Abstract
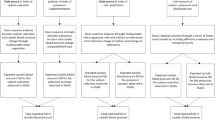
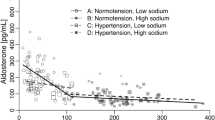
Sodium and potassium appear to interact with each other in their effects on blood pressure with potassium supplementation having a greater blood pressure lowering-effect when sodium intake is high. Whether the effect of sodium reduction on blood pressure varies according to potassium intake levels is unclear. We carried out a systematic review and meta-analysis to examine the impact of baseline potassium intake on blood pressure response to sodium reduction in randomized trials in adult populations, with sodium and potassium intake estimated from 24-h urine samples. We included 68 studies involving 5708 participants and conducted univariable and multivariable meta-regression. The median intake of baseline potassium was 67.7 mmol (Interquartile range: 54.6–76.4 mmol), and the mean reduction in sodium intake was 128 mmol (95% CI: 107–148). Multivariable meta-regression that included baseline 24-h urinary potassium excretion, age, ethnicity, baseline blood pressure, change in 24-h urinary sodium excretion, as well as the interaction between baseline 24-h urinary potassium excretion and change in 24-h urinary sodium excretion did not identify a significant association of baseline potassium intake levels with the blood pressure reduction achieved with a 50 mmol lowering of sodium intake (p > 0.05 for both systolic and diastolic blood pressure). A higher starting level of blood pressure was consistently associated with a greater blood pressure reduction from reduced sodium consumption. However, the nonsignificant findings may subject to the limitations of the data available. Additional studies with more varied potassium intake levels would allow a more confident exclusion of an interaction.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 digital issues and online access to articles
$119.00 per year
only $9.92 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
Code availability
Stata codes for conducting the analyses are available upon reasonable request.
References
G. B. D. Causes of Death Collaborators. Global, regional, and national age-sex-specific mortality for 282 causes of death in 195 countries and territories, 1980-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018;392:1736–88.
Graudal N, Hubeck-Graudal T, Jürgens G, Taylor RS. Dose-response relation between dietary sodium and blood pressure: a meta-regression analysis of 133 randomized controlled trials. Am J Clin Nutr. 2019;109:1273–8.
He F, Li J, Macgregor G. Effect of longer term modest salt reduction on blood pressure: Cochrane systematic review and meta-analysis of randomised trials. BMJ. 2013;346:f1325.
World Health Organization. Tackling NCDs best buys. 2017. https://apps.who.int/iris/bitstream/handle/10665/259232/WHO-NMH-NVI-17.9-eng.pdf;jsessionid=5F68E9D42BD4DD6D485B8D0399DD2D9C?sequence=1. Accessed 2 Jan 2020.
Filippini T, Violi F, D’Amico R, Vinceti M. The effect of potassium supplementation on blood pressure in hypertensive subjects: a systematic review and meta-analysis. Int J Cardiol. 2017;230:127–35.
Aburto N, Hanson S, Gutierrez H, Hooper L, Elliott P, Cappuccio F. Effect of increased potassium intake on cardiovascular risk factors and disease: systematic review and meta-analyses. BMJ. 2013;346:f1378.
Rodrigues SL, Baldo MP, Machado RC, Forechi L, Molina Mdel C, Mill JG. High potassium intake blunts the effect of elevated sodium intake on blood pressure levels. J Am Soc Hypertens. 2014;8:232–8.
Perez V, Chang ET. Sodium-to-potassium ratio and blood pressure, hypertension, and related factors. Adv Nutr. 2014;5:712–41.
World Health Organization. Guideline: potassium intake for adults and children. Geneva: World Health Organization (WHO); 2012.
World Health Organization. Guideline: sodium intake for adults and children. Geneva: World Health Organization (WHO); 2012.
Bernabe-Ortiz A, Sal YRVG, Ponce-Lucero V, Cardenas MK, Carrillo-Larco RM, Diez-Canseco F, et al. Effect of salt substitution on community-wide blood pressure and hypertension incidence. Nat Med. 2020;26:374–8.
