Abstract
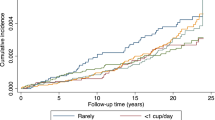
Some debates exist regarding the association of coffee consumption with hypertension risk. We performed a meta-analysis including dose–response analysis aimed to derive a more quantitatively precise estimation of this association. PubMed and Embase were searched for cohort studies published up to 18 July 2017. Fixed-effects generalized least-squares regression models were used to assess the quantitative association between coffee consumption and hypertension risk across studies. Restricted cubic spline was used to model the dose–response association. We identified eight articles (10 studies) investigating the risk of hypertension with the level of coffee consumption, including 243,869 individuals and 58,094 incident cases of hypertension. We found no evidence of a nonlinear dose–response association of coffee consumption and hypertension (P nonlinearity = 0.243). The risk of hypertension was reduced by 2% (relative risk (RR) = 0.98, 95% confidence interval (CI) 0.98–0.99) with each one cup/day increment of coffee consumption. With the linear cubic spline model, the RRs of hypertension risk were 0.97 (95% CI 0.95–0.99), 0.95 (95% CI 0.91–0.99), 0.92 (95% CI 0.87–0.98), and 0.90 (95% CI 0.83–0.97) for 2, 4, 6, and 8 cups/day, respectively, compared with individuals with no coffee intakes. This meta-analysis provides quantitative evidence that consumption of coffee was inversely associated with the risk of hypertension in a dose–response manner.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 digital issues and online access to articles
$119.00 per year
only $9.92 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
World Health Organization. A Global Brief on Hypertension: Silent Killer, Global Public Health Crisis: World Health Day 2013; 2013.
Cao X. A call for global research on non-communicable diseases. Lancet. 2015;385:e5–6.
Benjamin EJ, Blaha MJ, Chiuve SE, Cushman M, Das SR, Deo R, et al. Heart disease and stroke statistics-2017 update: a report from the American heart association. Circulation. 2017;135:e146–603.
Murray CJ, Lopez AD. Measuring the global burden of disease. N Engl J Med. 2013;369:448–57.
Kearney PM, Whelton M, Reynolds K, Muntner P, Whelton PK, He J. Global burden of hypertension: analysis of worldwide data. Lancet. 2005;365:217–23.
Butt MS, Sultan MT. Coffee and its consumption: benefits and risks. Crit Rev Food Sci Nutr. 2011;51:363–73.
Horst K, Robinson WD, Jenkins WL, Bao DL. The effect of caffeine, coffee and decaffeinated coffee upon blood pressure, pulse rate and certain motor reactions of normal young men. J Pharmacol Exp Ther. 1935;53:307–21.
Simon NM. Coffee and hypertension. N Engl J Med. 1978;298:1092.
Klag MJ, Wang NY, Meoni LA, Brancati FL, Cooper LA, Liang KY, et al. Coffee intake and risk of hypertension: the Johns Hopkins precursors study. Arch Intern Med. 2002;162:657–62.
Winkelmayer WC, Stampfer MJ, Willett WC, Curhan GC. Habitual caffeine intake and the risk of hypertension in women. JAMA. 2005;294:2330–5.
Uiterwaal CS, Verschuren WM, Bueno-de-Mesquita HB, Ocke M, Geleijnse JM, Boshuizen HC, et al. Coffee intake and incidence of hypertension. Am J Clin Nutr. 2007;85:718–23.
Palatini P, Dorigatti F, Santonastaso M, Cozzio S, Biasion T, Garavelli G, et al. Association between coffee consumption and risk of hypertension. Ann Med. 2007;39:545–53.
Hu G, Jousilahti P, Nissinen A, Bidel S, Antikainen R, Tuomilehto J. Coffee consumption and the incidence of antihypertensive drug treatment in Finnish men and women. Am J Clin Nutr. 2007;86:457–64.
