Abstract
Background
Variations in dietary intake and environmental exposure patterns of essential and non-essential trace metals influence many aspects of human health throughout the life span.
Objective
To examine the relationship between urine profiles of essential and non-essential metals in mother-offspring pairs and their association with early dysglycemia.
Methods
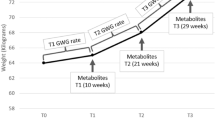
Herein, we report findings from an ancillary study to the international Hyperglycemia and Adverse Pregnancy Outcome Follow-Up Study (HAPO-FUS) that examined urinary essential and non-essential metal profiles from mothers and offspring ages 10–14 years (1012 mothers, 1013 offspring, 968 matched pairs) from 10 international sites.
Results
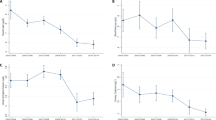
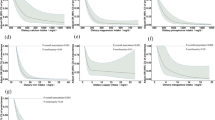
Our analysis demonstrated a diverse exposure pattern across participating sites. In multiple regression modelling, a positive association between markers of early dysglycemia and urinary zinc was found in both mothers and offspring after adjustment for common risk factors for diabetes. The analysis showed weaker, positive, and negative associations of the 2-h glucose value with urinary selenium and arsenic respectively. A positive association between 2-h glucose values and cadmium was found only in mothers in the fully adjusted model when participants with established diabetes were excluded. There was a high degree of concordance between mother and offspring urinary metal profiles. Mother-to-offspring urinary metal ratios were unique for each metal, providing insights into changes in their homeostasis across the lifespan.
Significance
Urinary levels of essential and non-essential metals are closely correlated between mothers and their offspring in an international cohort. Urinary levels of zinc, selenium, arsenic, and cadmium showed varying degrees of association with early dysglycemia in a comparatively healthy cohort with a low rate of preexisting diabetes.
Impact statement
Our data provides novel evidence for a strong correlation between mother and offspring urinary metal patterns with a unique mother-to-offspring ratio for each metal. The study also provides new evidence for a strong positive association between early dysglycemia and urinary zinc, both in mothers and offspring. Weaker positive associations with urinary selenium and cadmium and negative associations with arsenic were also found. The low rate of preexisting diabetes in this population provides the unique advantage of minimizing the confounding effect of preexisting, diabetes related renal changes that would alter the relationship between dysglycemia and renal metal excretion.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 6 print issues and online access
$259.00 per year
only $43.17 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
Data availability
Data will be made available upon reasonable request.
References
Klaassen CD, Watkins JB, Casarett LJ Casarett & Doull’s essentials of toxicology. McGraw-Hill Medical: New York, 2010.
Nordberg G, Fowler BA, Nordberg M, Handbook on the Toxicology of Metals. 2014.
Attar T. A mini-review on importance and role of trace elements in the human organism. Chem Rev Lett. 2020;3:117–30.
Bogden JD, Klevay LM, Clinical Nutrition of the Essential Trace Elements and Minerals. Springer, 2000.
Nuttall JR, Supasai S, Kha J, Vaeth BM, Mackenzie GG, Adamo AM, et al. Gestational marginal zinc deficiency impaired fetal neural progenitor cell proliferation by disrupting the ERK1/2 signaling pathway. J Nutr Biochem. 2015;26:1116–23.
Aimo L, Mackenzie GG, Keenan AH, Oteiza PI. Gestational zinc deficiency affects the regulation of transcription factors AP-1, NF-kappaB and NFAT in fetal brain. J Nutr Biochem. 2010;21:1069–75.
Modzelewska D, Sole-Navais P, Brantsaeter AL, Flatley C, Elfvin A, Meltzer HM, et al. Maternal dietary selenium intake during pregnancy and neonatal outcomes in the Norwegian mother, father, and child cohort study. Nutrients. 2021;13:1239.
Mendel RR, Kruse T. Cell biology of molybdenum in plants and humans. Biochim Biophys Acta. 2012;1823:1568–79.
Bellinger DC. Lead neurotoxicity and socioeconomic status: conceptual and analytical issues. Neurotoxicology. 2008;29:828–32.
Liu S, Guo X, Wu B, Yu H, Zhang X, Li M. Arsenic induces diabetic effects through beta-cell dysfunction and increased gluconeogenesis in mice. Sci Rep. 2014;4:6894.