Hernandez AV, Emonds EE, Chen BA, Zavala-Loayza AJ, Thota P, Pasupuleti V, et al. Effect of low-sodium salt substitutes on blood pressure, detected hypertension, stroke and mortality. Heart. 2019;105:953–60.
Chang H, Hu Y, Yue C, Wen Y, Yeh W, Hsu L, et al. Effect of potassium-enriched salt on cardiovascular mortality and medical expenses of elderly men. Am J Clin Nutr. 2006;83:1289–96.
Huang L, Trieu K, Yoshimura S, Neal B, Woodward M, Campbell NRC, et al. Effect of dose and duration of reduction in dietary sodium on blood pressure levels: systematic review and meta-analysis of randomised trials. BMJ. 2020;368:m315.
Higgins JP, Green S. Cochrane handbook for systematic reviews of interventions. 2008. https://www.radioterapiaitalia.it/wp-content/uploads/2017/01/cochrane-handbook-for-systematic-reviews-of-interventions.pdf. Accessed 14 May 2019.
Stata. Estimate ratios. https://www.stata.com/manuals13/rratio.pdf. Accessed 2 Jun 2020.
Mark AL, Lawton WJ, Abboud FM, Fitz AE, Connor WE, Heistad DD. Effects of high and low sodium intake on arterial pressure and forearm vascular resistance in borderline hypertension. A preliminary report. Circulation Res. 1975;36:194–8.
Skrabal F, Auböck J, Hörtnagl H. Low sodium/high potassium diet for prevention of hypertension: probable mechanisms of action. Lancet. 1981;2:895–900.
MacGregor G, Markandu N, Best F, Elder D, Cam J, Sagnella G, et al. Double-blind randomised crossover trial of moderate sodium restriction in essential hypertension. Lancet. 1982;1:351–5.
Puska P, Iacono J, Nissinen A, Korhonen H, Vartianinen E, Pietinen P, et al. Controlled, randomised trial of the effect of dietary fat on blood pressure. Lancet. 1983;1:1–5.
Silman AJ, Mitchell P, Locke C, Humpherson P. Evaluation of the effectiveness of a low sodium diet in the treatment of mild to moderate hypertension. Lancet. 1983;1:1179–82.
Watt GCM, Edwards C, Hart JT. Dietary sodium restriction for mild hypertension in general practice. BMJ. 1983;286:432–6.
Gillies A, Carney S, Smith A, Waga S. Adjunctive effect of salt restriction on antihypertensive efficacy. Clin Exp Pharm Physiol. 1984;11:395–8.
Koolen M, Brummelen P. Adrenergic activity and peripheral hemodynamics in relation to sodium sensitivity in patients with essential hypertension. Hypertension. 1984;6:820–5.
Skrabal F, Hamberger L, Cerny E. Salt sensitivity in normotensives with and salt resistance in normotensives without heredity of hypertension. Scand J Clin Lab Invest. 1985;45:47–57.
Grobbee D, Hofman A, Roelandt J, Boomsma F, Schalekamp M, Valkenburg H. Sodium restriction and potassium supplementation in young people with mildly elevated blood pressure. J Hypetens. 1987;5:115–9.
MacGregor GA, Markandu ND, Singer DRJ. Moderate sodium restriction with angiotensin converting enzyme inhibitor in essential hypertension: a double blind study. BMJ. 1987;294:531–4.
Morgan T, Anderson A. Interaction in hypertensive man between sodium intake, converting enzyme inhibitor (enalapril), plasma renin and blood pressure control. J Hum Hypertens. 1988;1:311–5.
Nowson CA, Morgan TO. Change in blood pressure in relation to change in nutrients effected by manipulation of dietary sodium and potassium. Clin Exp Pharm Physiol. 1988;15:225–42.