Grosso G, Stepaniak U, Polak M, Micek A, Topor-Madry R, Stefler D, et al. Coffee consumption and risk of hypertension in the Polish arm of the HAPIEE cohort study. Eur J Clin Nutr. 2016;70:109–15.
Rhee JJ, Qin F, Hedlin HK, Chang TI, Bird CE, Zaslavsky O, et al. Coffee and caffeine consumption and the risk of hypertension in postmenopausal women. Am J Clin Nutr. 2016;103:210–07.
Chei CL, Loh JK, Soh A, Yuan JM, Koh WP. Coffee, tea, caffeine, and risk of hypertension: the Singapore Chinese health study. Eur J Nutr. 2017; e-pub ahead of print 1 March 2017; https://doi.org/10.1007/s00394-017-1412-4.
Steffen M, Kuhle C, Hensrud D, Erwin PJ, Murad MH. The effect of coffee consumption on blood pressure and the development of hypertension: a systematic review and meta-analysis. J Hypertens. 2012;30:2245–54.
Zhang Z, Hu G, Caballero B, Appel L, Chen L. Habitual coffee consumption and risk of hypertension: a systematic review and meta-analysis of prospective observational studies. Am J Clin Nutr. 2011;93:1212–9.
Geleijnse JM. Habitual coffee consumption and blood pressure: an epidemiological perspective. Vasc Health Risk Manage. 2008;4:963–70.
Stroup DF, Berlin JA, Morton SC, Olkin I, Williamson GD, Rennie D, et al. Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis of observational studies in epidemiology (moose) group. JAMA. 2000;283:2008–12.
Bekkering GE, Harris RJ, Thomas S, Mayer AMB, Beynon R, Ness AR, et al. How much of the data published in observational studies of the association between diet and prostate or bladder cancer is usable for meta-analysis. Am J Epidemiol. 2008;167:1017–26.
Wells GA, Shea BJ, O’Connell D, Peterson J, Welch V, Losos M, et al. The Newcastle–Ottawa Scale (NOS) for assessing the quality of non-randomized studies in meta-analysis. Appl Eng Agric. 2014;18:727–34.
Orsini N, Li R, Wolk A, Khudyakov P, Spiegelman D. Meta-analysis for linear and nonlinear dose-response relations: examples, an evaluation of approximations, and software. Am J Epidemiol. 2012;175:66–73.
Mantel N, Haenszel W. Statistical aspects of the analysis of data from retrospective studies of disease. J Natl Cancer Inst. 1959;22:719–48.
Bagnardi V, Zambon A, Quatto P, Corrao G. Flexible meta-regression functions for modeling aggregate dose-response data, with an application to alcohol and mortality. Am J Epidemiol. 2004;159:1077–86.
Orsini N, Bellocco R, Greenland S. Generalized least squares for trend estimation of summarized dose–response data. Stata J. 2006;6:40–57.
Greenland S. Dose-response and trend analysis in epidemiology: alternatives to categorical analysis. Epidemiology. 1995;6:356–65.
Hartemink N, Boshuizen HC, Nagelkerke NJD, Jacobs MAM, Houwelingen HCV. Combining risk estimates from observational studies with different exposure cutpoints: a meta-analysis on body mass index and diabetes Type 2. Am J Epidemiol. 2006;163:1042–52.
Higgins JPT, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. Br Med J. 2003;327:557–60.
Begg CB, Mazumdar M. Operating characteristics of a rank correlation test for publication bias. Biometrics. 1994;50:1088–101.
Godos J, Pluchinotta FR, Marventano S, Buscemi S, Li VG, Galvano F, et al. Coffee components and cardiovascular risk: beneficial and detrimental effects. Int J Food Sci Nutr. 2014;65:1–12.
Higdon JV, Frei B. Coffee and health: a review of recent human research. Crit Rev Food Sci Nutr. 2006;46:101–23.
