Abstract
Background
One of the most common pollutants in residences due to gas appliances, NO2 has been shown to increase the risk of asthma attacks after small increases in short term exposure. However, standard environmental sampling methods taken at the regional level overlook chronic intermittent exposure due to lack of temporal and spatial granularity. Further, the EPA and WHO do not currently provide exposure recommendations to at-risk populations.
Aims
A pilot study with pediatric asthma patients was conducted to investigate potential deployment challenges as well as benefits of home-based NO2 sensors and, when combined with a subject’s hospital records and self-reported symptoms, the richness of data available for larger-scale epidemiological studies.
Methods
We developed a compact personal NO2 sensor with one minute temporal resolution and sensitivity down to 15 ppb to monitor exposure levels in the home. Patient hospital records were collected along with self-reported symptom diaries, and two example hypotheses were created to further demonstrate how data of this detail may enable study of the impact of NO2 in this sensitive population.
Results
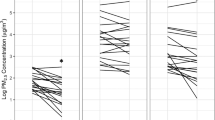
17 patients (55%) had at least 1 h each day with average NO2 exposure >21 ppb. Frequency of acute NO2 exposure >21 ppb was higher in the group with gas stoves (U = 27, p ≤ 0.001), and showed a positive correlation (rs = 0.662, p = 0.037, 95% CI 0.36–0.84) with hospital admissions.
Significance
Similar studies are needed to evaluate the true impact of NO2 in the home environment on at-risk populations, and to provide further data to regulatory bodies when developing updated recommendations.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 6 print issues and online access
$259.00 per year
only $43.17 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout





Similar content being viewed by others
References
Masoli M, Fabian D, Hold S, Beasley R. The global burden of asthma: executive summary of the GINA Dissemination Committee Report. Allergy. 2004;59:469–78.
Akinbami LJ, Moorman JE, Liu X. Asthma Prevalence, Health Care Use, and Mortality: United States, 2005-2009. CDC Natl Health Stat Rep. 2011;32:1–15.
Ivanova JI, Bergman R, Birnbaum HG, Colice GL, Silverman RA, McLaurin K. Effect of asthma exacerbations on health care costs among asthmatic patients with moderate and severe persistent asthma. J Allergy Clin Immunol. 2012;129:1229–35.
Loyo-Berrios NI, Irizarry R, Hennessey JG, Tao XG, Metanoski G. Air Pollution Sources and Childhood Asthma Attacks in Cutano, Puerto Rico. Am J Epidemiol. 2007;165:927–35.
Subbarao P, Mandhane PJ, Sears MR. Asthma: epidemiology, etiology and risk factors. CMAJ. 2009;181:E181–E190.
Barnett SBL, Nurmagambetov TA. Costs of asthma in the United States: 2002-2007. J Allergy Clin Immunol. 2011;127:145–52.
Ross K, Chmiel JF, Ferkol T. The impact of the clean air act. J Pediatrics. 2012;161:781–6.
Schwartz J. Air pollution and children’s health. Pediatrics 2004;113:1037–43.
Dietert RR,ERA,CD,HM,HSD, Jarabek AM, Landreth K, Peden DB, Pinkerton K, Smialowicz RJ, et al. Workshop to identify critical windows of exposure for children’s health: immune and respiratory systems work group summary. Environ Health Perspect. 2000;108:483–90.
Castellsague J, Sunyer J, Saez M, Anto JM. Short-term association between air pollution and emergency room visits for asthma in Barcelona. Thorax 1995;50:1051–6.
Norris G, YoungPong SN, Koenig JQ, Larson TV, Sheppard L, Stout JW. An Association between Fine Particles and Asthma Emergency Department Visits for Children in Seattle. Environ Health Perspect. 1999;107:489–93.
Schouten JP, Vonk JM, de Graaf A. Short term effects of air pollution on emergency hospital admissions for respiratory disease: results of the APHEA project in two major cities in The Netherlands, 1977-89. J Epidemiol Community Health 1996;50:s22–s29.
Burnett RT, Dales RE, Raizenne ME, Krewski D, Summers PW, Roberts GR, et al. Effects of low ambient levels of ozone and sulfates on the frequency of respiratory admissions to Ontario hospitals. Environ Res. 1994;65:172–94.
Schwartz J, Slater D, Larson TV, Pierson WE, Koenig JO. Particulate air pollution and hospital emergency room. Am Rev Respir Dis. 1993;147:826–31.
Slaughter JC, Kim E, Sheppard L, Sullivan JH, Larson TV, Claiborn C. Association between particulate matter and emergency room visits, hospital admissions and mortality in Spokane, Washington. J Exposure Sci Environ Epidemiol. 2005;15:153.
