Abstract
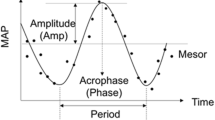
An exaggerated morning blood pressure surge (MBPS) has independent predictive value for cardiovascular mortality and is suggested to be prevalent in elderly hypertensive patients: men and white populations. To better understand the MBPS profile in a young and normotensive population, we evaluated the MBPS in young adults and explored associations with demographic, cardiovascular and health behaviour measurements. We included 845 black (n = 439) and white (n = 406) men and women aged between 20 and 30 years. We calculated the sleep-trough and dynamic morning surge, and compared demographic data, health behaviours and ambulatory blood pressure according to MBPS quartiles. In the total group, higher waist circumference, socioeconomic score, lean mass, ambulatory blood pressure (24-h, daytime blood pressure) and increased night-time dipping (all p < 0.05) were found in the highest sleep-trough and dynamic morning surge quartiles. In the total white group, particularly men, both sleep-trough and dynamic morning surge were higher than the black group (all p < 0.013). More black participants were non-dippers than whites (44% vs 34%; p = 0.004). In multivariable adjusted regression in the total group, we found no consistent associations of MBPS with demographic and health behaviour measurements. MBPS related independently and positively with night-time percentage dipping in all ethnic groups (all p < 0.01). Ethnic differences in MBPS is evident in young adults, with a higher, but normal MBPS in white men. A non-dipping night-time pattern in young black adults (with reduced MBPS) and a higher MBPS (observed in dippers) may serve as potential risk factors for cardiovascular disease.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 digital issues and online access to articles
$119.00 per year
only $9.92 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
Change history
19 November 2018
In the article “Morning blood pressure surge in young black and white adults: The African-PREDICT Study” by Gontse Gratitude Mokwatsi, Aletta Elisabeth Schutte, Catharina Martha Cornelia Mels and Ruan Kruger which appeared in ‘Journal of Human Hypertension’ (2018) volume 32, DOI 10.1038/s41371-018-0089-3, the authors regret that they mentioned erroneously that none of their study participants had an exaggerated morning blood pressure surge. They would like to point out that 40 participants in their study population had an exaggerated sleep-trough surge whereas 128 had an exaggerated dynamic surge.
References
Mc Causland FR, McMullan CJ, Sacks FM, Forman JP. Race, plasma renin activity, and morning blood pressure surge—results from the dietary approaches to stop hypertension trial. Am J Hypertens. 2013;27:530–6.
Kario K. Morning surge in blood pressure and cardiovascular risk evidence and perspectives. Hypertension. 2010;56:765–73.
Kario K. Vascular damage in exaggerated morning surge in blood pressure. Hypertension. 2007;49:771–2.
Neutel J, Schumacher H, Gosse P, Lacourciere Y, Williams B. Magnitude of the early morning blood pressure surge in untreated hypertensive patients: a pooled analysis. Int J Clin Pract. 2008;62:1654–63.
Yano Y, Kario K. Nocturnal blood pressure, morning blood pressure surge, and cerebrovascular events. Curr Hypertens Rep. 2012;14:219–27.
Caliskan M, Caliskan Z, Gullu H, Keles N, Bulur S, Turan Y, et al. Increased morning blood pressure surge and coronary microvascular dysfunction in patient with early stage hypertension. J Am Soc Hypertens. 2014;8:652–9.
Shimizu M, Ishikawa J, Yano Y, Hoshide S, Shimada K, Kario K. The relationship between the morning blood pressure surge and low-grade inflammation on silent cerebral infarct and clinical stroke events. Atherosclerosis. 2011;219:316–21.
Amici A, Cicconetti P, Sagrafoli C, Baratta A, Passador P, Pecci T, et al. Exaggerated morning blood pressure surge and cardiovascular events. A 5-year longitudinal study in normotensive and well-controlled hypertensive elderly. Arch Gerontol Geriatr. 2009;49:e105–9.
Dodt C, Breckling U, Derad I, Fehm HL, Born J. Plasma epinephrine and norepinephrine concentrations of healthy humans associated with nighttime sleep and morning arousal. Hypertension. 1997;30:71–6.
Kaplan NM. Morning surge in blood pressure. Circulation. 2003;107:1347.
Opie LH. Heart physiology: from cell to circulation. Lippincott Williams & Wilkins; 2004. p. 200.
Klabunde R. Cardiovascular physiology concepts. Lippincott Williams & Wilkins; 2011. p. 89.
Ohira T, Tanigawa T, Tabata M, Imano H, Kitamura A, Kiyama M, et al. Effects of habitual alcohol intake on ambulatory blood pressure, heart rate, and its variability among Japanese men. Hypertension. 2009;53:13–9.
Pardell H, Rodicio JL. High blood pressure, smoking and cardiovascular risk. J Hypertens. 2005;23:219–21.
