Abstract
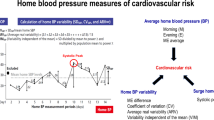
Arterial hypertension (AHT) is a major risk factor for stroke, yet blood pressure (BP) goals thereafter remain uncertain. Although additional prognostic value of 24-hour ambulant BP monitoring (ABPM) is acknowledged, its clinical impacts remain limited. We suspected that routine ABPM could identify characteristic circadian BP patterns in different brain lesion types, the knowledge of which might, in turn, be helpful in improving overall BP management in patients after stroke. In our study, we compared cardiovascular parameters derived from ABPM and traditional blood pressure measurements (TBPM) among 105 stroke survivors who entered our inpatient neuro-rehabilitation program. The mean age of mostly male (64.8%) patients was 71 ± 12 years. Ischemic strokes were predominant (75.2%). Despite normotensive systolic BP means in TBPM (133.5 ± 18.2 mmHg) and ABPM (24 h: 122.8 ± 14.7 mmHg), AHT persisted in up to 67.6% of all patients, with ABPM uncovering nocturnal systolic non- or reversed dipping in 89.5% and 53.3%, respectively. The latter was predominant (85.7%) in the hemorrhagic subgroup which also displayed lower daytime SBP than the ischemic one (ABPM: 117.1 ± 11.8 vs 124.7 ± 14.7 mmHg, p = 0.033). Further differences were present among distinct brain lesion types. Sufficient dippers were younger (58 ± 12 vs 75 ± 11 years, p < 0.001), but adjusting for age yielded no independent correlations. In spite of normotensive daytime BP measurements, ABPM detects latent AHT and insufficient nocturnal BP dipping after the acute phase of stroke. Further studies are needed to elucidate the role of increased nocturnal BP in patients after stroke.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 digital issues and online access to articles
$119.00 per year
only $9.92 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Williams B, Mancia G, Spiering W, Agabiti Rosei E, Azizi M, Burnier M, et al. 2018 ESC/ESH guidelines for the management of arterial hypertension. Eur Heart J. 2018;39:3021–104.
Pats Collaborating Group. Post-stroke antihypertensive treatment study. A preliminary result. Chin Med J (Engl). 1995;108:710–7.
Progress Collaborative Group. Randomised trial of a perindopril-based blood-pressure-lowering regimen among 6,105 individuals with previous stroke or transient ischaemic attack. Lancet. 2001;358:1033–41.
Liu L, Wang Z, Gong L, Zhang Y, Thijs L, Staessen JA, et al. Blood pressure reduction for the secondary prevention of stroke: a Chinese trial and a systematic review of the literature. Hypertens Res. 2009;32:1032–40.
Katsanos AH, Filippatou A, Manios E, Deftereos S, Parissis J, Frogoudaki A, et al. Blood pressure reduction and secondary stroke prevention: a systematic review and metaregression analysis of randomized clinical trials. Hypertension. 2017;69:171–9.
Kernan WN, Ovbiagele B, Black HR, Bravata DM, Chimowitz MI, Ezekowitz MD, et al. Guidelines for the prevention of stroke in patients with stroke and transient ischemic attack: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2014;45:2160–236.
SPSS Group, Benavente OR, Coffey CS, Conwit R, Hart RG, McClure LA, et al. Blood-pressure targets in patients with recent lacunar stroke: the SPS3 randomised trial. Lancet. 2013;382:507–15.
Kakaletsis N, Ntaios G, Milionis H, Haidich AB, Makaritsis K, Savopoulos C, et al. Prognostic value of 24-h ABPM in acute ischemic stroke for short-, medium-, and long-term outcome: a systematic review and meta-analysis. Int J Stroke. 2015;10:1000–7.
Papaioannou TG, Karageorgopoulou TD, Sergentanis TN, Protogerou AD, Psaltopoulou T, Sharman JE, et al. Accuracy of commercial devices and methods for noninvasive estimation of aortic systolic blood pressure a systematic review and meta-analysis of invasive validation studies. J Hypertens. 2016;34:1237–48.
Kario K, Pickering TG, Matsuo T, Hoshide S, Schwartz JE, Shimada K. Stroke prognosis and abnormal nocturnal blood pressure falls in older hypertensives. Hypertension. 2001;38:852–7.
Ohkubo T, Hozawa A, Yamaguchi J, Kikuya M, Ohmori K, Michimata M, et al. Prognostic significance of the nocturnal decline in blood pressure in individuals with and without high 24-h blood pressure: the Ohasama study. J Hypertens. 2002;20:2183–9.
Ben-Dov IZ, Kark JD, Ben-Ishay D, Mekler J, Ben-Arie L, Bursztyn M. Predictors of all-cause mortality in clinical ambulatory monitoring: unique aspects of blood pressure during sleep. Hypertension. 2007;49:1235–41.
Fagard RH, Thijs L, Staessen JA, Clement DL, De Buyzere ML, De Bacquer DA. Prognostic significance of ambulatory blood pressure in hypertensive patients with history of cardiovascular disease. Blood Press Monit. 2008;13:325–32.
Fagard RH, Thijs L, Staessen JA, Clement DL, De Buyzere ML, De Bacquer DA. Night-day blood pressure ratio and dipping pattern as predictors of death and cardiovascular events in hypertension. J Hum Hypertens. 2009;23:645–53.
Yamamoto Y, Akiguchi I, Oiwa K, Hayashi M, Kimura J. Adverse effect of nighttime blood pressure on the outcome of lacunar infarct patients. Stroke. 1998;29:570–6.
Bravata DM, Daggy J, Brosch J, Sico JJ, Baye F, Myers LJ, et al. Comparison of risk factor control in the year after discharge for ischemic stroke versus acute myocardial infarction. Stroke. 2018;49:296–303.
Jain S, Namboodri KK, Kumari S, Prabhakar S. Loss of circadian rhythm of blood pressure following acute stroke. BMC Neurol. 2004;4:1
Castilla-Guerra L, Espino-Montoro A, Fernandez-Moreno MC, Lopez-Chozas JM. Abnormal blood pressure circadian rhythm in acute ischaemic stroke: are lacunar strokes really different? Int J Stroke. 2009;4:257–61.
Sander D, Klingelhofer J. Changes of circadian blood pressure patterns and cardiovascular parameters indicate lateralization of sympathetic activation following hemispheric brain infarction. J Neurol. 1995;242:313–8.
Blissitt PA. Sleep-disordered breathing after stroke: nursing implications. Stroke. 2017;48:e81–4.
Hla KM, Young T, Finn L, Peppard PE, Szklo-Coxe M, Stubbs M. Longitudinal association of sleep-disordered breathing and nondipping of nocturnal blood pressure in the Wisconsin Sleep Cohort Study. Sleep. 2008;31:795–800.
Acknowledgements
We thank Thomas Gaisl, MD (Department of Pulmonology, University Hospital Zurich, Switzerland) for his cross-disciplinary contribution.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethics/registration
The study was approved by the Cantonal Ethics Committee of Zurich in Switzerland (BASEC-No.: 2016-00247; submission viewable upon request under www.swissethics.ch). The need for patient consent was waived by the board.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Rejmer, P., Palla, A., Schulz, E.G. et al. Ambulatory blood pressure monitoring on admission in survivors of recent stroke entering inpatient rehabilitation. J Hum Hypertens 34, 364–371 (2020). https://doi.org/10.1038/s41371-019-0237-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41371-019-0237-4