Rumchev K, Spickett J, Bulsara M, Phillips M, Stick S. Association of domestic exposure to volatile organic compounds with asthma in young children. Thorax 2004;59:746–51.
Rodrigo M, Morell F, Helm RM, Swanson M, Greife A, Anto JM, et al. Identification and partial characterization of the soybean-dust allergens involved in the Barcelona asthma epidemic. J Allergy Clin Immunol. 1990;85:778–84.
English P, Neutra R, Scalf R, Sullivan M, Waller L, Zhu L. Examining associations between childhood asthma and traffic flow using a geographic information system. Environ Health Perspect. 1999;107:761–7.
Salvaggio J, Seabury J, Schoenhardt EA. New Orleans asthma: V. Relationship between Charity Hospital asthma admission rates, semiquantitative pollen and fungal spore counts, and total particulate aerometric sampling data. J Allergy Clin Immunol. 1971;48:96–114.
Seals B, Krasner A. Health Effects from Gas Stove Pollution. Rocky Mountain Institute, Physicians for Social Responsibility, Mothers Out Front, and Sierra Club. 2020. https://www.psr.org/wp-content/uploads/2020/05/health-effects-from-gas-stove-pollution.pdf.
Logue JM, Klepeis NE, Lobscheid AB, Singer BC. Pollutant exposures from natural gas cooking burners: a simulation-based assessment for Southern California. Environ Health Perspect. 2014;122:43–50.
U.S. Energy Information Administration. Residential Energy Consumption Survey (RECS). 2018. https://www.eia.gov/consumption/residential/data/2015/hc/php/hc3.6.php.
United States Environmental Protection Agency. Why Indoor Air Quality is Important to Schools. 2019. https://www.epa.gov/iaq-schools/why-indoor-air-quality-important-schools.
Belanger K, Holford TR, Gent JF, Hill ME, Kezik JM, Leaderer BP. Household Levels of Nitrogen Dioxide and Pediatric Asthma Severity. Epidemiology 2013;24:320–30.
World Health Organization. WHO guidelines for indoor air quality: selected pollutants. Geneva: World Health Organization; 2010.
Barck C, Lundahl J, Hallden G, Bylin G. Brief exposures to NO2 augment the allergic inflammation in asthmatics. Environ Res. 2005;97:58–66.
Klepeis NE, Nelson WC, Ott WR, Robinson JP, Tsang AM, Switzer P, et al. The National Human Activity Pattern Survey (NHAPS): a resource for assessing exposure to environmental pollutants. J Exposure Sci Environ Epidemiol. 2001;11:231–52.
Dong Q, Li B, Downen RS, Tran N, Chorvinsky E, Pillai DK, et al. A Cloud-Connected NO2 and Ozone Sensor System for Personalized Pediatric Asthma Research and Management. IEEE Sensors Journal. 2020;20:15143–53
Nathan RA, Sorkness CA, Kosinski M, Shatz M, Li JT, Marcus P, et al. Development of the Asthma Control Test: A Survey for Assessing Asthma Control. J Allergy Clin Immunol. 2004;113:59–65.
Tukey JW. Exploratory Data Analysis. Biometrical J. 1981;23:413–4.
Bonett DG, Wright TA. Sample size requirements for estimating Pearson, Kendall and Spearman correlations. Psychometrika 2000;65:23–28.
Altman DG, Gardner MJ. Regression and Correlation. In: Statistics With Confidence. London: John Wiley & Sons; 2000. p. 73–92.
Frampton MW,MD, Greaves IA,MD. NOx - NOX: Who’s There? Am J Respir CritCare Med. 2009;179:1077–83.
Schildcrout JS, Sheppard L, LT, Slaughter JC, Koenig JQ, Shapiro GG. Ambient air pollution and asthma exacerbations in children: an eight-city analysis. Am J Epidemiol. 2006;164:505–17.
Studnicka M, Hackl E, Pischinger J, Fangmeyer C, Haschke N, Kuhr J, et al. Traffic-related NO2 and the prevalence of asthma and respiratory symptoms in seven year olds. Eur Respiratory J. 1997;10:2275–8.
Brown JS. Nitrogen dioxide exposureand airway responsiveness in individuals with asthma. Inhalation Toxicol. 2015;27:1–14.
Lin S, Liu X, Le LH, Hwang SA. Chronic Exposure to Ambient Ozone and Asthma Hospital Admissions among Children. Environ Health Perspect. 2008;116:1725.