Maull EA, Ahsan H, Edwards J, Longnecker MP, Navas-Acien A, Pi J, et al. Evaluation of the association between arsenic and diabetes: a National Toxicology Program workshop review. Environ Health Perspect. 2012;120:1658–70.
Martin E, Gonzalez-Horta C, Rager J, Bailey KA, Sanchez-Ramirez B, Ballinas-Casarrubias L, et al. Metabolomic characteristics of arsenic-associated diabetes in a prospective cohort in Chihuahua, Mexico. Toxicol Sci. 2015; https://doi.org/10.1093/toxsci/kfu318.
Brauner EV, Nordsborg RB, Andersen ZJ, Tjonneland A, Loft S, Raaschou-Nielsen O. Long-term exposure to low-level arsenic in drinking water and diabetes incidence: a prospective study of the diet, cancer and health cohort. Environ Health Perspect. 2014;122:1059–65.
Davila-Esqueda ME, Morales JM, Jimenez-Capdeville ME, De la Cruz E, Falcon-Escobedo R, Chi-Ahumada E, et al. Low-level subchronic arsenic exposure from prenatal developmental stages to adult life results in an impaired glucose homeostasis. Exp Clin Endocrinol Diabetes: Off J, Ger Soc Endocrinol Ger Diabetes Assoc. 2011;119:613–7.
James KA, Byers T, Hokanson JE, Meliker JR, Zerbe GO, Marshall JA. Association between lifetime exposure to inorganic arsenic in drinking water and coronary heart disease in Colorado residents. Environ Health Perspect. 2015;123:128–34.
Saintilnord WN, Tenlep SYN, Preston JD, Duregon E, DeRouchey JE, Unrine JM, et al. Chronic exposure to cadmium induces differential methylation in mice spermatozoa. Toxicol Sci. 2021;180:262–76.
Buchet JP, Lauwerys R, Roels H, Bernard A, Bruaux P, Claeys F, et al. Renal effects of cadmium body burden of the general population. Lancet. 1990;336:699–702.
Buha A, Dukic-Cosic D, Curcic M, Bulat Z, Antonijevic B, Moulis JM, et al. Emerging links between cadmium exposure and insulin resistance: human, animal, and cell study data. Toxics. 2020;8:63.
Benoff S, Hauser R, Marmar JL, Hurley IR, Napolitano B, Centola GM. Cadmium concentrations in blood and seminal plasma: correlations with sperm number and motility in three male populations (infertility patients, artificial insemination donors, and unselected volunteers). Mol Med. 2009;15:248–62.
Wallia A, Allen NB, Badon S, El Muayed M. Association between urinary cadmium levels and prediabetes in the NHANES 2005–2010 population. Int J Hyg Environ Health. 2014;37:2960–5.
Filippini T, Wise LA, Vinceti M. Cadmium exposure and risk of diabetes and prediabetes: A systematic review and dose-response meta-analysis. Environ Int. 2022;158:106920.
Cardoso BR, Braat S, Graham RM. Selenium status is associated with insulin resistance markers in adults: Findings From the 2013 to 2018 National Health and Nutrition Examination Survey (NHANES). Front Nutr. 2021;8:696024.
Kohler LN, Foote J, Kelley CP, Florea A, Shelly C, Chow HS, et al. Selenium and Type 2 Diabetes: Systematic Review. Nutrients. 2018;10:1924.
Lu CW, Chang HH, Yang KC, Kuo CS, Lee LT, Huang KC. High serum selenium levels are associated with increased risk for diabetes mellitus independent of central obesity and insulin resistance. BMJ Open Diabetes Res Care. 2016;4:e000253.
Scholtens DM, Kuang A, Lowe LP, Hamilton J, Lawrence JM, Lebenthal Y, et al. Hyperglycemia and Adverse Pregnancy Outcome Follow-up Study (HAPO FUS): Maternal glycemia and childhood glucose metabolism. Diabetes Care. 2019;42:381–92.
el-Yazigi A, Hannan N, Raines DA. Effect of diabetic state and related disorders on the urinary excretion of magnesium and zinc in patients. Diabetes Res. 1993;22:67–75.
Garg VK, Gupta R, Goyal RK. Hypozincemia in diabetes mellitus. J Assoc Physicians India. 1994;42:720–1.