Leary AC, Struthers AD, Donnan PT, MacDonald TM, Murphy MB. The morning surge in blood pressure and heart rate is dependent on levels of physical activity after waking. J Hypertens. 2002;20:865–70.
Egan B, Panis R, Hinderliter A, Schork N, Julius S. Mechanism of increased alpha adrenergic vasoconstriction in human essential hypertension. J Clin Invest. 1987;80:812.
Pierdomenico SD, Pierdomenico AM, Di Tommaso R, Coccina F, Di Carlo S, Porreca E, et al. Morning blood pressure surge, dipping, and risk of coronary events in elderly treated hypertensive patients. Am J Hypertens. 2015;29:39–45.
Sheppard JP, Hodgkinson J, Riley R, Martin U, Bayliss S, McManus RJ. Prognostic significance of the morning blood pressure surge in clinical practice: a systematic review. Am J Hypertens. 2014;28:30–41.
Kario K, Shimada K, Pickering TG. Clinical implication of morning blood pressure surge in hypertension. J Cardiovasc Pharmacol. 2003;42:S87–S91.
Kario K. Essential manual of 24h blood pressure management: from morning to nocturnal hypertension. John Wiley & Sons; 2015. p. 70.
Kario K, Pickering TG, Umeda Y, Hoshide S, Hoshide Y, Morinari M, et al. Morning surge in blood pressure as a predictor of silent and clinical cerebrovascular disease in elderly hypertensives a prospective study. Circulation. 2003;107:1401–6.
Metoki H, Ohkubo T, Kikuya M, Asayama K, Obara T, Hashimoto J, et al. Prognostic significance for stroke of a morning pressor surge and a nocturnal blood pressure decline: the Ohasama Study. Hypertension. 2006;47:149–54.
Verdecchia P, Angeli F, Mazzotta G, Garofoli M, Ramundo E, Gentile G, et al. Day-night dip and early-morning surge in blood pressure in hypertension prognostic implications. Hypertension. 2012;60:34–42.
Rizzoni D, Porteri E, Platto C, Rizzardi N, De Ciuceis C, Boari GE, et al. Morning rise of blood pressure and subcutaneous small resistance artery structure. J Hypertens. 2007;25:1698–703.
Haas DC, Gerber LM, Shimbo D, Warren K, Pickering TG, Schwartz JE. A comparison of morning blood pressure surge in African Americans and whites. J Clin Hypertens. 2005;7:205–11.
Sun N, Xi Y, Jing S, Lu X. Morning blood pressure surge varies with age and gender in hypertensive individuals. Int J Cardiol. 2009;135:272–3.
Patro BK, Jeyashree K, Gupta PK. Kuppuswamy’s socioeconomic status scale 2010—the need for periodic revision. Indian J Pediatr. 2012;79:395–6.
O’brien E, Asmar R, Beilin L, Imai Y, Mancia G, Mengden T, et al. Practice guidelines of the European Society of Hypertension for clinic, ambulatory and self blood pressure measurement. J Hypertens. 2005;23:697–701.
Kario K, Bhatt DL, Brar S, Cohen SA, Fahy M, Bakris GL. Effect of catheter-based renal denervation on morning and nocturnal blood pressure novelty and significance. Hypertension. 2015;66:1130–7.
Li Y, Thijs L, Hansen TW, Kikuya M, Boggia J, Richart T, et al. Prognostic value of the morning blood pressure surge in 5645 subjects from 8 populations. Hypertension. 2010;55:1040–8.
Kario K. Evidence and perspectives on the 24-hour management of hypertension: hemodynamic biomarker-initiated ‘anticipation medicine’for zero cardiovascular event. Prog Cardiovasc Dis. 2016;59:262–81.
Kario K. Perfect 24-h management of hypertension: clinical relevance and perspectives. J Hum Hypertens. 2016;31:231–43.
Organization WH. Regional Consultation on Strategies to Reduce Salt Intake, Singapore, 2–3 June 2010: report. Manila: WHO Regional Office for the Western Pacific. 2010.
Lockette W, Otsuka Y, Carretero O. The loss of endothelium-dependent vascular relaxation in hypertension. Hypertension. 1986;8:II61–6.
Matsuda H, Kuon E, Holtz J, Busse R. Endothelium-mediated dilations contribute to the polarity of the arterial wall in vasomotion induced by [alpha] 2-adrenergic agonists. J Cardiovasc Pharmacol. 1985;7:680–8.
Cocks T, Angus J. Endothelium-dependent relaxation of coronary arteries by noradrenaline and serotonin. Nature. 1983;305:627–30.
Godfraind T, Egleme C, Al Osachie I. Role of endothelium in the contractile response of rat aorta to α-adrenoceptor agonists. Clin Sci. 1985;68:65s–71s.
