Abstract
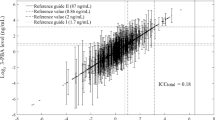
Single-spot urine is often used to estimate organophosphorus insecticide (OP) exposure. However, variations of urinary metabolite concentrations during the day are considerable as OP half-lives are short and as diet is their main exposure source. In addition, quality control is indispensable for institutions that analyze these metabolites. This study aimed to clarify (1) adequate frequencies of urine collection for estimating OP exposure and (2) interlaboratory variation in measured concentrations of OP metabolites, dialkylphosphates (DAPs). To quantify intra-individual variations, urine was collected eight times during a period that spanned 5 consecutive days from nine children aged 5–6 years. For interlaboratory variations, 41 spot samples from 14 pregnant women and 13 three-year-old children were used. Intraclass correlation coefficients for the DAPs were moderate but misclassification occurred in > 50% of the surrogate category analyses using single measurements. The misclassification frequency decreased to satisfactory levels when three temporal measurements were conducted. Values of four DAPs measured in the two laboratories correlated well except in the cases of urine samples obtained from two pregnant women. In conclusion, urinary DAPs should be measured from spot urine samples obtained during 3 different days. Sharing matrix-contained standards and quality control samples should minimize interlaboratory variations.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 6 print issues and online access
$259.00 per year
only $43.17 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Burns CJ, McIntosh LJ, Mink PJ, Jurek AM, Li AA. Pesticide exposure and neurodevelopmental outcomes: review of the epidemiologic and animal studies. J Toxicol Environ Health B Crit Rev. 2013;16:127–283.
Gonzalez-Alzaga B, Lacasana M, Aguilar-Garduno C, Rodriguez-Barranco M, Ballester F, Rebagliato M, et al. A systematic review of neurodevelopmental effects of prenatal and postnatal organophosphate pesticide exposure. Toxicol Lett. 2014;230:104–21.
Munoz-Quezada MT, Lucero BA, Barr DB, Steenland K, Levy K, Ryan PB, et al. Neurodevelopmental effects in children associated with exposure to organophosphate pesticides: a systematic review. Neurotoxicology. 2013;39:158–68.
Bouchard MF, Bellinger DC, Wright RO, Weisskopf MG. Attention-deficit/hyperactivity disorder and urinary metabolites of organophosphate pesticides. Pediarics. 2010;125:e1270–7.
Marks AR, Harley K, Bradman A, Kogut K, Barr DB, Johnson C, et al. Organophosphate pesticide exposure and attention in young Mexican-American children: the CHAMACOS study. Environ Health Perspect. 2010;118:1768–74.
Eskenazi B, Marks AR, Bradman A, Harley K, Barr DB, Johnson C, et al. Organophosphate pesticide exposure and neurodevelopment in young Mexican-American children. Environ Health Perspect. 2007;115:792–8.
Jurewicz J, Hanke W. Prenatal and childhood exposure to pesticides and neurobehavioral development: review of epidemiological studies. Int J Occup Med Environ Health. 2008;21:121–32.
Rauh VA, Garfinkel R, Perera FP, Andrews HF, Hoepner L, Barr DB, et al. Impact of prenatal chlorpyrifos exposure on neurodevelopment in the first 3 years of life among inner-city children. Pediatrics. 2006;118:e1845–59.
Engel SM, Wetmur J, Chen J, Zhu C, Barr DB, Canfield RL, et al. Prenatal exposure to organophosphates, paraoxonase 1, and cognitive development in childhood. Environ Health Perspect. 2011;119:1182–8.
Gunier RB, Bradman A, Harley KG, Kogut K, Eskenazi B. Prenatal residential proximity to agricultural pesticide use and IQ in 7-year-old children. Environ Health Perspect. 2017;125:057002.
Rowe C, Gunier R, Bradman A, Harley KG, Kogut K, Parra K, et al. Residential proximity to organophosphate and carbamate pesticide use during pregnancy, poverty during childhood, and cognitive functioning in 10-year-old children. Environ Res. 2016;150:128–37.
Stein LJ, Gunier RB, Harley K, Kogut K, Bradman A, Eskenazi B. Early childhood adversity potentiates the adverse association between prenatal organophosphate pesticide exposure and child IQ: the CHAMACOS cohort. Neurotoxicology. 2016;56:180–7.
Fenske RA, Lu C, Curl CL, Shirai JH, Kissel JC. Biologic monitoring to characterize organophosphorus pesticide exposure among children and workers: an analysis of recent studies in Washington State. Environ Health Perspect. 2005;113:1651–7.
Lu C, Toepel K, Irish R, Fenske RA, Barr DB, Bravo R. Organic diets significantly lower children’s dietary exposure to organophosphorus pesticides. Environ Health Perspect. 2006;114:260–3.
Needham LL. Assessing exposure to organophosphorus pesticides by biomonitoring in epidemiologic studies of birth outcomes. Environ Health Perspect. 2005;113:494–8.
Barr DB. Biomonitoring of exposure to pesticides. J Chem Health Saf. 2008;15:20–9.
Attfield KR, Hughes MD, Spengler JD, Lu C. Within- and between-child variation in repeated urinary pesticide metabolite measurements over a 1-year period. Environ Health Perspect. 2014;122:201–6.