Basaki M, Saeb M, Nazifi S, Shamsaei HA. Zinc, copper, iron, and chromium concentrations in young patients with type 2 diabetes mellitus. Biol Trace Elem Res. 2012;148:161–4.
Jansen J, Rosenkranz E, Overbeck S, Warmuth S, Mocchegiani E, Giacconi R, et al. Disturbed zinc homeostasis in diabetic patients by in vitro and in vivo analysis of insulinomimetic activity of zinc. J Nutr Biochem. 2012;23:1458–66.
Schwartz GG, Il’yasova D, Ivanova A. Urinary cadmium, impaired fasting glucose, and diabetes in the NHANES III. Diabetes Care. 2003;26:468–70.
Afridi HI, Kazi TG, Kazi N, Jamali MK, Arain MB, Jalbani N, et al. Evaluation of status of toxic metals in biological samples of diabetes mellitus patients. Diabetes Res Clin Pr. 2008;80:280–8.
Swaddiwudhipong W, Limpatanachote P, Mahasakpan P, Krintratun S, Punta B, Funkhiew T. Progress in cadmium-related health effects in persons with high environmental exposure in northwestern Thailand: a five-year follow-up. Environ Res. 2012;112:194–8.
Wei J, Zeng C, Gong QY, Yang HB, Li XX, Lei GH, et al. The association between dietary selenium intake and diabetes: a cross-sectional study among middle-aged and older adults. Nutr J. 2015;14:18.
Fu J, Woods CG, Yehuda-Shnaidman E, Zhang Q, Wong V, Collins S, et al. Low-level arsenic impairs glucose-stimulated insulin secretion in pancreatic beta cells: involvement of cellular adaptive response to oxidative stress. Environ Health Perspect. 2010;118:864–70.
Sung TC, Huang JW, Guo HR. Association between arsenic exposure and diabetes: a meta-analysis. Biomed Res Int. 2015;2015:368087.
Lowe WL Jr., Scholtens DM, Kuang A, Linder B, Lawrence JM, Lebenthal Y, et al. Hyperglycemia and Adverse Pregnancy Outcome Follow-up Study (HAPO FUS): Maternal gestational diabetes mellitus and childhood glucose metabolism. Diabetes Care. 2019;42:372–80.
Lowe WL Jr., Scholtens DM, Lowe LP, Kuang A, Nodzenski M, Talbot O, et al. Association of gestational diabetes with maternal disorders of glucose metabolism and childhood adiposity. JAMA: J Am Med Assoc. 2018;320:1005–16.
Group HSCR, Metzger BE, Lowe LP, Dyer AR, Trimble ER, Chaovarindr U, et al. Hyperglycemia and adverse pregnancy outcomes. N. Engl J Med. 2008;358:1991–2002.
CDC. National Health and Nutrition Examination Survey 1999–2012 Survey Content Brochure. In, 2012.
Wong WP, Allen NB, Meyers MS, Link EO, Zhang X, MacRenaris KW, et al. Exploring the association between demographics, SLC30A8 genotype, and human islet content of Zinc, Cadmium, Copper, Iron, Manganese and Nickel. Sci Rep. 2017;7:473.
Peake M, Whiting M. Measurement of serum creatinine-current status and future goals. Clin Biochem Rev. 2006;27:173–84.
Barr DB, Wilder LC, Caudill SP, Gonzalez AJ, Needham LL, Pirkle JL. Urinary creatinine concentrations in the U.S. population: implications for urinary biologic monitoring measurements. Environ Health Perspect. 2005;113:192–200.
Chabosseau P, Rutter GA. Zinc and diabetes. Arch Biochem Biophys. 2016;611:79–85.
Fernandez-Cao JC, Warthon-Medina M, Victoria HM, Arija V, Doepking C, Serra-Majem L, et al. Zinc intake and status and risk of type 2 diabetes mellitus: a systematic review and meta-analysis. Nutrients. 2019;11:1027.
Lau AL, Failla ML. Urinary excretion of zinc, copper and iron in the streptozotocin-diabetic rat. J Nutr. 1984;114:224–33.
Stenvinkel P, Bolinder J, Alvestrand A. Effects of insulin on renal haemodynamics and the proximal and distal tubular sodium handling in healthy subjects. Diabetologia. 1992;35:1042–8.
