Abstract
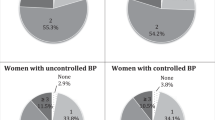
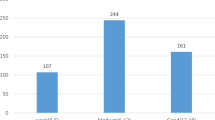
Adoption of a healthy lifestyle is strongly recommended for the control of hypertension, but professional advice alone does not ensure uptake of healthy behavior. Therefore, this study aimed to investigate the factors-associated with non-adoption of healthy behaviors among individuals with a medical diagnosis of hypertension. It was a cross-sectional study using data from the National Health Survey (PNS) carried out in Brazil in 2013, based on interviews with adults (≥18 years) (n = 60,202). The outcome variable was the non-adoption—two or fewer—of healthy behaviors (regular physical activity, recommended consumption of fruit and vegetables, no excessive alcohol consumption, no smoking, and very low/low salt intake [self-perceived]). A logistic regression model was used to verify the factors-associated with non-adoption of healthy behaviors. Approximately 64% of the study sample did not adopt healthy behaviors, i.e., they adopted two or fewer healthy habits. The most frequently mentioned healthy behaviors were not drinking excessively (91.5%), followed by not smoking (86%). Short time since disease diagnosis (OR = 1.20, 95% CI: 1.01–1.43), not using antihypertensive medication (OR = 1.38, 95% CI: 1.13–1.68), not making regular doctor visits (OR = 1.43, 95% CI: 1.23–1.65), and good self-rated health (OR = 1.16, 95% CI: 1.01–1.36) increased the chance of individuals not adopting healthy behaviors compared with their respective reference categories, independently of gender, age, schooling, and economic status. Counseling strategies should consider patient particularities, and health professionals need to be aware of issues that can interfere with the adoption of healthy behaviors of hypertensive patients.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 digital issues and online access to articles
$119.00 per year
only $9.92 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
World Health Organization. Global brief on hypertension: silent killer, global public health crisis. Geneva, Switzerland, 2013. https://www.who.int/cardiovascular_diseases/publications/global_brief_hypertension/en/. [cited 2019 Jun 15]
World Health Organization. Global status report on noncommunicable diseases. Geneva, Switzerland, 2014. https://www.who.int/nmh/publications/ncd-status-report-2014/en/. [cited 2019 Jun 30]
Cheong AT, Sazlina SG, Tong SF, Azah AS, Salmiah S. Poor blood pressure control and its associated factors among older people with hypertension: a cross-sectional study in six public primary care clinics in Malaysia. Malaysian Fam Physician. 2015; 10:19–25. PMC4567889
Lawes CM, Hoorn SV, Rodgers A. Global burden of blood-pressure-related disease, 2001. Lancet 2008;371:1513–8. https://doi.org/10.1016/S0140-6736(08)60655-8
Lobo LAC, Canuto R, Dias-da-Costa JS, Pattussi MP [Time trend in the prevalence of systemic arterial hypertension in Brazil]. Cad Saude Publica. 2017;33. https://doi.org/10.1590/0102-311x00035316
Lessa I. Hipertensão arterial sistêmica no Brasil: tendência temporal [editorial]. Cad Saude Publica. 2010;26:1470. https://doi.org/10.1590/S0102-311X2010000800001
Andrade SS, de A, Stopa SR, Brito AS, Chueri PS, Szwarcwald CL, et al. Self-reported hypertension prevalence in the Brazilian population: analysis of the National Health Survey, 2013. Epidemiol e Serviços Saúde. 2015;24:297–304. https://doi.org/10.5123/S1679-49742015000200012
Gebrezgi MT, Trepka MJ, Kidane EA.Barriers to and facilitators of hypertension management in Asmara, Eritrea: patients’ perspectives.J Heal Popul Nutr. 2017;36:11 https://doi.org/10.1186/s41043-017-0090-4
de Sousa MR, Mourilhe-Rocha R, de Paola AAV, Köhler I, Feitosa GS, Schneider JC, et al. 1st Guidelines of the Brazilian society of cardiology on processes and skills for education in cardiology in Brazil - Executive summary. Arq Bras Cardiol. 2012;98:98–103.
Gontijo M, de F, Ribeiro AQ, Klein CH, Rozenfeld S, Acurcio F. et al. [Use of anti-hypertensive and anti-diabetic drugs by the elderly: a survey in Belo Horizonte, Minas Gerais State, Brazil]. Cad Saude Publica.2012;28:1337–46.
