Abstract
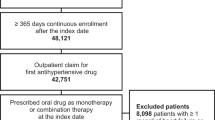
An important component of hypertension management is the initiation and continuation of antihypertensive medications. Non-adherence during the long-term use of antihypertensive medications is well studied. However, there is a paucity of research about the frequency and clinical consequences of failing to take the first dose of an antihypertensive, a treatment challenge known as initial medication non-adherence (IMN). This systematic literature review summarizes the published evidence from 2010 to 2019 on the prevalence, associated factors, consequences, and solutions for IMN to antihypertensive medications in the United States. Of the fifteen studies identified, nine studies reported the prevalence of IMN, two studies examined patient-reported reasons for IMN, and four studies evaluated interventions aimed to lower IMN. It is estimated that 5–34% of patients do not obtain their new antihypertensive medications. Factors and reasons cited include patient demographics, patient beliefs or perceptions about medications, cost or financial barriers, and clinical characteristics, such as a new hypertension diagnosis or higher co-morbid disease burden. The clinical, economic, and patient-reported outcomes of IMN are not well researched. In addition, interventions to address IMN have yielded inconsistent results. Significant opportunities exist for further research into this dimension of patient behavior to better understand and address IMN to new antihypertensive medications.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 digital issues and online access to articles
$119.00 per year
only $9.92 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Nambiar L, LeWinter MM, VanBuren PC, Dauerman HL. Decade-long temporal trends in US hypertension-related cardiovascular mortality. J Am Coll Cardiol. 2020;75:2644–6.
Whelton PK, Carey RM, Aronow WS, Casey DE, Collins KJ, Dennison Himmelfarb C, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension. 2018;71:e13–e115.
Centers for Disease Control and Prevention (CDC). Hypertension cascade: hypertension prevalence, treatment and control estimates among US adults aged 18 years and older applying the criteria from the American College of Cardiology and American Heart Association’s 2017 Hypertension Guideline—NHANES 2013–2016. Atlanta, GA: US Department of Health and Human Services; 2019.
Samanic CM, Barbour KE, Liu Y, Fang J, Lu H, Schiebet L, et al. Prevalence of self-reported hypertension and antihypertensive medication use among adults—United States, 2017. MMWR Morb Mortal Wkly Rep. 2020;69:393–8.
World Health Organization. Adherence to long-term therapies: evidence for action. Geneva, Switzerland: World Health Organization; 2003. https://www.who.int/chp/knowledge/publications/adherence_full_report.pdf?ua=1.
Anderson LJ, Nuckols TK, Coles C, Le MM, Schnipper JL, Shane R, et al. A systematic overview of systematic reviews evaluating medication adherence interventions. Am J Health Syst Pharm. 2020;77:138–47.
Gast A, Mathes T. Medication adherence influencing factors-an (updated) overview of systematic reviews. Syst Rev. 2019;8:112.
Hutchins DS, Zeber JE, Roberts CS, Williams AF, Manias E, Peterson AM, et al. Initial medication adherence-review and recommendations for good practices in outcomes research: an ISPOR medication adherence and persistence special interest group report. Value Health. 2015;18:690–9.
Cooke CE, Xing S, Lee HY, Belletti DA. You wrote the prescription, but will it get filled? J Fam Pr. 2011;60:321–7.
Zeber JE, Manias E, Williams AF, Hutchins D, Udezi WA, Roberts CS, et al. A systematic literature review of psychosocial and behavioral factors associated with initial medication adherence: a report of the ISPOR medication adherence & persistence special interest group. Value Health J Int Soc Pharmacoecon Outcomes Res. 2013;16:891–900.
Adams AJ, Stolpe SF. Defining and measuring primary medication nonadherence: development of a quality measure. J Manag Care Spec Pharm. 2016;22:516–23.
Lee SQ, Raamkumar AS, Li J, Cao Y, Witedwittayanusat K, Chen L, et al. Reasons for primary medication nonadherence: a systematic review and metric analysis. J Manag Care Spec Pharm. 2018;24:778–94.
Cheen MHH, Tan YZ, Oh LF, Wee HL, Thumboo J. Prevalence of and factors associated with primary medication non-adherence in chronic disease: A systematic review and meta-analysis. Int J Clin Pract. 2019;73:e13350.
Comer D, Couto J, Aguiar R, Wu P, Elliott D. Using aggregated pharmacy claims to identify primary nonadherence. Am J Manag Care. 2015;21:e655–e660.
Fischer MA, Stedman MR, Lii J, Vogeli C, Shrank WH, Brookhart MA, et al. Primary medication non-adherence: analysis of 195,930 electronic prescriptions. J Gen Intern Med. 2010;25:284–90.
Fischer MA, Choudhry NK, Brill G, Avorn J, Schneeweiss S, Hutchins D, et al. Trouble getting started: predictors of primary medication nonadherence. Am J Med. 2011;124:1081.e9–1081.e1.081E22.
Jackson TH, Bentley JP, McCaffrey DJ 3rd, Pace P, Holmes E, West-Strum D. Store and prescription characteristics associated with primary medication nonadherence. J Manag Care Spec Pharm. 2014;20:824–32.