Raz I, Havivi E. Influence of chronic diabetes on tissue and blood cells status of zinc, copper, and chromium in the rat. Diabetes Res. 1988;7:19–23.
Ward DT, Hamilton K, Burnand R, Smith CP, Tomlinson DR, Riccardi D. Altered expression of iron transport proteins in streptozotocin-induced diabetic rat kidney. Biochim Biophys Acta. 2005;1740:79–84.
Kinlaw WB, Levine AS, Morley JE, Silvis SE, McClain CJ. Abnormal zinc metabolism in type II diabetes mellitus. Am J Med. 1983;75:273–7.
In: Global Mercury Assessment 2018. United Nations Environment Program, 2018.
Ezzati M, Lopez AD, Rodgers AA, Murray CJL, Comparative quantification of health risks, volume 1: global and regional burden of disease attributable to selected major risk factors. In. Geneva: World Health Organization, 2004.
Wang X, Mukherjee B, Batterman S, Harlow SD, Park SK. Urinary metals and metal mixtures in midlife women: The Study of Women’s Health Across the Nation (SWAN). Int J Hyg Environ Health. 2019;222:778–89.
OCED Environment Health and Safety Division ED. Considerations for Assessing the Risks of Combined Exposure to Multiple Chemicals, Series on Testing and Assessment No. 296. OECD, 2018.
Garcia-Villarino M, Signes-Pastor AJ, Karagas MR, Riano-Galan I, Rodriguez-Dehli C, Grimalt JO, et al. Exposure to metal mixture and growth indicators at 4-5 years. A study in the INMA-Asturias cohort. Environ Res. 2022;204:112375.
Koszewicz M, Markowska K, Waliszewska-Prosol M, Poreba R, Gac P, Szymanska-Chabowska A, et al. The impact of chronic co-exposure to different heavy metals on small fibers of peripheral nerves. A study of metal industry workers. J Occup Med Toxicol. 2021;16:12.
LeRoith D, Taylor S, Olefsky J. Diabetes Mellitus, A Fundamental and Clinical Text. Philadelphia: Lippincott Williams & Wilkins; 2004.
Noctor E, Crowe C, Carmody LA, Saunders JA, Kirwan B, O’Dea A, et al. Abnormal glucose tolerance post-gestational diabetes mellitus as defined by the International Association of Diabetes and Pregnancy Study Groups criteria. Eur J Endocrinol/Eur Federation Endocr Societies. 2016;175:287–97.
Shan Z, Bao W, Zhang Y, Rong Y, Wang X, Jin Y, et al. Interactions between zinc transporter-8 gene (SLC30A8) and plasma zinc concentrations for impaired glucose regulation and type 2 diabetes. Diabetes. 2014;63:1796–803.
Galvez-Fernandez M, Powers M, Grau-Perez M, Domingo-Relloso A, Lolacono N, Goessler W, et al. Urinary Zinc and Incident Type 2 Diabetes: Prospective Evidence From the Strong Heart Study. Diabetes Care 2022; e-pub ahead of print 2022/09/23; https://doi.org/10.2337/dc22-1152.
Dwivedi OP, Lehtovirta M, Hastoy B, Chandra V, Krentz NAJ, Kleiner S, et al. Loss of ZnT8 function protects against diabetes by enhanced insulin secretion. Nat Genet. 2019;51:1596–606.
Flannick J, Thorleifsson G, Beer NL, Jacobs SB, Grarup N, Burtt NP, et al. Loss-of-function mutations in SLC30A8 protect against type 2 diabetes. Nat Genet. 2014;46:357–63.
Merriman C, Huang Q, Rutter GA, Fu D. Lipid-tuned zinc transport activity of human ZnT8 protein correlates with risk for Type-2 diabetes. J Biol Chem. 2016;291:26950–7.
Beck R, Chandi M, Kanke M, Styblo M, Sethupathy P. Arsenic is more potent than cadmium or manganese in disrupting the INS-1 beta cell microRNA landscape. Arch Toxicol. 2019;93:3099–109.
Li YY, Douillet C, Huang M, Beck R, Sumner SJ, Styblo M. Exposure to inorganic arsenic and its methylated metabolites alters metabolomics profiles in INS-1 832/13 insulinoma cells and isolated pancreatic islets. Arch Toxicol. 2020;94:1955–72.
