions. Eur Heart J. 2019;40:1590–6.
Basu R, Malig B, Broadwin R, Ebisu K, Gold EB, Qi L, et al. Association between gaseous air pollutants and inflammatory, hemostatic and lipid markers in a cohort of midlife women. Environ Int. 2017;107:131–9.
Hadley MB, Vedanthan R, Fuster V. Air pollution and cardiovascular disease: a window of opportunity. Nat Rev Cardiol. 2018;15:193–4.
Frumkin H, Haines A. Global environmental change and noncommunicable disease risks. Ann Rev Public Health. 2019;40:261–82.
Mensah GA, Roth GA, Fuster V. The global burden of cardiovascular diseases and risk factors: 2020 and beyond. J Am Coll Cardiol. 2019;74:2529–32.
Brook RD, Newby DE, Rajagopalan S. The global threat of outdoor ambient air pollution to cardiovascular health: time for intervention. JAMA Cardiol. 2017;2:353–4.
Schraufnagel DE, Balmes J, Cowl CT, De Matteis S, Jung S-H, Mortimer K et al. Air pollution and non-communicable diseases: a review by the forum of international respiratory societies’ environmental committee. Part 2: air pollution and organ systems. Chest. 2018;155:417–26.
Morishita M, Wang L, Speth K, Zhou N, Bard RL, Li F, et al. Acute blood pressure and cardiovascular effects of near-roadway exposures with and without N95 respirators. Am J Hypertens. 2019;32:1054–65.
Barzeghar V, Sarbakhsh P, Hassanvand MS, Faridi S, Gholampour A. Long-term trend of ambient air PM10, PM2. 5, and O3 and their health effects in Tabriz city, Iran, during 2006–2017. Sustain Cities Soc. 2020;54:101988.
Rajagopalan S, Al-Kindi SG, Brook RD. Air pollution and cardiovascular disease: JACC state-of-the-art review. J Am Coll Cardiol. 2018;72:2054–70.
Giles LV, Barn P, Künzli N, Romieu I, Mittleman MA, van Eeden S, et al. From good intentions to proven interventions: effectiveness of actions to reduce the health impacts of air pollution. Environ Health Perspect. 2010;119:29–36.
Langrish JP, Li X, Wang S, Lee MM, Barnes GD, Miller MR, et al. Reducing personal exposure to particulate air pollution improves cardiovascular health in patients with coronary heart disease. Environ Health Perspect. 2012;120:367–72.
Barrett JR. Air pollution intervention: study links use of face masks to improved cardiovascular outcomes. Nat Inst Environ Health Sci. 2012;120:A122.
Shi J, Lin Z, Chen R, Wang C, Yang C, Cai J, et al. Cardiovascular benefits of wearing particulate-filtering respirators: a randomized crossover trial. Environ Health Perspect. 2016;125:175–80.
Langrish JP, Mills NL, Chan JK, Leseman DL, Aitken RJ, Fokkens PH, et al. Beneficial cardiovascular effects of reducing exposure to particulate air pollution with a simple facemask. Part Fibre Toxicol. 2009;6:8.
Guan T, Hu S, Han Y, Wang R, Zhu Q, Hu Y, et al. The effects of facemasks on airway inflammation and endothelial dysfunction in healthy young adults: a double-blind, randomized, controlled crossover study. Part fibre Toxicol. 2018;15:30.
Cherrie JW, Apsley A, Cowie H, Steinle S, Mueller W, Lin C, et al. Effectiveness of face masks used to protect Beijing residents against particulate air pollution. Occup Environ Med. 2018;75:446–52.
van Dorn A. Clearing the air: do facemasks protect health? Lancet Respiratory Med. 2017;5:555–6.
Huang W, Morawska L. Face masks could raise pollution risks. Nature Publishing Group. Nature. 2019.
Faridi S, Niazi S, Shamsipour M, Hassanvand MS. Comments on:” Meteorological correlates and AirQ+ health risk assessment of ambient fine particulate matter in Tehran, Iran”. Environ Res. 2019;174:122.
Faridi S, Niazi S, Yousefian F, Azimi F, Pasalari H, Momeniha F et al. Spatial homogeneity and heterogeneity of ambient air pollutants in Tehran. Sci Total Environ. 2019;697:134123.