Sherwood A, Routledge FS, Wohlgemuth WK, Hinderliter AL, Kuhn CM, Blumenthal JA. Blood pressure dipping: ethnicity, sleep quality, and sympathetic nervous system activity. Am J Hypertens. 2011;24:982–8.
Pickering TG, Shimbo D, Haas D. Ambulatory blood-pressure monitoring. N Engl J Med. 2006;354:2368–74.
Ohkubo T, Hozawa A, Yamaguchi J, Kikuya M, Ohmori K, Michimata M, et al. Prognostic significance of the nocturnal decline in blood pressure in individuals with and without high 24-h blood pressure: the Ohasama study. J Hypertens. 2002;20:2183–9.
Israel S, Israel A, Ben-Dov IZ, Bursztyn M. The morning blood pressure surge and all-cause mortality in patients referred for ambulatory blood pressure monitoring. Am J Hypertens. 2011;24:796–801.
Pierdomenico SD, Pierdomenico AM, Coccina F, Lapenna D, Porreca E. Circadian blood pressure changes and cardiovascular risk in elderly-treated hypertensive patients. Hypertens Res. 2016;39:805–11.
Hoshide S, Kario K, De La Sierra A, Bilo G, Schillaci G, Banegas JR, et al. Ethnic differences in the degree of morning blood pressure surge and in its determinants between Japanese and European hypertensive subjects novelty and significance: data from the ARTEMIS Study. Hypertension. 2015;66:750–60.
Elsurer R, Afsar B. Morning blood pressure surge is associated with serum gamma-glutamyltransferase activity in essential hypertensive patients. J Hum Hypertens. 2015;29:331–6.
White WB. Importance of blood pressure control over a 24-hour period. J Manag Care Pharm. 2007;13(Supp B):34–9.
Wang X, Zhu H, Dong Y, Treiber FA, Snieder H. Effects of angiotensinogen and angiotensin II type I receptor genes on blood pressure and left ventricular mass trajectories in multiethnic youth. Twin Res Hum Genet. 2006;9:393–402.
Ellis JA, Wong ZY, Stebbing M, Harrap SB. Sex, genes and blood pressure. Clin Exp Pharmacol Physiol. 2001;28:1053–5.
Schutte AE, Huisman HW, Van Rooyen JM, De Ridder JH, Malan NT. Associations between arterial compliance and anthropometry of children from four ethnic groups in South Africa: the THUSA BANA Study. Blood Press. 2003;12:97–103.
Kawano Y, Horio T, Matayoshi T, Kamide K. Masked hypertension: subtypes and target organ damage. Clin Exp Hypertens. 2008;30:289–96.
Roseman C, Truedsson L, Kapetanovic MC. The effect of smoking and alcohol consumption on markers of systemic inflammation, immunoglobulin levels and immune response following pneumococcal vaccination in patients with arthritis. Arthritis Res Ther. 2012;14:R170.
Van Rooyen J, Poglitsch M, Huisman H, Mels C, Kruger R, Malan L, et al. Quantification of systemic renin-angiotensin system peptides of hypertensive black and white African men established from the RAS-Fingerprint®. J Renin Angiotensin Aldosterone Syst. 2016;17. 1470320316669880.
Acknowledgements
The authors are grateful towards all individuals participating voluntarily in the study. The dedication of the support and research staff as well as students at the Hypertension Research and Training Clinic at the North-West University are also duly acknowledged.
Funding
The African-PREDICT study is an ongoing study financially supported by the South African Medical Research Council (SAMRC) with funds from National Treasury under its Economic Competitiveness and Support Package; the South African Research Chairs Initiative (SARChI) of the Department of Science and Technology and National Research Foundation (NRF) of South Africa; the Strategic Health Innovation Partnerships (SHIP) Unit of the SAMRC with funds received from the South African National Department of Health, GlaxoSmithKline R&D, the UK Medical Research Council and with funds from the UK Government’s Newton Fund; as well as corporate social investment grants from Pfizer (South Africa), Boehringer-Ingelheim (South Africa), Novartis (South Africa), the Medi Clinic Hospital Group (South Africa) and in kind contributions of Roche Diagnostics (South Africa). Any opinion, findingsand conclusions or recommendations expressed in this material arethose of the authors and therefore the NRF does not accept any liabilityin regard thereto.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Electronic supplementary material
Rights and permissions
About this article
Cite this article
Mokwatsi, G.G., Schutte, A.E., Mels, C.M.C. et al. Morning blood pressure surge in young black and white adults: The African-PREDICT Study. J Hum Hypertens 33, 22–33 (2019). https://doi.org/10.1038/s41371-018-0089-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41371-018-0089-3
This article is cited by
-
Retinal microvasculature and masked hypertension in young adults: the African-PREDICT study
Hypertension Research (2020)
-
Disturbed Sleep as a Mechanism of Race Differences in Nocturnal Blood Pressure Non-Dipping
Current Hypertension Reports (2019)