Huang M, Douillet C, Styblo M. Arsenite and its trivalent methylated metabolites inhibit glucose-stimulated calcium influx and insulin secretion in murine pancreatic islets. Arch Toxicol. 2019;93:2525–33.
Kitchin KT, Wallace K. The role of protein binding of trivalent arsenicals in arsenic carcinogenesis and toxicity. J Inorg Biochem. 2008;102:532–9.
Styblo M, Venkatratnam A, Fry RC, Thomas DJ. Origins, fate, and actions of methylated trivalent metabolites of inorganic arsenic: progress and prospects. Arch Toxicol. 2021;95:1547–72.
Edwards JR, Prozialeck WC. Cadmium, diabetes, and chronic kidney disease. Toxicol Appl Pharm. 2009;238:289–93.
El Muayed M, Raja MR, Zhang X, Macrenaris KW, Bhatt S, Chen X, et al. Accumulation of cadmium in insulin-producing beta cells. Islets. 2012;4:405–16.
Chang KC, Hsu CC, Liu SH, Su CC, Yen CC, Lee MJ, et al. Cadmium induces apoptosis in pancreatic beta-cells through a mitochondria-dependent pathway: the role of oxidative stress-mediated c-Jun N-Terminal Kinase Activation. PLoS One. 2013;8:e54374.
Wong WPS, Wang JC, Meyers MS, Wang NJ, Sponenburg RA, Allen NB, et al. A novel chronic in vivo oral cadmium exposure-washout mouse model for studying cadmium toxicity and complex diabetogenic effects. Toxicol Appl Pharm. 2022;447:116057.
Olsson IM, Bensryd I, Lundh T, Ottosson H, Skerfving S, Oskarsson A. Cadmium in blood and urine-impact of sex, age, dietary intake, iron status, and former smoking-association of renal effects. Environ Health Perspect. 2002;110:1185–90.
Bulat ZP, Dukic-Cosic D, Dokic M, Bulat P, Matovic V. Blood and urine cadmium and bioelements profile in nickel-cadmium battery workers in Serbia. Toxicol Ind Health. 2009;25:129–35.
Link B, Gabrio T, Piechotowski I, Zollner I, Schwenk M. Baden-Wuerttemberg Environmental Health Survey (BW-EHS) from 1996 to 2003: toxic metals in blood and urine of children. Int J Hyg Environ Health. 2007;210:357–71.
Jarup L, Rogenfelt A, Elinder CG, Nogawa K, Kjellstrom T. Biological half-time of cadmium in the blood of workers after cessation of exposure. Scand J Work Environ Health. 1983;9:327–31.
Dakeshita S, Kawai T, Uemura H, Hiyoshi M, Oguma E, Horiguchi H, et al. Gene expression signatures in peripheral blood cells from Japanese women exposed to environmental cadmium. Toxicology. 2009;257:25–32.
Ebert-McNeill A, Clark S, Miller J, Birdsall P, Chandar M, Wu L, et al. Cadmium intake and systemic exposure in postmenopausal women and age-matched men who smoke cigarettes. Toxicol Sci. 2012;130:191–204.
Ruiz P, Mumtaz M, Osterloh J, Fisher J, Fowler BA. Interpreting NHANES biomonitoring data, cadmium. Toxicol Lett. 2010;198:44–48.
Ferraro PM, Costanzi S, Naticchia A, Sturniolo A, Gambaro G. Low-level exposure to cadmium increases the risk of chronic kidney disease: analysis of the NHANES 1999–2006. BMC Public Health. 2010;10:304.
Amzal B, Julin B, Vahter M, Wolk A, Johanson G, Akesson A. Population toxicokinetic modeling of cadmium for health risk assessment. Environ Health Perspect. 2009;117:1293–301.
Maret W, Moulis JM. The bioinorganic chemistry of cadmium in the context of its toxicity. Met Ions Life Sci. 2013;11:1–29.
Elinder CG, Lind B, Kjellstrom T, Linnman L, Friberg L. Cadmium in kidney cortex, liver, and pancreas from Swedish autopsies. Estimation of biological half time in kidney cortex, considering calorie intake and smoking habits. Arch Environ Health. 1976;31:292–302.