Staessen J, Bulpitt C, Fagard R, Joossens J, Lijnen P, Amery A. Salt intake and blood pressure in the general population: a controlled intervention trial in two towns. J Hypetens. 1988;6:965–73.
Chalmers JP, Doyle AE, Hopper JL, Howe PRC, Matthews PG, Mathews J, et al. Fall in blood pressure with modest reduction in dietary salt intake in mild hypertension. Lancet. 1989;1:399–402.
Hargreaves M, Morgan T, Snow R, Guerin M. Exercise tolerance in the heat on low and normal salt intakes. Clin Sci. 1989;76:553–7.
MacGregor GA, Markandu ND, Sagnella GA, Singer DRJ, Cappuccio FP. Double-blind study of three sodium intakes and long-term effects of sodium restriction in essential hypertension. Lancet. 1989;2:1244–7.
Bruun N, Skøtt P, Nielsen M, Rasmussen S, Schütten H, Leth A, et al. Normal renal tubular response to changes of sodium intake in hypertensive man. J Hypetens. 1990;8:219–27.
Sharma AM, Arntz HR, Kribben A, Schattenfroh S, Distler A. Dietary sodium restriction: adverse effect on plasma lipids. Klin Wochenschr. 1990;68:664–8.
Carney S, Gillies A, Smith A, Smitham S. Increased dietary sodium chloride in patients treated with antihypertensive drugs. Clin Exp Hypertens A. 1991;13:401–7.
Sharma A, Ruland K, Spies K, Distler A. Salt sensitivity in young normotensive subjects is associated with a hyperinsulinemic response to oral glucose. J Hypetens. 1991;9:329–35.
Alli C, Avanzini F, Bettelli G, Bonati M, Colombo F, Corso R, et al. Feasibility of a long-term low-sodium diet in mild hypertension. J Hum Hypertens. 1992;6:281–6.
Benetos A, Yang-Yan X, Cuche JL, Hannaert P, Safar M. Arterial effects of salt restriction in hypertensive patients. A 9-week, randomized, double-blind, crossover study. J Hypetens. 1992;10:355–60.
Cobiac L, Nestel PJ, LMH Wing, Howe PRC. A low-sodium diet supplemented with fish oil lowers blood pressure in the elderly. J Hypetens. 1992;10:87–92.
Huggins R, Nicolantonio R, Morgan T. Preferred salt levels and salt taste acuity in human subjects after ingestion of untasted salt. Appetite. 1992;18:111–9.
Fotherby MD, Potter JF. Effects of moderate sodium restriction on clinic and twenty-four-hour ambulatory blood pressure in elderly hypertensive subjects. J Hypetens. 1993;11:657–63.
Nestel PJ, Clifton PM, Noakes M, McArthur R, Howe PR. Enhanced blood pressure response to dietary salt in elderly women, especially those with small waist: Hip ratio. J Hypetens. 1993;11:1387–94.
Río A, Rodríguez-Villamil J. Metabolic effects of strict salt restriction in essential hypertensive patients. J Intern Med. 1993;233:409–14.
Sharma A, Schorr U, Oelkers W, Distler A. Effects of sodium salts on plasma renin activity and norepinephrine response to orthostasis in salt-sensitive normotensive subjects. Am J Hypertens. 1993;6:780–5.
Sharma AM, Schorr U, Distler A. Insulin resistance in young salt-sensitive normotensive subjects. Hypertension. 1993;21:273–9.
Howe PRC, Lungershausen YK, Cobiac L, Dandy G, Nestel PJ. Effect of sodium restriction and fish oil supplementation on BP and thrombotic risk factors in patients treated with ACE inhibitors. J Hum Hypertens. 1994;8:43–49.
Iwaoka T, Umeda T, Inoue J, Naomi S, Sasaki M, Fujimoto Y, et al. Dietary NaCl restriction deteriorates oral glucose tolerance in hypertensive patients with impairment of glucose tolerance. Am J Hypertens. 1994;7:460–3.
