Abstract
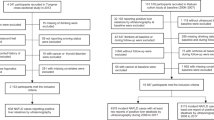
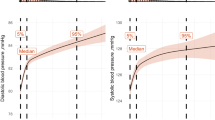
To date, there are few studies in Asian populations on the association between snoring (a major clinical symptom of sleep apnea) and hypertension. This study aims to examine whether snoring frequency is associated with blood pressure and hypertension in the general Japanese population, after adjustment for major confounding factors. A cross-sectional study of 2021 middle-aged Japanese men and women enrolled in the Toon Health Study between 2009−2012 was conducted. Snoring frequency was assessed using a self-reported questionnaire, and was classified into four categories: never, ≤2 times/week, ≥3 times/week, and unknown. Multivariable regression coefficients for each snoring category were calculated for systolic and diastolic blood pressure, and their odds ratios (ORs) and 95% confidence intervals (95% CIs) for hypertension were calculated after adjusting for major confounding factors. The same analyses were also conducted after stratification by several major confounding factors. Multivariable-adjusted means of systolic and diastolic blood pressure among individuals who snored ≥3 times/week were 4.57 mmHg and 2.58 mmHg higher, respectively, than in individuals who never snored (p < 0.05). The multivariable-adjusted OR (95% CI) for hypertension in the group that snored ≥3 times/week was 1.79 (1.29–2.48), compared with the group that never snored. We also found a significant positive association between snoring frequency and hypertension not only in normal and overweight individuals, but also in lean individuals (body mass index ≤22.8 kg/m2). Higher snoring frequency was associated with higher blood pressure and hypertension among both lean and non-lean Japanese.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 digital issues and online access to articles
$119.00 per year
only $9.92 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Enright PL, Newman AB, Wahl PW, Manolio TA, Haponik EF, Boyle PJ. Prevalence and correlates of snoring and observed apneas in 5,201 older adults. Sleep. 1996;19:531–8.
Hori M, Kitamura A, Kiyama M, Imano H, Yamagishi K, Cui R, et al. Fifty-year time trends in blood pressures, body mass index and their relations in a Japanese Community: The Circulatory Risk in Communities Study (CIRCS). J Atheroscler Thromb. 2017;24:518–29.
Ohira T, Iso H. Cardiovascular disease epidemiology in Asia: an overview. Circ J. 2013;77:1646–52.
Li D, Liu D, Wang X, He D. Self-reported habitual snoring and risk of cardiovascular disease and all-cause mortality. Atherosclerosis. 2014;235:189–95.
Thomas GN, Jiang CQ, Lao XQ, McGhee SM, Zhang WS, Schooling CM, et al. Snoring and vascular risk factors and disease in a low-risk Chinese population: the Guangzhou Biobank Cohort Study. Sleep. 2006;29:896–900.
Kim J, Yi H, Shin KR, Kim JH, Jung KH, Shin C. Snoring as an independent risk factor for hypertension in the nonobese population: the Korean Health and Genome Study. Am J Hypertens. 2007;20:819–24.
Corbo GM, Forastiere F, Agabiti N, Baldacci S, Farchi S, Pistelli R, et al. Rhinitis and snoring as risk factors for hypertension in post-menupausal women. Respir Med. 2006;100:1368–73.
Jennum P, Hein HO, Suadicani P, Gyntelberg F. Cardiovascular risk factors in snorers. a cross-sectional study of 3,323 men aged 54 to 74 years: the Copenhagen Male Study. Chest. 1992;102:1371–6.
Hu FB, Willett WC, Colditz GA, Ascherio A, Speizer FE, Rosner B, et al. Prospective study of snoring and risk of hypertension in women. Am J Epidemiol. 1999;150:806–16.
OECD (2014) ObesityUpdate (Accessed April 14, 2017, at http://www.oecd.org/health/Obesity-Update-2014.pdf).
Tanno S, Tanigawa T, Maruyama K, Eguchi E, Abe T, Saito I. Sleep-related intermittent hypoxia is associated with decreased psychomotor vigilance in Japanese community residents. Sleep Med. 2017;29:7–12.
Saito I, Hitsumoto S, Maruyama K, Eguchi E, Kato T, Okamoto A, et al. Impact of heart rate variability on C-reactive protein concentrations in Japanese adult nonsmokers: the Toon Health Study. Atherosclerosis. 2016;244:79–85.
Nikolaus C. Using the Berlin Questionnaire to identify patients at risk for the sleep apnea syndrome. Ann Intern Med. 1999;131:485–91.
