Abstract
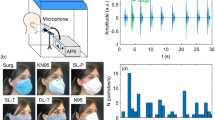
Respirator face masks (RFMs) as a personal-level intervention is increasingly being utilized to reduce ambient particulate matter (PM) exposure, globally. We tested the effectiveness of 50 commercially available ones in reducing the exposure of ambient particle number concentrations (PNC), PM10, PM2.5, and PM1 (PM ≤ 10, 2.5, and 1 μm in diameter, respectively) in a traffic-affected urban site in Tehran. To examine the efficiency of RFMs, we applied a specific experimental setup including vacuum pumps, dummy heads, connecting tubes, glass chambers, and GRIMM Aerosol Spectrometer to measure all metrics after dummy heads. The average effectiveness of RFMs was in the range of 0.7–83.5%, 3.5–68.1%, 0.8–46.1%, and 0.4–32.2% in reducing ambient PNC, PM10, PM2.5, and PM1, respectively. Considering all metrics, the highest effectiveness was observed always for Biomask, followed by 3 M 9332, due to their well-designed physical characteristics (e.g., adjustable nose clip for any face/nose shape, and size, soft inner material in the nose panel to provide a secure seal against leakage, adjustable or elasticated straps/ear loops to better adjust on any face). Biomask reduced ambient PM10 with a mean value of 94.6 μg m−3 (minimum–maximum: 51.7–100.3 μg m−3), whereas it filtered on average just 29.0 μg m−3 (25.7–43.5 μg m−3) of ambient PM2.5 and 18.2 μg m−3 (14.7–21.8 μg m−3) of PM1. A fuzzy analytical hierarchy process to find the most important design-related factors of RFMs affecting their effectiveness, which showed the exhalation valve and its diaphragm (20.4%), nose clip (19.7%), and cheek flaps (18.6%) are ranked as the main design-related variables. The fuzzy technique for order preference by similarity to ideal solution indicated that Biomask and 3M 9332 had scores of 1 and 0.97, the highest scores compared with other RFMs. This study provides crucial evidence-based results to elucidate the effectiveness and design-related factors of RFMs in real-environmental circumstances.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 6 print issues and online access
$259.00 per year
only $43.17 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout






Similar content being viewed by others
References
Brook RD, Newby DE, Rajagopalan S. The global threat of outdoor ambient air pollution to cardiovascular health: time for intervention. JAMA Cardiol. 2017;2:353–4.
Lelieveld J, Evans JS, Fnais M, Giannadaki D, Pozzer A. The contribution of outdoor air pollution sources to premature mortality on a global scale. Nature. 2015;525:367.
Hadley MB, Vedanthan R, Fuster V. Air pollution and cardiovascular disease: a window of opportunity. Nat Rev Cardiol. 2018;15:193.
Burnett R, Chen H, Szyszkowicz M, Fann N, Hubbell B, Pope CA, et al. Global estimates of mortality associated with long-term exposure to outdoor fine particulate matter. Proc Natl Acad Sci USA. 2018;115:9592–7.
Rajagopalan S, Al-Kindi SG, Brook RD. Air pollution and cardiovascular disease: JACC state-of-the-art review. J Am Coll Cardiol. 2018;72:2054–70.
Hadley MB, Baumgartner J, Vedanthan R. Developing a clinical approach to air pollution and cardiovascular health. Circulation. 2018;137:725–42.
Landrigan PJ, Fuller R, Acosta NJ, Adeyi O, Arnold R, Baldé AB, et al. The Lancet Commission on pollution and health. Lancet. 2018;391:462–512.
Apte JS, Brauer M, Cohen AJ, Ezzati M, Pope III CA. Ambient PM2. 5 reduces global and regional life expectancy. Environ Sci Technol Lett. 2018;5:546–51.
Fantke P, McKone TE, Tainio M, Jolliet O, Apte JS, Stylianou K, et al. Global effect factors for exposure to fine particulate matter. Environ Sci Technol. 2019;53:6855–68.
West JJ, Cohen A, Dentener F, Brunekreef B, Zhu T, Armstrong B, et al. What we breathe impacts our health: improving understanding of the link between air pollution and health. Environ Sci Technol. 2016:50:4895–904.
Barzeghar V, Sarbakhsh P, Hassanvand MS, Faridi S, Gholampour A. Long-term trend of ambient air PM10, PM2.5, and O3 and their health effects in Tabriz city, Iran, during 2006–17. Sustain Cities Soc. 2020;54:101988.