Yousefian F, Mahvi AH, Yunesian M, Hassanvand MS, Kashani H, Amini H. Long-term exposure to ambient air pollution and autism spectrum disorder in children: a case-control study in Tehran, Iran. Sci total Environ. 2018;643:1216–22.
Faridi S, Naddafi K, Kashani H, Nabizadeh R, Alimohammadi M, Momeniha F, et al. Bioaerosol exposure and circulating biomarkers in a panel of elderly subjects and healthy young adults. Sci Total Environ. 2017;593:380–9.
Faridi S, Shamsipour M, Krzyzanowski M, Künzli N, Amini H, Azimi F, et al. Long-term trends and health impact of PM2. 5 and O3 in Tehran, Iran, 2006–2015. Environ Int. 2018;114:37–49.
Yousefian F, Faridi S, Azimi F, Aghaei M, Shamsipour M, Yaghmaeian K, et al. Temporal variations of ambient air pollutants and meteorological influences on their concentrations in Tehran during 2012–2017. Sci Rep. 2020;10:1–11.
Pacitto A, Amato F, Salmatonidis A, Moreno T, Alastuey A, Reche C, et al. Effectiveness of commercial face masks to reduce personal PM exposure. Sci Total Environ. 2019;650:1582–90.
Bard RL, Ijaz MK, Zhang JJ, Li Y, Bai C, Yang Y, et al. Interventions to reduce personal exposures to air pollution: a primer for health care providers. Glob Heart. 2019;14:47.
Shahbazi H, Reyhanian M, Hosseini V, Afshin H. The relative contributions of mobile sources to air pollutant emissions in Tehran, Iran: an emission inventory approach. Emiss Control Sci Technol. 2016;2:44–56.
Shahbazi H, Hassani A, Hosseini V. Evaluation of Tehran clean air action plan using emission inventory approach. Urban Clim. 2019;27:446–56.
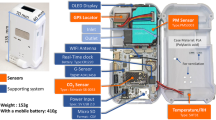
Faridi S, Nodehi RN, Sadeghian S, Tajdini M, Hoseini M, Yunesian M et al. Can respirator face masks in a developing country reduce exposure to ambient particulate matter? J Exposure Sci Environ Epidemiol. 2020;30:1–12.
Morishita M, Adar SD, D’Souza J, Ziemba RA, Bard RL, Spino C, et al. Effect of portable air filtration systems on personal exposure to fine particulate matter and blood pressure among residents in a low-income senior facility: a randomized clinical trial. JAMA Intern Med. 2018;178:1350–7.
Shenal BV, Radonovich LJ Jr, Cheng J, Hodgson M, Bender BS. Discomfort and exertion associated with prolonged wear of respiratory protection in a health care setting. J Occup Environ Hyg. 2012;9:59–64.
Yang B-Y, Qian Z, Howard SW, Vaughn MG, Fan S-J, Liu K-K, et al. Global association between ambient air pollution and blood pressure: a systematic review and meta-analysis. Environ Pollut. 2018;235:576–88.
Yang X, Jia X, Dong W, Wu S, Miller M, Hu D, et al. Cardiovascular benefits of reducing personal exposure to traffic‐related noise and particulate air pollution: a randomized crossover study in the Beijing subway system. Indoor Air. 2018;28:777–86.
Zhang Y, Chu M, Zhang J, Duan J, Hu D, Zhang W, et al. Urine metabolites associated with cardiovascular effects from exposure of size-fractioned particulate matter in a subway environment: a randomized crossover study. Environ Int. 2019;130:104920.
Acknowledgements
We thank the participants, the Exceptional Talents Development Center for Tehran University of Medical Sciences, Institute for Environmental Research (IER) of Tehran University of Medical Sciences and the very supportive staff at Tehran Heart Center.
Funding
This study was financially supported by the Iran National Science Foundation (INSF) (grant number: 97011909). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Faridi, S., Brook, R.D., Hassanvand, M.S. et al. Cardiovascular health effects of wearing a particulate-filtering respirator to reduce particulate matter exposure: a randomized crossover trial. J Hum Hypertens 36, 659–669 (2022). https://doi.org/10.1038/s41371-021-00552-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41371-021-00552-1