Menke A, Guallar E, Cowie CC. Metals in urine and Diabetes in U.S. adults. Diabetes. 2016;65:164–71.
Moon SS. Association of lead, mercury and cadmium with diabetes in the Korean population: the Korea National Health and Nutrition Examination Survey (KNHANES) 2009–2010. Diabet Med: a J Br Diabet Assoc. 2013;30:e143–148.
Nie X, Wang N, Chen Y, Chen C, Han B, Zhu C, et al. Blood cadmium in Chinese adults and its relationships with diabetes and obesity. Environ Sci Pollut Res Int. 2016;23:18714–23.
Liu B, Feng W, Wang J, Li Y, Han X, Hu H, et al. Association of urinary metals levels with type 2 diabetes risk in coke oven workers. Environ Pollut. 2016;210:1–8.
Wong WP, Wallia A, Edwards JR, El Muayed M. Comment on Menke et al. Metals in urine and diabetes in U.S. adults. Diabetes. 2016;65:164–71. Diabetes 2016; 65: e31
Wong WW, Chung SW, Chan BT, Ho YY, Xiao Y. Dietary exposure to inorganic arsenic of the Hong Kong population: results of the first Hong Kong total diet study. Food Chem Toxicol. 2013;51:379–85.
Rayman MP. Selenium and human health. Lancet. 2012;379:1256–68.
Johnson CC, Fordyce FM, Rayman MP. Symposium on ‘Geographical and geological influences on nutrition’: Factors controlling the distribution of selenium in the environment and their impact on health and nutrition. Proc Nutr Soc. 2010;69:119–32.
Murphy J, Cashman KD. Selenium status of Irish adults: evidence of insufficiency. Ir J Med Sci. 2002;171:81–84.
Murphy J, Hannon EM, Kiely M, Flynn A, Cashman KD. Selenium intakes in 18-64-y-old Irish adults. Eur J Clin Nutr. 2002;56:402–8.
Rayman MP, Rayman MP. The argument for increasing selenium intake. Proc Nutr Soc. 2002;61:203–15.
Whitfield JB, Dy V, McQuilty R, Zhu G, Heath AC, Montgomery GW, et al. Genetic effects on toxic and essential elements in humans: arsenic, cadmium, copper, lead, mercury, selenium, and zinc in erythrocytes. Environ Health Perspect. 2010;118:776–82.
da Rocha TJ, Korb C, Schuch JB, Bamberg DP, de Andrade FM, Fiegenbaum M. SLC30A3 and SEP15 gene polymorphisms influence the serum concentrations of zinc and selenium in mature adults. Nutr Res. 2014;34:742–8.
Acknowledgements
ICP-MS metal analysis was performed at Quantitative Bio-elemental Imaging Center, Northwestern University that is supported by NASA Ames Research Center (NNA04CC36G). Data and urine samples used in this ancillary study originated from the Hyperglycemia and Adverse Pregnancy Outcome Follow Up Study (HAPO-FUS). Group Information: The collaborator members of the HAPO Follow-up Study Cooperative Research Group by field center are: Bangkok, Thailand: C. Deerochanawong, T. Tanaphonpoonsuk (Rajavithi Hospital) and S. Binratkaew, U. Chotigeat, W. Manyam (Queen Sirikit National Institute of Child Health); Barbados: M. Forde, A. Greenidge, K. Neblett, P. M. Lashley, D. Walcott (Queen Elizabeth Hospital, School of Clinical Medicine and Research, University of the West Indies); Belfast, Ireland: K. Corry, L. Francis, J. Irwin, A. Langan, D. R. McCance, M. Mousavi (Belfast Health and Social Care Trust) and I. S. Young (Queen’s University); Bellflower, California: J. Gutierrez, J. Jimenez, J. M. Lawrence, D. A. Sacks, H. S. Takhar, E. Tanton (Kaiser Permanente of Southern California); Chicago, Illiniois: W. J. Brickman, J. Howard, J. L. Josefson, L. Miller (Ann and Robert H. Lurie Children’s Hospital and Northwestern University Feinberg School of Medicine); Cleveland, Ohio: J. Bjaloncik, P. M. Catalano, A. Davis, K. Koontz, L. Presley, S. Smith, A. Tyhulski (MetroHealth Medical Center and Case Western Reserve University); Hong Kong, China: A. Li, R. C. Ma, R. Ozaki, W. H. Tam, M. Wong, C. Yuen (Chinese University of Hong Kong and Prince of Wales Hospital); Manchester, England: P. E. Clayton, A. Khan, A. Vyas (Royal Manchester Children’s Hospital, Manchester University Hospitals NHS Foundation Trust, Manchester Academic Healthy Sciences Centre and School of Medical Sciences, Faculty of Biology, Medicine, and Health, University of Manchester) and M. Maresh (St Mary’s Hospital, Manchester University