Abstract
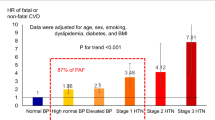
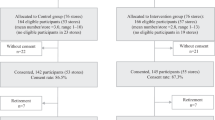
The aim of our study was to evaluate the prevalence, awareness, and control of hypertension in an apparently healthy company population. We conducted a cross-sectional study on a total sample of 2058 individuals with a mean age of 38 ± 9 years, enrolled for the first time to the Ferrari corporate wellness program “Formula Benessere”. Hypertension was defined as systolic blood pressure (SBP) level ≥140 mmHg or diastolic BP (DBP) ≥90 mmHg or use of antihypertensive medication, whereas BP control was defined as BP level <130/80 mmHg. All 2058 participants were divided into three groups based on age: Group 1 aged <40 years (n = 1177, 57%), Group 2 aged 40–50 years (n = 627, 30%), and Group 3 aged >50 years (n = 254, 13%). Four-hundred and one subjects had BP levels ≥130/80 mmHg (19.5%). Two-hundred and sixty-one individuals (12.7%) had high-normal BP values and 140 subjects had rest SBP ≥140 mmHg and/or DBP ≥90 mmHg (6,8%), of which 41 (29.3%) with grade 2 hypertension. In the overall population, 259 individuals (12.5%) were affected by hypertension, the prevalence increasing with age. Only a minority (51%) was aware of being hypertensive and already treated with antihypertensive medications (45.9%). An adequate BP control was achieved in only 57% of subjects who received BP-lowering therapy. Corporate wellness programs may represent an essential tool in identifying apparently healthy subjects with an inadequate control of cardiovascular (CV) risk factors, such as hypertension. These preventive programs in the workplace may help to improve and spread primary CV prevention at the population level.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 digital issues and online access to articles
$119.00 per year
only $9.92 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Lewington S, Clarke R, Qizilbash N, Peto R, Collins R. Prospective Studies Collaboration. Age-specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studies. Lancet. 2002;360:1903–13. https://doi.org/10.1016/s0140-6736(02)11911-8.
Redon J, Mourad JJ, Schmieder RE, Volpe M, Weiss TW. Why in 2016 are patients with hypertension not 100% controlled? A call to action. J Hypertens. 2016;34:1480–1488. https://doi.org/10.1097/HJH.0000000000000988.
Lim SS, Vos T, Flaxman AD, Danaei G, Shibuya K, Adair-Rohani H, et al. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990-2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380:2224–2260. https://doi.org/10.1016/S0140-6736(12)61766-8.
Biffi A, Fernando F, Adami PE, Messina M, Sirico F, Di Paolo F, et al. Ferrari corporate wellness program: results of a pilot analysis and the "Drag" impact in the workplace. High Blood Press Cardiovasc Prev. 2018;25:261–6.
Williams B, Mancia G, Spiering W, Agabiti Rosei E, Azizi M, Burnier M. et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension. Eur Heart J. 2018;39:3021–3104.
Whelton PK, Carey RM, Aronow WS, Casey DE Jr, Collins KJ, Dennison Himmelfarb C, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation 2018;138:e484–e594. https://doi.org/10.1161/CIR.0000000000000596.
NCD Risk Factor Collaboration (NCD-RisC). Worldwide trends in blood pressure from 1975 to 2015: a pooled analysis of 1479 population-based measurement studies with 19·1 million participants. Lancet. 2017;389:37–55.
Tocci G, Muiesan ML, Parati G, Agabiti Rosei E, Ferri C, Virdis A, et al. Trends in prevalence, awareness, treatment, and control of blood pressure recorded from 2004 to 2014 During World Hypertension Day in Italy. J Clin Hypertens (Greenwich). 2016;18:551–6.
Rahimi K, Emdin CA, MacMahon S. The epidemiology of blood pressure and its worldwide management. Circ Res. 2015;116:925–36.
Falaschetti E, Mindell J, Knott C, Poulter N. Hypertension management in England: a serial cross-sectional study from 1994 to 2011. Lancet. 2014;383:1912–9.
Tocci G, Rosei EA, Ambrosioni E, Borghi C, Ferri C, Ferrucci A, et al. Blood pressure control in Italy: analysis of clinical data from 2005-11 surveys on hypertension. J Hypertens. 2012;30:1065–74.
NCD Risk Factor Collaboration (NCD-RisC). Long-term and recent trends in hypertension awareness, treatment, and control in 12 high-income countries: an analysis of 123 nationally representative surveys. Lancet. 2019;394:639–51.
Lee JH, Kim SH, Kang SH, Cho JH, Cho Y, Oh I, et al. Blood pressure control and cardiovascular outcomes: real-world implications of the 2017 ACC/AHA hypertension guideline. Sci Rep. 2018;8:13155. https://doi.org/10.1038/s41598-018-31549-5.
Brunström M, Ng N, Dahlström J, Lindholm LH, Lönnberg G, Norberg M, et al. Association of physician education and feedback on hypertension management with patient blood pressure and hypertension control. JAMA Netw Open. 2020;3:e1918625. https://doi.org/10.1001/jamanetworkopen.2019.18625.
Redon J, Mourad JJ, Schmieder RE, Volpe M, Weiss TW. Why in 2016 are patients with hypertension not 100% controlled? A call to action. J Hypertens. 2016;34:1480–8.
Tocci G, Nati G, Cricelli C, Parretti D, Lapi F, Ferrucci A, et al. Prevalence and control of hypertension in the general practice in Italy: updated analysis of a large database. J Hum Hypertens. 2017;31:258–62.