MacFadyen RJ, Lees KR, Reid JL. Responses to low dose intravenous perindoprilat infusion in salt deplete/salt replete normotensive volunteers. Br J Clin Pharmacol. 1994;38:329–34.
Ferri C, Bellini C, Carlomagno A, Desideri G, Santucci A. Active kallikrein respons to changes in sodium-chloride intake in essential hypertensive patients. J Am Soc Nephrol. 1996;7:443–53.
Inoue J, Cappuccio F, Sagnella G, Markandu N, Folkerd E, Sampson B, et al. Glucose load and renal sodium handling in mild essential hypertension on different sodium intakes. J Hum Hypertens. 1996;10:523–9.
Ishimitsu T, Nishikimi T, Matsuoka H, Kangawa K, Kitamura K, Minami J, et al. Behaviour of adrenomedullin during acute and chronic salt loading in normotensive and hypertensive subjects. Clin Sci. 1996;91:293–8.
Cappuccio FP, Markandu ND, Carney C, Sagnella GA, MacGregor GA. Double-blind randomised trial of modest salt restriction in older people. Lancet. 1997;350:850–4.
Herlitz H, Dahlöf B, Jonsson O, Friberg P. Relationship between salt and blood pressure in hypertensive patients on chronic ACE-inhibition. Blood Press. 1998;7:47–52.
Davrath L, Gotshall R, Tucker A, Sadeh W, Luckasen G, Downes T, et al. Moderate sodium restriction does not alter lower body negative pressure tolerance. Aviat Space Environ Med. 1999;70:577–82.
Boero R, Pignataro A, Bancale E, Campo A, Morelli E, Nigra M, et al. Metabolic effects of changes in dietary sodium intake in patients with essential hypertension. Minerva Urol Nefrol. 2000;52:13–16.
Dishy V, Sofowora G, Imamura H, Nishimi Y, Xie H, Wood A, et al. Nitric oxide production decreases after salt loading but is not related to blood pressure changes or nitric oxide-mediated vascular responses. J Hypetens. 2003;21:153–7.
Nowson CA, Morgan TO, Gibbons C. Decreasing dietary sodium while following a self-selected potassium-rich diet reduces blood pressure. J Nutr. 2003;133:4118–23.
Cappuccio F, Kerry S, Micah F, Plange-Rhule J, Eastwood J. A community programme to reduce salt intake and blood pressure in Ghana [Randomized Controlled Trial; Research Support, Non-U.S. Government]. BMC Public Health. 2006;6:13
Melander O, Wowern F, Frandsen E, Burri P, Willsteen G, Aurell M, et al. Moderate salt restriction effectively lowers blood pressure and degree of salt sensitivity is related to baseline concentration of renin and N-terminal atrial natriuretic peptide in plasma. J Hypetens. 2007;25:619–27.
Tzemos N, Lim P, Wong S, Struthers A, MacDonald T. Adverse cardiovascular effects of acute salt loading in young normotensive individuals. Hypertension. 2008;51:1525–30.
Dickinson K, Keogh J, Clifton P. Effects of a low-salt diet on flow-mediated dilatation in humans. Am J Clin Nutr. 2009;89:485–90.
He F, Marciniak M, Visagie E, Markandu N, Anand V, Dalton R, et al. Effect of modest salt reduction on blood pressure, urinary albumin, and pulse wave velocity in white, black, and Asian mild hypertensives. Hypertension. 2009;54:482–8.
Pimenta E, Gaddam KK, Oparil S, Aban I, Husain S, Dell’Italia LJ, et al. Effects of dietary sodium reduction on blood pressure in subjects with resistant hypertension: Results from a randomized trial. Hypertension 2009;54:475–81.
Starmans-Kool MJ, Stanton AV, Xu YY, Mc GTSA, Parker KH, Hughes AD. High dietary salt intake increases carotid blood pressure and wave reflection in normotensive healthy young men. J Appl Physiol. 2011;110:468–71.