Raebel MA, Carroll NM, Ellis JL, Schroeder EB, Bayliss EA. Importance of including early nonadherence in estimations of medication adherence. Ann Pharmacother. 2011;45:1053–60.
Raebel MA, Ellis JL, Carroll NM, Bayliss EA, McGinnis B, Schroeder EB, et al. Characteristics of patients with primary non-adherence to medications for hypertension, diabetes, and lipid disorders. J Gen Intern Med. 2012;27:57–64.
Romanelli RJ, Huang Q, LaMori J, Doshi D, Chung S. Patients' medication-related experience of care is associated with adherence to cardiometabolic disease therapy in real-world clinical practice. Popul Health Manag. 2018;21:409–14.
Shin J, McCombs JS, Sanchez RJ, Udall M, Deminski MC, Cheetham TC. Primary nonadherence to medications in an integrated healthcare setting. Am J Manag Care. 2012;18:426–34.
Shrank WH, Choudhry NK, Fischer MA, Avorn J, Powell M, Schneeweiss S, et al. The epidemiology of prescriptions abandoned at the pharmacy. Ann Intern Med. 2010;153:633–640.
Polinski JM, Kesselheim AS, Frolkis JP, Wescott P, Allen-Coleman C, Fischer MA. A matter of trust: patient barriers to primary medication adherence. Health Educ Res. 2014;29:755–63.
McHorney CA, Spain CV. Frequency of and reasons for medication non-fulfillment and non-persistence among American adults with chronic disease in 2008. Health Expect. 2011;14:307–20.
Fischer MA, Choudhry NK, Bykov K, Brill G, Bopp G, Wurst AM, et al. Pharmacy-based interventions to reduce primary medication nonadherence to cardiovascular medications. Med Care. 2014;52:1050–4.
Fischer MA, Jones JB, Wright E, Van Loan RP, Xie J, Gallagher L, et al. A randomized telephone intervention trial to reduce primary medication nonadherence. J Manag Care Spec Pharm. 2015;21:124–31.
Kerner DE, Knezevich EL. Use of communication tool within electronic medical record to improve primary nonadherence. J Am Pharm Assoc. 2017;57:S270–S273.e2.
O'Connor PJ, Schmittdiel JA, Pathak RD, Harris RI, Newton KM, Ohnsorg KA, et al. Randomized trial of telephone outreach to improve medication adherence and metabolic control in adults with diabetes. Diabetes Care. 2014;37:3317–24.
Hwang W, Chang J, Laclair M, Paz H. Effects of integrated delivery system on cost and quality. Am J Manag Care. 2013;19:e175–84.
Mazzaglia G, Ambrosioni E, Alacqua M, Filippi A, Sessa E, Immordino V, et al. Adherence to antihypertensive medications and cardiovascular morbidity among newly diagnosed hypertensive patients. Circulation. 2009;120:1598–605.
Surescripts. 2019 National progress report. Arlington, Virginia: Surescripts; 2020. https://surescripts.com/news-center/national-progress-report-2019/.
Centers for Disease Control and Prevention (CDC). Behavioral risk factor surveillance system. BRFSS frequently asked questions (FAQs). Atlanta, Georgia: Centers for Disease Control and Prevention; 2020. https://www.cdc.gov/brfss/about/brfss_faq.htm.
Wilhelmsen NC, Eriksson T. Medication adherence interventions and outcomes: an overview of systematic reviews. Eur J Hosp Pharm. 2019;26:187–92.
Gale S, Xing S, Peters S, Cooke CE. Development of a first-fill failure (FFF) service utilizing RXFILL notifications. Pharmacotherapy. 2018;38:e80.
NCPDP. NCPDP SCRIPT Version 2017071 ePrescribing Testing Tool Now Available. Scottsdale, Arizona: NCPDP; 2020. https://www.ncpdp.org/NCPDP/media/pdf/pressrelease/SCRIPT-v-2017071Testing-Tool-Now-Available-091318.pdf.
Centers for Medicare and Medicaid Services. E-prescribing. Baltimore, Maryland: Centers for Medicare and Medicaid Services; 2020 https://www.cms.gov/Medicare/E-Health/Eprescribing.
Moher D, Liberati A, Tetzlaff J, Altman DG, The PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6:e1000097. https://doi.org/10.1371/journal.pmed.1000097.
Acknowledgements
We would like to acknowledge Carly Stokum, MPH, and Eileen Sparling, Ed.M. for their initial reviews and contributions to this manuscript.
Funding
The initial work for this manuscript was supported by an interagency agreement between the Maryland Department of Health and the University of Maryland School of Pharmacy titled “Facilitating Engagement Between Pharmacists and Physician Teams to Improve Outcomes for Patients with Hypertension”.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Cooke, C.E., Xing, S., Gale, S.E. et al. Initial non-adherence to antihypertensive medications in the United States: a systematic literature review. J Hum Hypertens 36, 3–13 (2022). https://doi.org/10.1038/s41371-021-00549-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41371-021-00549-w
This article is cited by
-
Association between health literacy and medication adherence in chronic diseases: a recent systematic review
International Journal of Clinical Pharmacy (2023)
-
Management of Hypertension in the Elderly and Frail Patient
Drugs & Aging (2022)