Yang F, Qian D, Hu D. Prevalence, awareness, treatment, and control of hypertension in the older population: results from the multiple national studies on ageing. J Am Soc Hypertens. 2016;10:140–8. https://doi.org/10.1016/j.jash.2015.11.016
Nogueira IC, Santos ZM, de SA, Mont’Alverne DGB, Martins ABT, Magalhães CB, et al. [Effects of exercise on hypertension control in older adults: systematic review]. Rev Bras Geriatr e Gerontol. 2012;15:587–601.
Castro I, Waclawovsky G, Marcadenti A. Nutrition and physical activity on hypertension: implication of current evidence and guidelines. Curr Hypertens Rev. 2015;11:91–9. https://doi.org/10.2174/1573402111666150429170302
Guo J, Zhu Y-C, Chen Y-P, Hu Y, Tang X-W, Zhang B. The dynamics of hypertension prevalence, awareness, treatment, control and associated factors in Chinese adults. J Hypertens. 2015;33:1688–96. https://doi.org/10.1097/HJH.0000000000000594
Malachias MVB, Gomes MAM, Nobre F, Alessi A, Feitosa AD, Coelho EB. 7th Brazilian Guideline of Arterial Hypertension: Chapter 2 - Diagnosis and Classification. Arq Bras Cardiol. 2016; 107:1–83. https://doi.org/10.5935/abc.20160152
Pearce N, Ebrahim S, Mackee M, Lamptey P, Barreto ML, Matheson D, et al. Global prevention and control of NCDs: limitations of the standard approach. J Public Health Policy. 2015;36:408–25. https://doi.org/10.1057/jphp.2015.29
Hankonen N. Psychosocial processes of health behavior change in a lifestyle intervention. National Institute for Health and Welfare. 2011. https://helda.helsinki.fi/bitstream/handle/10138/24850/psychoso.pdf?sequence=3 [cited 2019 Out 02].
Souza-Júnior PRB, de, Freitas MPS, de, Antonaci G, de A, Szwarcwald CL. Sampling design for the National Health Survey, Brazil 2013. Epidemiol e Serviços Saúde. 2015;24:207–16. https://doi.org/10.5123/S1679-49742015000200003
Instituto Brasileiro de Geografia e Estatística (IBGE). Pesquisa Nacional de Saúde - 2013: percepção do estado de saude, estilos de vida e doenças crônicas - Brasil, Grandes Regiões e Unidades da Federação [Internet]. 2014:181. https://biblioteca.ibge.gov.br/visualizacao/livros/liv91110.pdf [cited 2019 Aug 14].
Szwarcwald CL, Malta DC, Pereira CA. Vieira MLFP, Conde WL, Souza Júnior PRB, et al. [National Health Survey in Brazil: design and methodology of application]. Cien Saude Colet. 2014;19:333–42. https://doi.org/10.1590/1413-81232014192.14072012
Damacena GN, Szwarcwald CL, Malta DC, Souza Júnior PRB, Vieira MLFP, Pereira CA. et al. O Process de Desenvolv da Pesqui Nacional de Saúde no Bras, 2013. Epidemiol e Serviços Saúde. 2015;24:197–206. https://doi.org/10.5123/S1679-49742015000200002
National Institute on Alcohol Abuse and Alcoholism. National Institute of Alcohol Abuse and Alcoholism Council approves definition of binge drinking. NIAAA Newsletter. 2004. Winter. Retrieved October 25, 2007. http://pubs.niaaa.nih.gov/publications/Newsletter/winter2004/Newsletter_Number3.htm
Kamakura W, Mazzon A. Alterações na aplicação do Critério Brasil, válidas a partir de 01/06/2019. http://www.abep.org/criterioBr/01_cceb_2019.pdf [cited 2019 Sep 11].