Allen AR, Gullixson LR, Wolhart SC, Kost SL, Schroeder DR, Eisenach JH. Dietary sodium influences the effect of mental stress on heart rate variability: a randomized trial in healthy adults. J Hypetens. 2014;32:374–82.
Gijsbers L, Dower JI, Schalkwijk CG, Kusters YHAM, Bakker SJL, Hollman PCH, et al. Effects of sodium and potassium supplementation on endothelial function: a fully controlled dietary intervention study. Br J Nutr. 2015;114:1419–26.
He FJ, Wu Y, Feng XX, Ma J, Ma Y, Wang H, et al. School based education programme to reduce salt intake in children and their families (School-EduSalt): cluster randomised controlled trial. BMJ. 2015;350:h770.
Matthews EL, Brian MS, Ramick MG, Lennon-Edwards S, Edwards DG, Farquhar WB. High dietary sodium reduces brachial artery flow-mediated dilation in humans with salt-sensitive and salt-resistant blood pressure. J Appl Physiol. 2015:1985;118:1510–5.
Riphagen IJ, Gijsbers L, van Gastel MD, Kema IP, Gansevoort RT, Navis G, et al. Effects of potassium supplementation on markers of osmoregulation and volume regulation: results of a fully controlled dietary intervention study. J Hypetens. 2016;34:215–20.
Suckling RJ, He FJ, Markandu ND, Macgregor GA. Modest salt reduction lowers blood pressure and albumin excretion in impaired glucose tolerance and type 2 diabetes mellitus: a randomized double-blind trial. Hypertension. 2016;67:1189–95.
Brian MS, Dalpiaz A, Matthews EL, Lennon-Edwards S, Edwards DG, Farquhar WB. Dietary sodium and nocturnal blood pressure dipping in normotensive men and women. J Hum Hypertens. 2017;31:145–50.
Rorije NMG, Olde Engberink RHG, Chahid Y, van Vlies N, van Straalen JP, van den Born BH, et al. Microvascular permeability after an acute and chronic salt load in healthy subjects: a randomized open-label crossover intervention study. Anesthesiology. 2018;128:352–60.
Wang Y, Chu C, Wang KK, Hu JW, Yan Y, Lv YB, et al. Effect of salt intake on plasma and urinary uric acid levels in chinese adults: an interventional trial. Sci Rep. 2018;8:1434.
Babcock MC, Robinson AT, Migdal KU, Watso JC, Wenner MM, Stocker SD, et al. Reducing dietary sodium to 1000 mg per day reduces neurovascular transduction without stimulating sympathetic outflow. Hypertension. 2019;73:587–93.
Cashman KD, Kenny S, Kerry JP, Leenhardt F, Arendt EK. ‘Low-salt’ bread as an important component of a pragmatic reduced-salt diet for lowering blood pressure in adults with elevated blood pressure. Nutrients. 2019;11:1725.
Rahimdel T, Morowatisharifabad MA, Salehi-Abargouei A, Mirzaei M, Fallahzadeh H. Evaluation of an education program based on the theory of planned behavior for salt intake in individuals at risk of hypertension. Health Educ Res. 2019;34:268–78.
Ramick MG, Brian MS, Matthews EL, Patik JC, Seals DR, Lennon SL, et al. Apocynin and Tempol ameliorate dietary sodium-induced declines in cutaneous microvascular function in salt-resistant humans. Am J Physiol Heart Circ Physiol. 2019;317:H97–H103.
Rorije NMG, Rademaker E, Schrooten EM, Wouda RD, Homan Van Der Heide JJ, Van Den Born BH, et al. High-salt intake affects sublingual microcirculation and is linked to body weight change in healthy volunteers: a randomized cross-over trial. J Hypertens. 2019;37:1254–61.
Yasutake K, Umeki Y, Horita N, Morita R, Murata Y, Ohe K, et al. A self-monitoring urinary salt excretion level measurement device for educating young women about salt reduction: a parallel randomized trial involving two groups. J Clin Hypertens. 2019;21:730–8.