Lin M, Chen Y, Burnett RT, Villeneuve PJ, Krewsk D. Effect of short-term exposure to gaseous pollution on asthma hospitalisation in children: a bi-directional case-crossover analysis. J Epidemiol Community Health. 2003;57:50–55.
Strand V, Rak S, Svartengren M, Bylin G. Nitrogen dioxide exposure enhances asthmatic reaction to inhaled allergen in subjects with asthma. Am J Respiratory Crit Care Med. 1997;155:881–7.
U.S. Environmental Protection Agency. Risk and Exposure Assessment for Review of the Secondary National Ambient Air Quality Standards for Oxides of Nitrogen and Oxides of Sulfur. 2009. Accessed 2020 Apr. https://www3.epa.gov/ttn/naaqs/standards/no2so2sec/cr_rea.html.
Linn WS, Shamoo DA, Anderson KR, Peng RC, Avol EL, Hackney JD, et al. Short-term air pollution exposures and responses in Los Angeles area schoolchildren. J exposure Anal Environ Epidemiol. 1996;6:449–72.
National Research Council. Assessment of exposure-response functions for rocket-emission toxicants. Washington, DC: National Academies Press; 1998.
U.S. Environmental Protection Agency. Integrated Science Assessment for Oxides of Nitrogen—Health Criteria. 2008. Accessed Apr 2020. http://cfpub.epa.gov/ncea/cfm/recordisplay.cfm?deid=194645.
U.S. Environmental Protection Agency. Air Quality Criteria for Oxies of Nitrogen, Vol. 3. Washington, D.C.: U.S. Environmental Protection Agency; 1993.
U.S. Environmental Protection Agency. Nitrogen Dioxide (NO2) Pollution: History of the National Ambient Air Quality Standards for NO2. 2017. Accessed Apr 2020. https://www.epa.gov/no2-pollution/table-historical-nitrogen-dioxide-national-ambient-air-quality-standards-naaqs.
Achakulwisut P, Brauer M, Hystad P, Anenberg S. Global, national, and urban burdens of paediatric asthma incidence attributable to ambient NO2 pollution: estimates from global datasets. Lancet Planet Health. 2019;3:e166–e178.
Strand V, Svartengren M, Rak S, Barck C, Bylin G. Repeated exposure to an ambient level of NO2 enhances asthmatic response to a nonsymptomatic allergen dose. Eur Respiratory J. 1998;12:6–12.
O’Connor GT, Neas L, Vaughn B, Kattan M, Mitchell H, Crain EF, et al. Acute respiratory health effects of air pollution on children with asthma in US inner cities. J Allergy Clin Immunol. 2008;121:1133–9.
Utah Department of Health. Nitrogen Dioxide (NO2). 2016. Accessed Apr 2020l. https://www.health.utah.gov/utahair/pollutants/NO2/.
The National Institute for Occupational Safety and Health (NIOSH). NIOSH Pocket Giude to Chemical Hazards: Nitrogen dioxide. 2019. Accessed Apr 2020. https://www.cdc.gov/niosh/npg/npgd0454.html.
Acknowledgements
This work was supported by the National Institute of Biomedical Imaging and Bioengineering (NIBIB) of the National Institutes of Health (NIH). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. Clinical data was collected through Children’s National Hospital in accordance with a plan approved by the Institutional Review Board (IRB; #Pro00009593). Supported by National Institutes of Health grant 1U01EB021986-01. This paper is subject to the NIH Public Access Policy (http://publicaccess.nih.gov).
Author information
Authors and Affiliations
Contributions
RSD: conceptualization, methodology, validation, formal analysis, investigation, data curation, writing—original draft, writing—review and editing, visualization. QD: conceptualization, methodology, software, validation, formal analysis, data curation, writing—review and editing. EC: investigation, data curation, resources, writing—review and editing. BL: conceptualization, methodology, software, formal analysis, investigation, writing—review and editing. NT: software, data curation. JHJ: investigation, resources, data curation. DKP: conceptualization, methodology, formal analysis, investigation, resources, writing—review and editing, supervision, project administration, funding acquisition. MZ: conceptualization, methodology, formal analysis, resources, writing—review and editing, supervision, project administration, funding acquisition. ZL: conceptualization, methodology, formal analysis, resources, writing—review and editing, supervision, project administration, funding acquisition.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Scott Downen, R., Dong, Q., Chorvinsky, E. et al. Personal NO2 sensor demonstrates feasibility of in-home exposure measurements for pediatric asthma research and management. J Expo Sci Environ Epidemiol 32, 312–319 (2022). https://doi.org/10.1038/s41370-022-00413-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41370-022-00413-0