Abstract
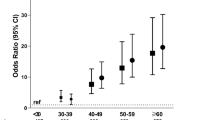
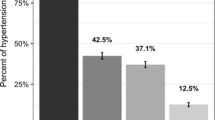
This study investigated rural–urban variation in the prevalence of self-reported hypertension and its risk factors among reproductive-age women in Kenya. The 2014 nationally representative Kenya Demographic and Health Survey (KDHS) data were used in this analysis. The survey adopted a multistage, geographically clustered, and probability-based sampling approach. Multivariable logistic regression was performed to assess the association between risk factors and self-reported hypertension. Overall, 9.38% of the women were hypertensive with higher prevalence among urban 11.61%, compared to rural women, 7.86%. Older age, obesity, having diabetes, and increased the odds of hypertension in both rural and urban areas. We also observed that the odds of hypertension differed by ethnic group. High wealth status was a significant correlate only among urban women with women from rich and richest wealth groups had 2–2.3 times higher odds of hypertension compared to the poor and poorest wealth groups. Women with diabetes had 22 times higher odds of hypertension in both in rural and urban areas compared to women without diabetes. In conclusion, our study found that an estimated 1 out of 10 Kenyan women have hypertension. We believe that this study contributes to better understanding of regional variation of hypertension prevalence and risk factors for reproductive women in Kenya. Future studies should seek to develop evidence-based hypertension prevention and management interventions that are targeted and tailored for urban and rural women in Kenya.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 digital issues and online access to articles
$119.00 per year
only $9.92 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Mudie K, Jin MM, Tan LK, Addo J, dos-Santos-Silva I, Quint J, et al. Non-communicable diseases in sub-Saharan Africa: a scoping review of large cohort studies. J Glob Health. 2019;9. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6684871/.
Engelgau MM, Rosenthal JP, Newsome BJ, Price L, Belis D, Mensah GA. Noncommunicable diseases in low-and middle-income countries: a strategic approach to develop a global implementation research workforce. Glob Heart. 2018;13:131–7.
World Health Organization G. Noncommunicable diseases. 2020. https://www.who.int/en/news-room/fact-sheets/detail/noncommunicable-diseases.
Frieden TR, Jaffe MG. Saving 100 million lives by improving global treatment of hypertension and reducing cardiovascular disease risk factors. J Clin Hypertens. 2018;20:208–11.
Akinboboye O, Idris O, Akinkugbe O. Trends in coronary artery disease and associated risk factors in sub-Saharan Africans. J Hum Hypertens. 2003;17:381–7.
Joshi MD, Ayah R, Njau EK, Wanjiru R, Kayima JK, Njeru EK, et al. Prevalence of hypertension and associated cardiovascular risk factors in an urban slum in Nairobi, Kenya: a population-based survey. BMC Public Health. 2014;14:1.
Irazola VE, Gutierrez L, Bloomfield G, Carrillo-Larco RM, Dorairaj P, Gaziano T, et al. Hypertension prevalence, awareness, treatment, and control in selected LMIC communities: results from the NHLBI/UHG network of Centers of Excellence for chronic diseases. Glob Heart. 2016;11:47–59.
van de Vijver SJ, Oti SO, Agyemang C, Gomez GB, Kyobutungi C. Prevalence, awareness, treatment and control of hypertension among slum dwellers in Nairobi, Kenya. J Hypertens. 2013;31:1018–24.
Jenson A, Omar AL, Omar MA, Rishad AS, Khoshnood K. Assessment of hypertension control in a district of Mombasa. Kenya Glob Public Health. 2011;6:293–306.
Murray CJ, Barber RM, Foreman KJ, Ozgoren AA, Abd-Allah F, Abera SF, et al. Global, regional, and national disability-adjusted life years (DALYs) for 306 diseases and injuries and healthy life expectancy (HALE) for 188 countries, 1990–2013: quantifying the epidemiological transition. Lancet. 2015;386:2145–91.
Omran AR. The epidemiologic transition: a theory of the epidemiology of population change. Milbank Q. 2005;83:731–57.
Mathenge W, Foster A, Kuper H. Urbanization, ethnicity and cardiovascular risk in a population in transition in Nakuru, Kenya: a population-based survey. BMC Public Health. 2010;10:1.
Smith SM, Mensah GA. Population aging and implications for epidemic cardiovascular disease in Sub-Saharan Africa. Ethn Dis. 2003;13:S2–77.
Mohamed SF, Mutua MK, Wamai R, Wekesah F, Haregu T, Juma P, et al. Prevalence, awareness, treatment and control of hypertension and their determinants: results from a national survey in Kenya. BMC Public Health. 2018;18:1219.
Chowdhury MAB, Uddin MJ, Haque MR, Ibrahimou B. Hypertension among adults in Bangladesh: evidence from a national cross-sectional survey. BMC Cardiovasc Disord. 2016;16:22.
Mkuu RS, Epnere K, Chowdhury MAB. Prevalence and predictors of overweight and obesity among kenyan women. Prev Chronic Dis. 2018;15:E44.
Chowdhury MAB, Adnan MM, Hassan MZTrends. prevalence and risk factors of overweight and obesity among women of reproductive age in Bangladesh: a pooled analysis of five national cross-sectional surveys. BMJ Open. 2018;8:e018468.