Baqar S, Kong YW, Chen AX, O’Callaghan C, MacIsaac RJ, Bouterakos M, et al. Effect of salt supplementation on sympathetic activity and endothelial function in salt-sensitive type 2 diabetes. J Clin Endocrinol Metab. 2020;105:e1187–e1200.
Braconnier P, Milani B, Loncle N, Lourenco JM, Brito W, Delacoste J, et al. Short-term changes in dietary sodium intake influence sweat sodium concentration and muscle sodium content in healthy individuals. J Hypertens. 2020;38:159–66.
Migdal KU, Babcock MC, Robinson AT, Watso JC, Wenner MM, Stocker SD, et al. The impact of high dietary sodium consumption on blood pressure variability in healthy, young adults. Am J Hypertens. 2020;33:422–9.
Sacks FM, Svetkey LP, Vollmer WM, Appel LJ, Bray GA, Harsha D.DASH-Sodium Collaborative Research Group et al.Effects on blood pressure of reduced dietary sodium and the Dietary Approaches to Stop Hypertension (DASH) diet.N Engl J Med. 2001;344:3–10.
Skrabal F, Gasser R, Finkenstedt G, Rhomberg H, Lochs A. Low-sodium diet versus low-sodium/high-potassium diet for treatment of hypertension. Klin Wochenschr. 1984;62:124–8.
Smith S, Markandu N, Sagnella G, MacGregor G. Moderate potassium chloride supplementation in essential hypertension: is it additive to moderate sodium restriction? BMJ. 1985;290:110–3.
Powles J, Fahimi S, Micha R, Khatibzadeh S, Shi P, Ezzati M, et al. Global, regional and national sodium intakes in 1990 and 2010: a systematic analysis of 24 h urinary sodium excretion and dietary surveys worldwide. BMJ Open. 2013;3:e003733.
Stone MS, Martyn L, Weaver CM. Potassium intake, bioavailability, hypertension, and glucose control. Nutrients. 2016;8:444.
Barberio AM, Sumar N, Trieu K, Lorenzetti DL, Tarasuk V, Webster J, et al. Population-level interventions in government jurisdictions for dietary sodium reduction: a Cochrane review. Int J Epidemiol. 2017;46:1405–1551.
Marklund M, Singh G, Greer R, Cudhea F, Matsushita K, Micha R, et al. Estimated population wide benefits and risks in China of lowering sodium through potassium enriched salt substitution: modelling study. BMJ. 2020;369:m824.
Greer R, Marklund M, Anderson C, Cobb L, Dalcin A, Henry M, et al. Potassium-enriched salt substitutes as a means to lower blood pressure: benefits and risks. Hypertension. 2020;75:266–74.
Ginos BNR, Engberink R. Estimation of sodium and potassium intake: current limitations and future perspectives. Nutrients. 2020;12:3275.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Outside this work, BN has received salt substitute for trials from Salt Manufacturing Company in China and Nutek. NRCC is an unpaid member of World Action on Salt and Health and an unpaid consultant on dietary sodium and hypertension control to numerous governmental and non-governmental organizations. FJH is a member of Consensus Action on Salt & Health (CASH) and World Action on Salt & Health (WASH). Both CASH and WASH are non-profit charitable organizations and FJH does not receive any financial support from CASH or WASH. JHYW is supported by a UNSW Scientia Fellowship. YH and MM, BN and JHYW, are researchers within a National Health and Medical Research Council Centre for Research Excellence in reducing salt intake using food policy interventions (APP1117300).
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Huang, L., Neal, B., Wu, J.H.Y. et al. The impact of baseline potassium intake on the dose–response relation between sodium reduction and blood pressure change: systematic review and meta-analysis of randomized trials. J Hum Hypertens 35, 946–957 (2021). https://doi.org/10.1038/s41371-021-00510-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41371-021-00510-x