Volpe M, Gallo G, Tocci G. Is early and fast blood pressure control important in hypertension management? Int J Cardiol. 2018;254:328–32.
Ettehad D, Emdin CA, Kiran A, Anderson SG, Callender T, Emberson J, et al. Blood pressure lowering for prevention of cardiovascular disease and death: a systematic review and meta-analysis. Lancet. 2016;387:957–67. https://doi.org/10.1016/S0140-6736(15)01225-8.
Xie X, Atkins E, Lv J, Bennett A, Neal B, Ninomiya T, et al. Effects of intensive blood pressure lowering on cardiovascular and renal outcomes: updated systematic review and meta-analysis. Lancet. 2016;387:435–43. https://doi.org/10.1016/S0140-6736(15)00805-3.
Hinton TC, Adams ZH, Baker RP, Hope KA, Paton JFR, Hart EC, et al. Investigation and treatment of high blood pressure in young people: too much medicine or appropriate risk reduction? Hypertension. 2020;75:16–22.
Gu A, Yue Y, Argulian E. Age Differences in treatment and control of hypertension in US physician offices, 2003-10: a serial cross-sectional study. Am J Med. 2016;129:50–58.e4. https://doi.org/10.1016/j.amjmed.2015.07.031.
Volpe M, Gallo G, Tocci G. Novel blood pressure targets in patients with high-normal levels and grade 1 hypertension: room for monotherapy? Int J Cardiol. 2019;291:105–111. https://doi.org/10.1016/j.ijcard.2019.04.074.
Torlasco C, Faini A, Makil E, Bilo G, Pengo M, Beaney T, et al. Nation-wide hypertension screening in Italy: data from May Measurements Month 2017-Europe. Eur Heart J Suppl. 2019;21:D66–70. https://doi.org/10.1093/eurheartj/suz058.
Padwal RS, Bienek A, McAlister FA, Campbell NR. Outcomes research task force of the Canadian hypertension education program. Epidemiology of hypertension in Canada: an update. Can J Cardiol. 2016;32:687–94.
Jaffe MG, Lee GA, Young JD, Sidney S, Go AS. Improved blood pressure control associated with a large-scale hypertension program. JAMA. 2013;310:699–705.
Otsuka T, Takada H, Nishiyama Y, Kodani E, Saiki Y, Kato K, et al. Dyslipidemia and the risk of developing hypertension in a working-age male population. J Am Heart Assoc. 2016;5:e003053. https://doi.org/10.1161/JAHA.115.003053.
Borghi C, Veronesi M, Bacchelli S, Esposti DD, Cosentino E, Ambrosioni E. Serum cholesterol levels, blood pressure response to stress and incidence of stable hypertension in young subjects with high normal blood pressure. J Hypertens. 2004;22:265–72.
Creager MA, Cooke JP, Mendelsohn ME, Gallagher SJ, Coleman SM, Loscalzo J, et al. Impaired vasodilation of forearm resistance vessels in hypercholesterolemic humans. J Clin Invest. 1990;86:228–34.
Lloyd-Jones DM, Leip EP, Larson MG, D'Agostino RB, Beiser A, Wilson PW, et al. Prediction of lifetime risk for cardiovascular disease by risk factor burden at 50 years of age. Circulation. 2006;113:791–798. https://doi.org/10.1161/CIRCULATIONAHA.105.548206.
Andersson C, Johnson AD, Benjamin EJ, Levy D, Vasan RS. 70-year legacy of the Framingham heart study. Nat Rev Cardiol. 2019;16:687–98. https://doi.org/10.1038/s41569-019-0202-5.
Mach F, Baigent C, Catapano AL, Koskinas KC, Casula M, Badimon L, et al. 2019 ESC/EAS Guidelines for the management of dyslipidaemias: lipid modification to reduce cardiovascular risk. Eur Heart J. 2020;41:111–188. https://doi.org/10.1093/eurheartj/ehz455.
Landsberg L, Aronne LJ, Beilin LJ, Burke V, Igel LI, Lloyd-Jones D, et al. Obesity-related hypertension: pathogenesis, cardiovascular risk, and treatment: a position paper of The Obesity Society and the American Society of Hypertension. J Clin Hypertens. 2013;15:14–33. https://doi.org/10.1111/jch.12049.
Hall JE, do Carmo JM, da Silva AA, Wang Z, Hall ME. Obesity-induced hypertension: interaction of neurohumoral and renal mechanisms. Circ Res. 2015;116:991–1006. https://doi.org/10.1161/CIRCRESAHA.116.305697.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Biffi, A., Gallo, G., Fernando, F. et al. Usefulness of the corporate wellness projects in primary prevention at the population level: a study on the prevalence, awareness, and control of hypertension in the Ferrari company. J Hum Hypertens 36, 308–314 (2022). https://doi.org/10.1038/s41371-021-00528-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41371-021-00528-1
This article is cited by
-
Association of CYP2C19 Polymorphic Markers with Cardiovascular Disease Risk Factors in Gas Industry Workers Undergoing Periodic Medical Examinations
High Blood Pressure & Cardiovascular Prevention (2023)
-
Blood Pressure Association with the 8-Item Morisky Medication Adherence Scale in Hypertensive Adults from Low-Resource Primary Care Settings: Results from a Prospective Cohort Nested within a Randomised Controlled Trial
High Blood Pressure & Cardiovascular Prevention (2023)
-
Risk Factors Control After an Acute Coronary Syndrome and Association with Major Adverse Cardiovascular Events: A Single Center Experience in Latin-America
High Blood Pressure & Cardiovascular Prevention (2023)
-
World Hypertension Day 2021 in Italy: Results of a Nationwide Survey
High Blood Pressure & Cardiovascular Prevention (2022)