WHO. Obesity: preventing and managing the global epidemic. Report of a WHO Consultation. WHO Technical Report Series 894. Geneva: World Health Organization, 2000.
Ishikawa-Takata K, Naito Y, Tanaka S, Ebine N, Tabata I. Use of doubly labeled water to validate a physical activity questionnaire developed for the Japanese population. J Epidemiol. 2011;21:114–21.
Young T, Shahar E, Nieto FJ, Redline S, Newman AB, Gottlieb DJ, et al. Predictors of sleep-disordered breathing in community-dwelling adults: the Sleep Heart Health Study. Arch Intern Med. 2002;162:893–900.
Satoh A, Arima H, Ohkubo T, Nishi N, Okuda N, Ae R, et al. Associations of socioeconomic status with prevalence, awareness, treatment, and control of hypertension in a general Japanese population: NIPPON DATA2010. J Hypertens. 2017;35:401–8.
Molloy GJ, Stamatakis E, Randall G, Hamer M. Marital status, gender and cardiovascular mortality: behavioural, psychological distress and metabolic explanations. Soc Sci Med. 2009;69:223–8.
Somers VK, Dyken ME, Clary MP, Abboud FM. Sympathetic neural mechanisms in obstructive sleep apnea. J Clin Invest. 1995;96:1897–904.
Carlson JT, Hender J, Elam M, Ejnell H, Sellgren J, Wallin BG. Augmentated resting sympathetic activity in awake patients with obstructive sleep apnea. Chest. 1993;103:1763–8.
Kraiczi H, Hedner J, Peker Y, Carlson J. Increased vasoconstrictor sensitivity in obstructive sleep apnea. J Appl Physiol. 2000;89:493–8.
Schulz R, Mahmoudi S, Hattar K, Sibelius U, Olschewski H, Mayer K, et al. Enhanced release of superoxide from polymorphonuclear neutrophils in obstructive sleep apnea. Impact of continuous positive airway pressure therapy. Am J Respir Crit Care Med. 2000;162:566–70.
Rangemark C, Hedner JA, Carlson JT, Gleerup G, Winter K. Platelet function and fibrinolytic activity in hypertensive and normotensive sleep apnea patients. Sleep. 1995;18:188–94.
Simon DI, Simon NM. Plasminogen activator inhibitor-1: a novel therapeutic target for hypertension? Circulation. 2013;128:2286–8.
Gozal D, Kheirandish L. Oxidant stress and inflammation in the snoring child: confluent pathways to upper airway pathogenesis and end-organ morbidity. Sleep Med Rev. 2006;10:83–96.
Puig F, Rico F, Almendros I, Montserrat JM, Navajas D, Farre R. Vibration enhances interleukin-8 release in a cell model of snoringinduced airway inflammation. Sleep. 2005;28:1312–6.
Tanigawa T, Tachibana N, Yamagishi K, Muraki I, Kudo M, Ohira T, et al. Relationship between sleep-disordered breathing and blood pressure levels in community-based samples of Japanese men. Hypertens Res. 2004;27:479–84.
Cui R, Tanigawa T, Sakurai S, Yamagishi K, Imano H, Ohira T, et al. Associations of sleep-disordered breathing with excessive daytime sleepiness and blood pressure in Japanese women. Hypertens Res. 2008;31:501–6.
Nagayoshi M1, Tanigawa T, Yamagishi K, Sakurai S, Kitamura A, Kiyama M. etc. Self-reported snoring frequency and incidence of cardiovascular disease: the Circulatory Risk in Communities Study (CIRCS). J Epidemiol. 2012;22:295–301.
Acknowledgements
This study was supported in part by Grants-in-Aid for Scientific Research from The Ministry of Education, Culture, Sports, Science and Technology of Japan (Grants-in-Aid for Research B, no 22390134 in 2010–2012 and 25293142 in 2013–2015, and Health and Labor Sciences Research Grants from the Ministry of Health, Welfare and Labor, Japan (Comprehensive Research on Life-Style Related Diseases including Cardiovascular Diseases and Diabetes Mellitus, no 201021038A in 2010–2012). The authors are grateful to the staff and participants of the Toon Health Study for their valuable contributions.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Goto, R., Tanigawa, T., Maruyama, K. et al. Associations of snoring frequency with blood pressure among the lean Japanese population: the Toon Health Study. J Hum Hypertens 34, 271–277 (2020). https://doi.org/10.1038/s41371-018-0148-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41371-018-0148-9
This article is cited by
-
Snoring might be a warning sign for metabolic syndrome in nonobese Korean women
Scientific Reports (2023)