Ding M, Bhupathiraju SN, Chen M, van Dam RM, Hu FB. Caffeinated and decaffeinated coffee consumption and risk of type 2 diabetes: a systematic review and a dose-response meta-analysis. Diabetes Care. 2014;37:569–86.
Kang YS. Obesity associated hypertension: new insights into mechanism. Electrolyte Blood Press. 2013;11:46–52.
Guessous I, Eap CB, Bochud M. Blood pressure in relation to coffee and caffeine consumption. Curr Hypertens Rep. 2014;16:468.
Palatini P, Dorigatti F, Santonastaso M, Cozzio S, Biasion T, Garavelli G, et al. Association between coffee consumption and risk of hypertension. Ann Med. 2007;39:545–53.
Narkiewicz K, Maraglino G, Biasion T, Rossi G, Sanzuol F, Palatini P. Interactive effect of cigarettes and coffee on daytime systolic blood pressure in patients with mild essential hypertension. HARVEST Study Group (Italy). Hypertension Ambulatory Recording VEnetia STudy. J Hypertens. 1995;13:965–70.
Cornelis MC, El-Sohemy A, Kabagambe EK, Campos H. Coffee,CYP1A2 genotype,and risk of myocardial infarction. JAMA. 2006;295:1135–41.
Platt DE, Ghassibesabbagh M, Salameh P, Salloum AK, Haber M, Mouzaya F, et al. Caffeine impact on metabolic syndrome components is modulated by a CYP1A2 Variant. Ann Nutr Metab. 2015;68:1–11.
Palatini P, Ceolotto G, Ragazzo F, Dorigatti F, Saladini F, Papparella I, et al. CYP1A2 genotype modifies the association between coffee intake and the risk of hypertension. J Hypertens. 2009;27:1594–601.
Ferraroni M, Tavani A, Decarli A, Franceschi S, Parpinel M, Negri E, et al. Reproducibility and validity of coffee and tea consumption in Italy. Eur J Clin Nutr. 2004;58:674–80.
Salvini S, Hunter DJ, Sampson L, Stampfer MJ, Colditz GA, Rosner B, et al. Food-based validation of a dietary questionnaire: The effects of week-to-week variation in food consumption. Int J Epidemiol. 1989;18:858–67.
Noordzij M, Uiterwaal CS, Arends LR, Kok FJ, Grobbee DE, Geleijnse JM. Blood pressure response to chronic intake of coffee and caffeine: a meta-analysis of randomized controlled trials. J Hypertens. 2005;23:921–8.
Acknowledgments
This research was supported by the National Social Science Foundation of China (Grant number 15BSH043). This research was supported by the National Social Science Foundation of China (Grant number 15BSH043). The National Social Science Foundation of China had no role in the design/conduct of the study, collection/analysis interpretation of the data, and preparation/review approval of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing financial interest.
Electronic supplementary material
Rights and permissions
About this article
Cite this article
Xie, C., Cui, L., Zhu, J. et al. Coffee consumption and risk of hypertension: a systematic review and dose–response meta-analysis of cohort studies. J Hum Hypertens 32, 83–93 (2018). https://doi.org/10.1038/s41371-017-0007-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41371-017-0007-0
This article is cited by
-
Coffee intake and hypertension in Korean adults: results from KNHANES 2012–2016
Clinical Hypertension (2023)
-
Implementation of non-pharmacological interventions for the treatment of hypertension in primary care: a narrative review of effectiveness, cost-effectiveness, barriers, and facilitators
BMC Primary Care (2022)
-
Effects of supplementation with main coffee components including caffeine and/or chlorogenic acid on hepatic, metabolic, and inflammatory indices in patients with non-alcoholic fatty liver disease and type 2 diabetes: a randomized, double-blind, placebo-controlled, clinical trial
Nutrition Journal (2021)
-
Coffee and Arterial Hypertension
Current Hypertension Reports (2021)
-
Caffeine and caffeine metabolites in relation to hypertension in U.S. adults
European Journal of Clinical Nutrition (2020)