Shamsipour M, Hassanvand MS, Gohari K, Yunesian M, Fotouhi A, Naddafi K, et al. National and sub-national exposure to ambient fine particulate matter (PM2. 5) and its attributable burden of disease in Iran from 1990 to 2016. Environ Pollut. 2019;255:113173.
Laumbach R, Meng Q, Kipen H. What can individuals do to reduce personal health risks from air pollution? J Thorac Dis. 2015;7:96.
Langrish JP, Li X, Wang S, Lee MM, Barnes GD, Miller MR, et al. Reducing personal exposure to particulate air pollution improves cardiovascular health in patients with coronary heart disease. Environ Health Perspect. 2012;120:367.
Li H, Cai J, Chen R, Zhao Z, Ying Z, Wang L, et al. Particulate matter exposure and stress hormone levels: a randomized, double-blind, crossover trial of air purification. Circulation. 2017;136:618–27.
Zhang S, Li L, Gao W, Wang Y, Yao X. Interventions to reduce individual exposure of elderly individuals and children to haze: a review. J Thorac Dis. 2016;8:E62.
Shakya KM, Noyes A, Kallin R, Peltier RE. Evaluating the efficacy of cloth facemasks in reducing particulate matter exposure. J Expo Sci Environ Epidemiol. 2017;27:352.
Peck R, Grinshpun S, Yermakov M, Rao M, Kim J, Reponen T. Efficiency of portable HEPA air purifiers against traffic related combustion particles. Build Environ. 2016;98:21–29.
Cherrie JW, Apsley A, Cowie H, Steinle S, Mueller W, Lin C, et al. Effectiveness of face masks used to protect Beijing residents against particulate air pollution. Occup Environ Med. 2018;75:446–52.
Steinle S, Sleeuwenhoek A, Mueller W, Horwell CJ, Apsley A, Davis A, et al. The effectiveness of respiratory protection worn by communities to protect from volcanic ash inhalation. Part II: Total inward leakage tests. Int J Hyg Environ Health. 2018;221:977–84.
Mueller W, Horwell CJ, Apsley A, Steinle S, McPherson S, Cherrie JW, et al. The effectiveness of respiratory protection worn by communities to protect from volcanic ash inhalation. Part I: Filtration efficiency tests. Int J Hyg Environ Health. 2018;221:967–76.
Chen R, Zhao A, Chen H, Zhao Z, Cai J, Wang C, et al. Cardiopulmonary benefits of reducing indoor particles of outdoor origin: a randomized, double-blind crossover trial of air purifiers. J Am Coll Cardiol. 2015;65:2279–87.
Giles LV, Barn P, Künzli N, Romieu I, Mittleman MA, van Eeden S, et al. From good intentions to proven interventions: effectiveness of actions to reduce the health impacts of air pollution. Environ Health Perspect. 2010;119:29–36.
Morishita M, Adar SD, D’Souza J, Ziemba RA, Bard RL, Spino C, et al. Effect of portable air filtration systems on personal exposure to fine particulate matter and blood pressure among residents in a low-income senior facility: a randomized clinical trial. JAMA Intern Med. 2018;178:1350–7.
Barrett JR. Air pollution intervention: study links use of face masks to improved cardiovascular outcomes. Natl Inst Environ Health Sci. 2012;120:a122.
Langrish JP, Mills NL, Chan JK, Leseman DL, Aitken RJ, Fokkens PH, et al. Beneficial cardiovascular effects of reducing exposure to particulate air pollution with a simple facemask. Part Fibre Toxicol. 2009;6:8.
Zhang J, Mu Q. Air pollution and defensive expenditures: evidence from particulate-filtering facemasks. J Environ Econ Manag. 2017;92:517–36.
Shi J, Lin Z, Chen R, Wang C, Yang C, Cai J, et al. Cardiovascular benefits of wearing particulate-filtering respirators: a randomized crossover trial. Environ Health Perspect. 2016;125:175–80.
Patel D, Shibata T, Wilson J, Maidin A. Challenges in evaluating PM concentration levels, commuting exposure, and mask efficacy in reducing PM exposure in growing, urban communities in a developing country. Sci Total Environ. 2016;543:416–24.
van Dorn A. Clearing the air: do facemasks protect health? Lancet Respir Med. 2017;5:555–6.
Cheng Z, Luo L, Wang S, Wang Y, Sharma S, Shimadera H, et al. Status and characteristics of ambient PM2. 5 pollution in global megacities. Environ Int. 2016;89:212–21.
Pacitto A, Amato F, Salmatonidis A, Moreno T, Alastuey A, Reche C, et al. Effectiveness of commercial face masks to reduce personal PM exposure. Sci Total Environ. 2019;650:1582–90.