Bradman A, Kogut K, Eisen EA, Jewell NP, Quiros-Alcala L, Castorina R, et al. Variability of organophosphorous pesticide metabolite levels in spot and 24-hr urine samples collected from young children during 1 week. Environ Health Perspect. 2013;121:118–24.
Fortenberry GZ, Meeker JD, Sanchez BN, Barr DB, Panuwet P, Bellinger D, et al. Urinary 3,5,6-trichloro-2-pyridinol (TCPY) in pregnant women from Mexico City: distribution, temporal variability, and relationship with child attention and hyperactivity. Int J Hyg Environ Health. 2014;217:405–12.
Griffith W, Curl CL, Fenske RA, Lu CA, Vigoren EM, Faustman EM. Organophosphate pesticide metabolite levels in pre-school children in an agricultural community: within- and between-child variability in a longitudinal study. Environ Res. 2011;111:751–6.
Hornung RW, Reed LD. Estimation of average concentration in the presence of nondetectable values. Appl Occup Environ Hyg. 1990;5:46–51.
Goen T, Schaller KH, Drexler H. External quality assessment of human biomonitoring in the range of environmental exposure levels. Int J Hyg Environ Health. 2012;215:229–32.
Prapamontol T, Sutan K, Laoyang S, Hongsibsong S, Lee G, Yano Y, et al. Cross validation of gas chromatography-flame photometric detection and gas chromatography-mass spectrometry methods for measuring dialkylphosphate metabolites of organophosphate pesticides in human urine. Int J Hyg Environ Health. 2014;217:554–66.
Kawamoto T, Nitta H, Murata K, Toda E, Tsukamoto N, Hasegawa M, et al. Rationale and study design of the Japan environment and children’s study (JECS). BMC Public Health. 2014;14:25.
Ueyama J, Saito I, Takaishi A, Nomura H, Inoue M, Osaka A, et al. A revised method for determination of dialkylphosphate levels in human urine by solid-phase extraction and liquid chromatography with tandem mass spectrometry: application to human urine samples from Japanese children. Environ Health Prev Med. 2014;19:405–13.
Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33:159–74.
Spaan S, Pronk A, Koch HM, Jusko TA, Jaddoe VW, Shaw PA, et al. Reliability of concentrations of organophosphate pesticide metabolites in serial urine specimens from pregnancy in the Generation R Study. J Exp Sci Environ Epidemiol. 2015;25:286–94.
Lewis RC, Cantonwine DE, Del Toro LV, Calafat AM, Valentin-Blasini L, Davis MD, et al. Distribution and determinants of urinary biomarkers of exposure to organophosphate insecticides in Puerto Rican pregnant women. Sci Total Environ. 2015;512–3:337–44.
Garfitt SJ, Jones K, Mason HJ, Cocker J. Exposure to the organophosphate diazinon: data from a human volunteer study with oral and dermal doses. Toxicol Lett. 2002;134:105–13.
Griffin P, Mason H, Heywood K, Cocker J. Oral and dermal absorption of chlorpyrifos: a human volunteer study. Occup Environ Med. 1999;56:10–3.
Becker K, Seiwert M, Angerer J, Kolossa-Gehring M, Hoppe HW, Ball M, et al. GerES IV pilot study: assessment of the exposure of German children to organophosphorus and pyrethroid pesticides. Int J Hyg Environ Health. 2006;209:221–33.
Berman T, Goldsmith R, Goen T, Spungen J, Novack L, Levine H, et al. Urinary concentrations of organophosphate pesticide metabolites in adults in Israel: demographic and dietary predictors. Environ Int. 2013;60:183–9.
Li Z, Romanoff LC, Lewin MD, Porter EN, Trinidad DA, Needham LL, et al. Variability of urinary concentrations of polycyclic aromatic hydrocarbon metabolite in general population and comparison of spot, first-morning, and 24-h void sampling. J Exp Sci Environ Epidemiol. 2010;20:526–35.
Zheng J, Liu L, Wang J, Jin Q. Urinary proteomic and non-prefractionation quantitative phosphoproteomic analysis during pregnancy and non-pregnancy. BMC Genomics. 2013;14:777.
Acknowledgements
This investigation was conducted as adjunct Study of Japan Environment and Children’s Study (JECS) at the Miyagi and Aichi regional Centers. Although JECS was funded by the Ministry of the Environment, Japan, the findings and conclusions of this article solely represent the authors and are not representative of the official views of the above government. This study was supported by the Environment Research and Technology Development Fund (5–1451) of the Ministry of the Environment, Japan.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflicts of interest.
Ethics approval
This study was approved by the Ethical Review Board of the Nagoya City University Graduate School of Medical Sciences.
Informed consent
Informed consent was obtained from all subjects.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Ito, Y., Ueyama, J., Nakayama, S.F. et al. Within-individual and interlaboratory variability analyses of urinary metabolites measurements of organophosphorus insecticides. J Expo Sci Environ Epidemiol 30, 721–729 (2020). https://doi.org/10.1038/s41370-019-0124-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41370-019-0124-7
Keywords
This article is cited by
-
Toxicity and degradation of the insecticide monocrotophos
Environmental Chemistry Letters (2019)