Hospitals NHS Foundation Trust, Manchester Academic Health Sciences Centre); Petah-Tikva, Israel: H. Benzaquen, N. Glickman, A. Hamou, O. Hermon, O. Horesh, Y. Keren, S. Shalitin (Schneider Children’s Medical Center of Israel) and Y. Lebenthal (Jesse Z. and Sara Lea Shafer Institute for Endocrinology and Diabetes, National Center for Childhood Diabetes, Schneider Children’s Medical Center of Israel, Sackler Faculty of Medicine, Tel Aviv University); and Toronto, Ontario, Canada: K. Cordeiro, J. Hamilton, H. Y. Nguyen, S. Steele (Hospital for Sick Children, University of Toronto). Coordinating Center: Northwestern University Feinberg School of Medicine (F. Chen, A. R. Dyer, W. Huang, A. Kuang, M. Jimenez, L. P. Lowe, W. L. Lowe Jr, B. E. Metzger, M. Nodzenski, A. Reisetter, D. Scholtens, O. Talbot, P. Yim). Consultants: D. Dunger, A. Thomas. National Institute of Diabetes and Digestive and Kidney Diseases: M. Horlick, B. Linder, A. Unalp-Arida. Eunice Kennedy Shriver National Institute of Child Health and Human Development: G. Grave.
Funding
The HAPO Follow-up Study was funded by grant 1U01DK094830 from the National Institute of Diabetes and Digestive and Kidney Diseases and the Eunice Kennedy Shriver National Institute of Child Health and Human Development. The HAPO Follow-up Study data were collected and managed using REDCap electronic data capture tools hosted at Northwestern University Feinberg School of Medicine. REDCap is supported at Feinberg School of Medicine by the Northwestern University Clinical and Translational Science Institute. The research reported in this article was supported, in part by grant UL1TR001422 from the National Center for Advancing Translational Sciences, National Institutes of Health. This ancillary study was also partially supported by grants from the National Institutes of Health/National Institute of Environmental Health Sciences (5R01ES027011) awarded to MEM.
Author information
Authors and Affiliations
Contributions
MEM: Conceptualization of the ancillary study, ancillary study administration formal analysis, ancillary study funding acquisition, methodology, resources, supervision, writing original draft, revisions, review & editing. JW: Project administration, data acquisition, data analysis, methodology, project Administration, Resources, Validation, WPW: Project administration, resources, supervision, review & editing. BEM: Conceptualization, methodology, resources, funding acquisition, supervision of the HAPO-FUS underlying the current study, manuscript editing. KBZ: Data analysis, visualization, methodology, manuscript editing. MGG: Data analysis for the revised manuscript, manuscript editing. RAS: Project administration, supervision, manuscript review & editing. MGH: Data curation, investigation, supervision, manuscript review & editing. DMS: Ancillary study data curation, conceptualization of the analysis, supervision of data analysis, resources, manuscript writing, review, and editing. LPL: Administration and conceptualization of the HAPO-FUS study, resources for the current ancillary study, analysis, manuscript review, and editing. WLL Jr.: Conceptualization, methodology, resources, funding acquisition, supervision of the HAPO-FUS underlying the current study, the conceptualization of the current ancillary study, manuscript review, and editing.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
HAPO-FUS was approved by the institutional Review Board (IRB). This ancillary study was classified as exempt from requiring IRB approval by the institutional IRB and approved by the HAPO-FUS steering committee.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
El Muayed, M., Wang, J.C., Wong, W.P. et al. Urinary metal profiles in mother-offspring pairs and their association with early dysglycemia in the International Hyperglycemia and Adverse Pregnancy Outcome Follow Up Study (HAPO-FUS). J Expo Sci Environ Epidemiol 33, 855–864 (2023). https://doi.org/10.1038/s41370-022-00511-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41370-022-00511-z