Costa MFF, de L, Peixoto SV, César CC, Malta DC, Moura EC. de. Comportamentos em saúde entre idosos hipertensos, Brasil, 2006. Rev Saude Publica. 2009;43:18–26. https://doi.org/10.1590/S0034-89102009000900004
Firmo JOA, Peixoto SV, Loyola Filho AI, Souza Júnior PRB, Andrade FB, Lima-Costa MF, et al. Comportamentos em saúde e o controle da hipertensão arterial: resultados do ELSI-BRASIL. Cad Saude Publica. 2019;35. https://doi.org/10.1590/0102-311x00091018
Duncan BB, Chor D, Aquino EML, Bensenor IM, Mill JG, Schmidt MI. et al. [Chronic non-communicable diseases in Brazil: priorities for disease management and research]. Rev Saude Publica. 2012;46:126–34. https://doi.org/10.1590/S0034-89102012000700017
Vrdoljak D, Marković BB, Puljak L, Lalić DI, Kranjčević K, Vučak J. Lifestyle intervention in general practice for physical activity, smoking, alcohol consumption and diet in elderly: a randomized controlled trial. Arch Gerontol Geriatr. 2014;58:160–9. https://doi.org/10.1016/j.archger.2013.08.007
Södergren M, Wang WC, Salmon J, Ball K, Crawford D, McNaughton SA. Predicting healthy lifestyle patterns among retirement age older adults in the WELL study: a latent class analysis of sex differences. Maturitas 2014;77:41–6. https://doi.org/10.1016/j.maturitas.2013.09.010
Melonashi E, Shkembi F. A predictive model for physical activity, healthy eating, alcohol drinking, and risky driving among Albanian youth. SAGE Open. 2015;5:215824401558037. https://doi.org/10.1177/2158244015580378
Harvey IS, Alexander K. Perceived social support and preventive health behavioral outcomes among older women. J Cross Cult Gerontol. 2012;27:275–90. https://doi.org/10.1007/s10823-012-9172-3
Barr PJ, Brady SC, Hughes CM, McElnay JC. Public knowledge and perceptions of connected health. J Eval Clin Pr. 2014;20:246–54. https://doi.org/10.1111/jep.12118
Motter FR, Olinto MTA, Paniz VMV. [Evaluation of knowledge on blood pressure levels and chronicity of hypertension among users of a public pharmacy in Southern Brazil]. Cad Saude Publica. 2015;31:395–404. https://doi.org/10.1590/0102-311X00061914
Gilsogamo CA, Oliveira JC, de, Teixeira JCA, Grossi LCN, Moreira MMP, Diniz LO. [Factors that interfere in the hypertension treatment envolvement of patients in the NAHI - Núcleo de Atendimento ao Hipertenso (Center of Support to the hand in the PSF - Programa Saúde da família (Family Health Program)]. Rev Bras Med Família e Comunidade. 2008;4:179–88.
Paula PAB, de, Stephan-Souza AI, Vieira R, de CPA, Alves TNP. [The use of medication in the perception of users Hiperdia Program]. Cien Saude Colet. 2011;16:2623–33. https://doi.org/10.1590/s1413-81232011000500032
Bezerra AS, de M, Lopes J, de L, Barros ALBL de. [Adherence of hypertensive patients to drug treatment]. Rev Bras Enferm. 2014;67:550–5. https://doi.org/10.1590/0034-7167.2014670408.
Araújo J, Ramos E, Lopes C. Lifestyles and self-rated health, in Portuguese elderly from rural and urban areas. Acta Med Port. 2011; 24:79–88. https://www.actamedicaportuguesa.com/revista/index.php/amp/article/view/1524/1109 [cited 2019 May 22]
Szwarcwald CL, Damacena GN, Souza Júnior PRB, Almeida WS, Lima LTM, Malta DC, et al. [Determinants of self-rated health and the influence of healthy behaviors: results from the National Health Survey, 2013]. Rev Bras Epidemiol. 2015;18:33–44. https://doi.org/10.1590/1980-5497201500060004
Patrão AL, Almeida M, da C, Matos SMA, Chor D, Aquino EML. Gender and psychosocial factors associated with healthy lifestyle in the Brazilian Longitudinal Study of Adult Health (ELSA-Brasil) cohort: a cross-sectional study. BMJ Open 2017;7:e015705. https://doi.org/10.1136/bmjopen-2016-015705
Barreto Junior IF, França CRA, Dias EC. Percepção do estado de saúde, estilo de vida e doenças crônicas: uma comparação entre Brasil e estado de São Paulo. Fundação Sistema Estadual de Análise de Dados. São Paulo-SP, 2015. https://www.seade.gov.br/wp-content/uploads/2016/01/Primeira_Analise_33_dez_final.pdf [cited 2019 Jul 20]
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
V. Dionato, F.A., Enes, C.C. & Nucci, L.B. Factors associated with not adopting healthy behavior among hypertensive individuals: a population-based study in Brazil. J Hum Hypertens 35, 718–725 (2021). https://doi.org/10.1038/s41371-020-0382-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41371-020-0382-9