Abstract
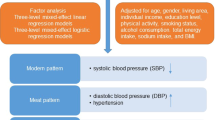
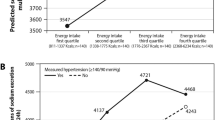
The desirable distribution of three major nutrients intake to prevent hypertension is not established. This study is to clarify the relationship between the prevalence of hypertension and the rate of intake of three major nutrients. This is a large-scale cross-sectional study. We analyzed Japanese subjects who had their annual medical examination at St Luke’s International Hospital, Tokyo from January 2004 to June 2010. The amount of three major nutrients and salt intake were checked by a questionnaire method, and this study clarified the relationship between the prevalence of hypertension and the rate of three major nutrients with adjustment for age, sex, body mass index (BMI), smoking, dyslipidemia, diabetes mellitus, hyperuricemia, and salt intake. We analyzed 89,851 subjects. Of those, the number of hypertensive subjects was 13,926 (15.5%). The hypertensive group had significantly higher rate of calories from protein (19.7% vs. 19.4%, P < 0.001) but lower rate of calories from fat (16.1% vs. 16.4%, P < 0.001) than that in the non-hypertensive group. The rate of calories from carbohydrate was almost the same between the two groups (64.2% vs. 64.2%). After multiple adjustments, high rate of calories from protein was associated with high prevalence of hypertension (odds ratio: 1.011, 95% confidence interval (CI), 1.005–1.017), as well as aging, male, high BMI, smoking habits, dyslipidemia, diabetes mellitus, and hyperuricemia. High rate of calories from protein could be associated with high risk of hypertension. Therefore, protein-restricted diet may have a favorable effect in preventing hypertension and cardiovascular diseases.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 digital issues and online access to articles
$119.00 per year
only $9.92 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Shimamoto K, Ando K, Fujita T, Hasebe N, Higaki J, Horiuchi M, et al. The Japanese Society of Hypertension Guidelines for the Management of Hypertension (JSH 2014). Hypertens Res. 2014;37:253–390.
Mancia G, Fagard R, Narkiewicz K, Redon J, Zanchetti A, Bohm M, et al. 2013 ESH/ESC guidelines for the management of arterial hypertension: the Task Force for the Management of Arterial Hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). Eur Heart J. 2013;34:2159–219.
Lagiou P, Sandin S, Lof M, Trichopoulos D, Adami HO, Weiderpass E. Low carbohydrate–high protein diet and incidence of cardiovascular diseases in Swedish women: prospective cohort study. BMJ. 2012;344:e4026.
Bravata DM, Sanders L, Huang J, Krumholz HM, Olkin I, Gardner CD, et al. Efficacy and safety of low-carbohydrate diets: a systematic review. JAMA. 2003;289:1837–50.
Samaha FF, Iqbal N, Seshadri P, Chicano KL, Daily DA, McGrory J, et al. A low-carbohydrate as compared with a low-fat diet in severe obesity. N Engl J Med. 2003;348:2074–81.
Dehghan M, Mente A, Zhang X, Swaminathan S, Li W, Mohan V, et al. Associations of fats and carbohydrate intake with cardiovascular disease and mortality in 18 countries from five continents (PURE): a prospective cohort study. Lancet. 2017. https://www.bmj.com/content/344/bmj.e4026.
Astrup A, Meinert Larsen T, Harper A. Atkins and other low-carbohydrate diets: hoax or an effective tool for weight loss? Lancet. 2004;364:897–9.
Abais-Battad JM, Lund H, Fehrenbach DJ, Dasinger JH, Mattson DL. Rag1-null Dahl SS rats reveal that adaptive immune mechanisms exacerbate high protein-induced hypertension and renal injury. Am J Physiol Regul Integr Comp Physiol. 2018;315:R28–R35.
Shaykh M, Pegoraro AA, Mo W, Arruda JA, Dunea G, Singh AK. Carbamylated proteins activate glomerular mesangial cells and stimulate collagen deposition. J Lab Clin Med. 1999;133:302–8.
Kuwabara M, Niwa K, Nishi Y, Mizuno A, Asano T, Masuda K, et al. Relationship between serum uric acid levels and hypertension among Japanese individuals not treated for hyperuricemia and hypertension. Hypertens Res. 2014;37:785–9.
Kuwabara M, Motoki Y, Ichiura K, Fujii M, Inomata C, Sato H, et al. Association between toothbrushing and risk factors for cardiovascular disease: a large-scale, cross-sectional Japanese study. BMJ Open. 2016;6:e009870.
Kuwabara M, Niwa K, Ohtahara A, Hamada T, Miyazaki S, Mizuta E, et al. Prevalence and complications of hypouricemia in a general population: a large-scale cross-sectional study in Japan. PLoS ONE. 2017;12:e0176055.
Kuwabara M, Niwa K, Nishihara S, Nishi Y, Takahashi O, Kario K, et al. Hyperuricemia is an independent competing risk factor for atrial fibrillation. Int J Cardiol. 2017;231:137–42.
Grootenhuis PA, Westenbrink S, Sie CM, de Neeling JN, Kok FJ, Bouter LM. A semiquantitative food frequency questionnaire for use in epidemiologic research among the elderly: validation by comparison with dietary history. J Clin Epidemiol. 1995;48:859–68.
Fujiwara N, Tokudome S. Reproducibility of self-administered questionnaire in epidemiological surveys. J Epidemiol. 1997;7:61–9.
Sasaki S, Yanagibori R, Amano K. Self-administered diet history questionnaire developed for health education: a relative validation of the test-version by comparison with 3-day diet record in women. J Epidemiol. 1998;8:203–15.
International Expert C. International Expert Committee report on the role of the A1C assay in the diagnosis of diabetes. Diabetes Care. 2009;32:1327–34.
Teramoto T, Sasaki J, Ishibashi S, Birou S, Daida H, Dohi S, et al. Executive summary of the Japan Atherosclerosis Society (JAS) guidelines for the diagnosis and prevention of atherosclerotic cardiovascular diseases in Japan—2012 version. J Atheroscler Thromb. 2013;20:517–23.
Lelong H, Blacher J, Baudry J, Adriouch S, Galan P, Fezeu L, et al. Individual and combined effects of dietary factors on risk of incident hypertension: prospective analysis from the NutriNet-Sante Cohort. Hypertension. 2017;70:712–20.
Acknowledgements
We thank all staff in Center for Preventive Medicine, St Luke’s International Hospital, for assistance with data collection. Dr Kuwabara reports the grant for studying abroad from Federation of National Public Service Personnel Mutual Aid Association in Japan.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kuwabara, M., Niwa, K., Ohno, M. et al. High rate of calories from protein is associated with higher prevalence of hypertension. J Hum Hypertens 33, 340–344 (2019). https://doi.org/10.1038/s41371-019-0162-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41371-019-0162-6