Morishita M, Wang L, Speth K, Zhou N, Bard RL, Li F, et al. Acute blood pressure and cardiovascular effects of near-roadway exposures with and without N95 respirators. Am J Hypertens. 2019;32:1054–65.
Faridi S, Shamsipour M, Krzyzanowski M, Künzli N, Amini H, Azimi F, et al. Long-term trends and health impact of PM 2.5 and O3 in Tehran, Iran, 2006–2015. Environ Int. 2018;114:37–49.
Faridi S, Niazi S, Yousefian F, Azimi F, Pasalari H, Momeniha F, et al. Spatial homogeneity and heterogeneity of ambient air pollutants in Tehran. Sci Total Environ. 2019;697:123–34.
Faridi S, Niazi S, Shamsipour M, Hassanvand MS. Comments on:” Meteorological correlates and AirQ+ health risk assessment of ambient fine particulate matter in Tehran, Iran”. Environ Res. 2019;174:122.
Bayat R, Ashrafi K, Motlagh MS, Hassanvand MS, Daroudi R, Fink G, et al. Health impact and related cost of ambient air pollution in Tehran. Environ Res. 2019;176:108547.
Yousefian F, Faridi S, Azimi F, Aghaei M, Shamsipour M, Yaghmaeian K, et al. Temporal variations of ambient air pollutants and meteorological influences on their concentrations in Tehran during 2012–2017. Sci Rep. 2020;10:1–11.
Huang W, Morawska L. Face masks could raise pollution risks. Nature. 2019;574:29–30.
Jung H, Kim J, Lee S, Lee J, Kim J, Tsai P, et al. Comparison of filtration efficiency and pressure drop in anti-yellow sand masks, quarantine masks, medical masks, general masks, and handkerchiefs. Aerosol Air Qual Res. 2014;14:991–1002.
Bard RL, Ijaz MK, Zhang JJ, Li Y, Bai C, Yang Y, et al. Interventions to reduce personal exposures to air pollution: a primer for health care providers. Glob heart. 2019;14:47.
Horwell C, Ferdiwijaya D, Wahyudi T, Dominelli L. Use of respiratory protection in Yogyakarta during the 2014 eruption of Kelud, Indonesia: community and agency perspectives. J Volcanol Geotherm Res. 2017;382:92–102.
Rengasamy S, Zhuang Z, Niezgoda G, Walbert G, Lawrence R, Boutin B, et al. A comparison of total inward leakage measured using sodium chloride (NaCl) and corn oil aerosol methods for air-purifying respirators. J Occup Environ Hyg. 2018;15:616–27.
Guan T, Hu S, Han Y, Wang R, Zhu Q, Hu Y, et al. The effects of facemasks on airway inflammation and endothelial dysfunction in healthy young adults: a double-blind, randomized, controlled crossover study. Part Fibre Toxicol. 2018;15:30.
Rengasamy S, Walbert GF, Newcomb WE, Faulkner K, Rengasamy MM, Brannen JJ, et al. Total inward leakage measurement of particulates for N95 filtering facepiece respirators—a comparison study. Ann Occup Hyg. 2013;58:206–16.
Rengasamy S, Eimer BC. Total inward leakage of nanoparticles through filtering facepiece respirators. Ann Occup Hyg. 2011;55:253–63.
Kelkar U, Gogate B, Kurpad S, Gogate P, Deshpande M. How effective are face masks in operation theatre? A time frame analysis and recommendations. Int J Infect Control 2013;9.
Shaffer RE, Rengasamy S. Respiratory protection against airborne nanoparticles: a review. J Nanopart Res. 2009;11:1661.
Kang M. Assessment of NIOSH-approved N95 filter performance against varying conditions. 2011. https://ir.uiowa.edu/etd/2722/.
Rengasamy S, Shaffer R, Williams B, Smit S. A comparison of facemask and respirator filtration test methods. J Occup Environ Hyg. 2017;14:92–103.
Lai A, Poon C, Cheung A. Effectiveness of facemasks to reduce exposure hazards for airborne infections among general populations. J R Soc Interface. 2011;9:938–48.
Li J, Chen H, Li X, Wang M, Zhang X, Cao J, et al. Differing toxicity of ambient particulate matter (PM) in global cities. Atmos Environ. 2019;212:305–15.
Amato F. Non-exhaust emissions: an urban air quality problem for public health; impact and mitigation measures. (Academic Press; 2018).