Mkuu RS, Gilreath TD, Wekullo C, Reyes GA, Harvey IS. Social determinants of hypertension and type-2 diabetes in Kenya: A latent class analysis of a nationally representative sample. PloS ONE. 2019;14. https://pubmed.ncbi.nlm.nih.gov/31425539/.
Saxena N, Bava AK, Nandanwar Y. Maternal and perinatal outcome in severe preeclampsia and eclampsia. Int J Reprod Contracept Obstet Gynecol. 2016;5.7:2171–6.
Chowdhury MAB, Mkuu RS, Epnere K, Cisse-Egbuonye N, Harvey I, Haque MA, et al. Risk factors for hypertension in early to mid-life Kenyans: the Kenya Demographic and Health Survey. Ann Behav Med. 2017;51:S1–2867.
Yang Q, Song C, Jiang J, Chen Y, Liang S, Ma N, et al. Association of reproductive history with hypertension and prehypertension in Chinese postmenopausal women: a population-based cross-sectional study. Hypertens Res. 2018;41:66–74.
Soubeiga JK, Millogo T, Bicaba BW, Doulougou B, Kouanda S. Prevalence and factors associated with hypertension in Burkina Faso: a countrywide cross-sectional study. BMC Public Health. 2017;17:64.
Acheampong K, Nyamari JM, Ganu D, Appiah S, Pan X, Kaminga A, et al. Predictors of hypertension among adult female population in Kpone-Katamanso District, Ghana. Int J Hypertens. 2019;2019:1876060.
Chowdhury MAB, Uddin MJ, Khan HM, Haque MR. Type 2 diabetes and its correlates among adults in Bangladesh: a population based study. BMC Public Health. 2015;15:1070.
Osman S, Costanian C, Annan NB, Fouad FM, Jaffa M, Sibai AM. Urbanization and socioeconomic disparities in hypertension among older adult women in Sudan. Ann Glob Health. 2019;85:1.
Cham B, Scholes S, Ng Fat L, Badjie O, Mindell JS. Burden of hypertension in the Gambia: evidence from a national World Health Organization (WHO) STEP survey. Int J Epidemiol. 2018;47:860–71.
Rush KL, Goma FM, Barker JA, Ollivier RA, Ferrier MS, Singini D. Hypertension prevalence and risk factors in rural and urban Zambian adults in western province: a cross-sectional study. Pan Afr Med J. 2018;30. https://pubmed.ncbi.nlm.nih.gov/30344881/.
Kodaman N, Aldrich MC, Sobota R, Asselbergs FW, Poku KA, Brown NJ, et al. Cardiovascular disease risk factors in Ghana during the rural-to-urban transition: a cross-sectional study. PLoS ONE. 2016;11.
Monda KL, Gordon-Larsen P, Stevens J, Popkin BM. China’s transition: the effect of rapid urbanization on adult occupational physical activity. Soc Sci Med. 2007;64:858–70.
Gissing SC, Pradeilles R, Osei-Kwasi HA, Cohen E, Holdsworth M. Drivers of dietary behaviours in women living in urban Africa: a systematic mapping review. Public Health Nutr. 2017;20:2104–13.
Demmler KM, Klasen S, Nzuma JM, Qaim M. Supermarket purchase contributes to nutrition-related non-communicable diseases in urban Kenya. PloS ONE. 2017;12. https://pubmed.ncbi.nlm.nih.gov/28934333/.
Franklin SS, Larson MG, Khan SA, Wong ND, Leip EP, Kannel WB, et al. Does the relation of blood pressure to coronary heart disease risk change with aging? The Framingham Heart Study. Circulation. 2001;103:1245–9.
Acheampong K, Nyamari JM, Ganu D, Appiah S, Pan X, Kaminga A, et al. Predictors of hypertension among adult female population in Kpone-Katamanso District, Ghana. Int J Hypertens. 2019;2019:1876060.
Hunter-Adams J, Battersby J, Oni T. Food insecurity in relation to obesity in peri-urban Cape Town, South Africa: Implications for diet-related non-communicable disease. Appetite. 2019;137:244–9.
Oyando R, Njoroge M, Nguhiu P, Kirui F, Mbui J, Sigilai A, et al. Patient costs of hypertension care in public health care facilities in Kenya. Int J Health Plan Manag. 2019;34:e1166–78.
Acknowledgements
We would like to thank MEASURE DHS for allowing us to use the data set. We are also thankful to the editor and reviewers for their valuable comments and suggestion, which led to significant improvements of the paper.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Chowdhury, M.A.B., Epnere, K., Haque, M.A. et al. Urban rural differences in prevalence and risk factors of self-reported hypertension among Kenyan women: a population-based study. J Hum Hypertens 35, 912–920 (2021). https://doi.org/10.1038/s41371-020-00435-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41371-020-00435-x
This article is cited by
-
Development and external validation of a diagnostic model for cardiometabolic-based chronic disease : results from the China health and retirement longitudinal study (CHARLS)
BMC Cardiovascular Disorders (2023)
-
Uncontrolled hypertension among tobacco-users: women of prime childbearing age at risk in India
BMC Women's Health (2021)