Yousefian F, Mahvi AH, Yunesian M, Hassanvand MS, Kashani H, Amini H. Long-term exposure to ambient air pollution and autism spectrum disorder in children: a case-control study in Tehran, Iran. Sci total Environ. 2018;643:1216–22.
Chen G, Morawska L, Zhang W, Li S, Cao W, Ren H, et al. Spatiotemporal variation of PM1 pollution in China. Atmos Environ. 2018;178:198–205.
Hassanvand MS, Naddafi K, Faridi S, Arhami M, Nabizadeh R, Sowlat MH, et al. Indoor/outdoor relationships of PM10, PM2. 5, and PM1 mass concentrations and their water-soluble ions in a retirement home and a school dormitory. Atmos Environ. 2014;82:375–82.
Meng X, Ma Y, Chen R, Zhou Z, Chen B, Kan H. Size-fractionated particle number concentrations and daily mortality in a Chinese city. Environ Health Perspect. 2013;121:1174–8.
Hassanvand MS, Naddafi K, Faridi S, Nabizadeh R, Sowlat MH, Momeniha F, et al. Characterization of PAHs and metals in indoor/outdoor PM10/PM2. 5/PM1 in a retirement home and a school dormitory. Sci Total Environ. 2015;527:100–10.
Hassanvand MS, Naddafi K, Kashani H, Faridi S, Kunzli N, Nabizadeh R, et al. Short-term effects of particle size fractions on circulating biomarkers of inflammation in a panel of elderly subjects and healthy young adults. Environ Pollut. 2017;223:695–704.
Vallero DA. Fundamentals of air pollution. (Academic press; 2014).
Moya J, Phillips L, Schuda L, Wood P, Diaz A, Lee R, et al. Exposure factors handbook 2011 edn (Final Report). US Environmental Protection Agency, Washington, DC, EPA/600/R-09/052F, 2011.
Gumus AT. Evaluation of hazardous waste transportation firms by using a two step fuzzy-AHP and TOPSIS methodology. Exp Syst Appl. 2009;36:4067–74.
Sun C-C. A performance evaluation model by integrating fuzzy AHP and fuzzy TOPSIS methods. Exp Syst Appl. 2010;37:7745–54.
Borza S, Inta M, Serbu R, Marza B. Multi-criteria analysis of pollution caused by auto traffic in a geographical area limited to applicability for an eco-economy environment. Sustainability. 2018;10:4240.
Yao B-g, Wang Y-x, Ye X-y, Zhang F, Peng Y-l. Impact of structural features on dynamic breathing resistance of healthcare face mask. Sci Total Environ. 2019;689:743–53.
Mahdavi A, Bahloul A, Haghighat F, Ostiguy C. Contribution of breathing frequency and inhalation flow rate on performance of N95 filtering facepiece respirators. Ann Occup Hyg. 2013;58:195–205.
Acknowledgements
This study was financially supported by the Iran National Science Foundation (INSF) (grant number: 97011909). The authors are also grateful to Institute for Environmental Research (IER), Tehran Heart Center (THC), and the Exceptional Talents Development Center at Tehran University of Medical Sciences. It should be noted that the use of any brand names in the current study in no way endorses the use of its RFM and other products. This article is the first part of a randomized crossover trial entitled “Evaluating performance of face masks in reducing ambient particulate matter exposure and their wearing on acute cardiovascular effects” with registration number “IRCT20181214041961N1”, in Tehran megacity and its results will be used in the next article. We sincerely acknowledge Sadegh Niazi, PhD candidate at Queensland University of Technology, for his assistance in the revision of our manuscript.
Author information
Authors and Affiliations
Contributions
SF, MSH, and KN provided the idea for this work and designed the method. SF, MSH, and SHN performed the experiments. SF and RNN contributed to the data analysis. SF prepared all figures and tables, and wrote the main manuscript. SS, MH, MT, MY, and MSH revised the manuscript.
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Faridi, S., Nodehi, R.N., Sadeghian, S. et al. Can respirator face masks in a developing country reduce exposure to ambient particulate matter?. J Expo Sci Environ Epidemiol 30, 606–617 (2020). https://doi.org/10.1038/s41370-020-0222-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41370-020-0222-6
Keywords
This article is cited by
-
Cardiovascular health effects of wearing a particulate-filtering respirator to reduce particulate matter exposure: a randomized crossover trial
Journal of Human Hypertension (2022)
-
Quantitative fit testing of filtering face-piece respirators during the COVID-19 pandemic reveals anthropometric deficits in most respirators available in Iran
Journal of Environmental Health Science and Engineering (2021)