Abstract
Aims
Body weight loss improves insulin resistance and growth hormone secretion in obesity, which may be regulated by leptin according to preclinical studies. How changes in leptin, lipids and insulin sensitivity after bariatric (metabolic) surgery affect the human growth hormone system is yet unclear.
Participants and methods
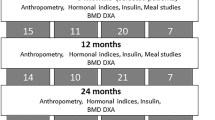
People with obesity (OBE, n = 79, BMI 50.8 ± 6.3 kg/m2) were studied before, 2, 12, 24 and 52 weeks after metabolic surgery and compared to lean healthy humans (control; CON, n = 24, BMI 24.3 ± 3.1 kg/m2). Tissue-specific insulin sensitivity was assessed by hyperinsulinemic-euglycemic clamps with D-[6,6-2H2]glucose. Fasting leptin, growth hormone (GH), insulin-like growth factor 1 (IGF-1) and IGF-binding proteins (IGFBP1, IGFBP3) were measured using ELISA.
Results
At baseline, OBE exhibited higher glycemia and leptinemia as well as pronounced peripheral, adipose tissue and hepatic insulin resistance compared to CON. GH and IGFBP1 were lower, while IGF1 was comparable between groups. At 52 weeks, OBE had lost 33% body weight and doubled their peripheral insulin sensitivity, which was paralleled by continuous increases in GH, IGF-1 and IGFBP1 as well as decrease in leptin. The rise in GH correlated with reductions in free fatty acids, adipose tissue insulin resistance and insulinemia, but not with changes in body weight, peripheral insulin sensitivity, glycemia or leptinemia. The rise in IGF-1 correlated with reduction in high-sensitive C-reactive protein.
Conclusion
Reversal of alterations of the GH-IGF-1 axis after surgically-induced weight loss is unlikely related to improved leptin secretion and/or insulin sensitivity, but is rather associated with restored adipose tissue function and reduced low-grade inflammation.
Similar content being viewed by others
Introduction
The rising prevalence of obesity and its associated complications such as type 2 diabetes (T2D), cardiovascular disease or cancers is becoming an increasing burden to healthcare systems globally [1]. In addition, endocrine disorders such as thyroid dysfunction [2] and particularly impaired growth hormone (GH) secretion [3] have been linked to the obesity epidemic.
Body weight loss improves insulin sensitivity even leading to remission of T2D, but may also normalise GH secretion by yet unclear mechanisms [4]. Effective weight loss upon bariatric (metabolic) surgery has been shown to profoundly alter gastrointestinal hormones controlling glucose and energy homoeostasis [5] but also to increase circulating GH concentrations. In contrast, cross-sectional studies on its impact on circulating insulin-like growth factor 1 (IGF-1) revealed conflicting results, by showing unchanged [6,7,8], decreased [9, 10] or even increased concentrations [11, 12] in lean humans compared with people with obesity. IGF-1 is involved in the regulation of both GH and insulin secretion to promote physiological carbohydrate and lipid metabolism [13], but its contribution to the improvement in tissue-specific insulin sensitivity after bariatric surgery also remains unclear.
The complex regulation of the GH-IGF-1 axis includes hypothalamic neuropeptides, ghrelin, insulin, free fatty acids (FFA), nutritional factors and IGF1-binding proteins (IGFBPs) [14]. Leptin, a key signal of long-term energy availability and an indicator of fat mass, inhibits GH secretion [15] and has been implicated in the regulation of IGF-1 secretion [16]. Indeed, recent studies showed that leptin substitution in children increases IGF-1 levels [17]. Furthermore, improvement of insulin sensitivity after metabolic surgery determines the restoration of leptin sensitivity through a molecular mechanism involving fatty acid-control of muscle malonyl-Co-A synthesis [15], indicating a direct link between leptin levels and lipid availability. Furthermore, increased muscle lipid oxidation pathways and regulation of muscle differentiation in people with obesity at 52 weeks after metabolic surgery [18] could relate to improved leptin and GH secretion. However, a direct association and possible mediators have not been demonstrated so far.
Previous studies were performed on rather small cohorts without detailed metabolic characterisation or without a lean control group and longer-term recording of the GH-IGF-1 axis after metabolic surgery [9, 15, 19,20,21,22]. The present study closely monitored the post-surgical time course of changes in the GH-IGF1 axis in comprehensively phenotyped individuals with class 3 obesity to elucidate factors associated with the reversal of altered GH-IGF-1 secretion. We hypothesised that post-surgical GH-IGF-1 axis improvements relate to the restoration of adipose tissue dysfunction and insulin sensitivity via changes in the secretion patterns of adipokines and pro-inflammatory cytokines.
Methods
Study population
We studied people with obesity of Caucasian origin (OBE, n = 79) before and 2, 12, 24 and 52 weeks after sleeve gastrectomy (n = 30) or gastric bypass surgery (n = 49). Healthy Caucasians without obesity were examined once as controls (CON, n = 24). T2D was present in 19 of the participants with obesity. All participants were non-smokers, engaged only in light physical activity and neither had previous pituitary disease (including known GH deficiency) or surgery nor received GH replacement. Data of some participants were part of previous reports of the BARIA_DDZ cohort [18, 23]. They provided informed written consent to this registered clinical cohort study (NCT01477957), which was approved by the ethics board of Heinrich-Heine University and University Hospital Düsseldorf and the ethics board of the North Rhine regional physicians’ association.
Clamp test
Each participant underwent 3 h hyperinsulinemic-euglycemic clamps employing the isotopic dilution technique using D-[6,6-2H2]glucose for measuring whole-body (mainly skeletal muscle) insulin sensitivity from insulin-stimulated rate of glucose disposal (clamp-Rd) [18, 23]. Fasting hepatic insulin sensitivity (HIS) was calculated by the formula: 100/[fasting endogenous glucose production (EGP)*fasting insulin] [23]. Adipose tissue insulin resistance was assessed in the fasted state from Adipo-IR, calculated as FFAfasting*insulinfasting, [24, 25] and during the hyperinsulinemic-euglycemic clamp from the percent suppression of FFA concentrations, calculated as [FFAfasting -FFAclamp360 min]*100/FFAfasting [26, 27]. Steady-state rates of glucose appearance (Ra) were calculated as [tracer infusion rate]*[tracer enrichment]/[percent tracer enrichment in plasma]-[tracer infusion rate] [28]. While in the fasted state, EGP equals Ra, clamp-Ra and -Rd were calculated using Steele’s steady state equations.
Blood analyses
Blood samples were collected before and during clamps for measuring hormones and metabolites. Metabolites, insulin, C-peptide, hsCRP, transforming growth factor β1 (TGFβ1), interleukin 1 receptor antagonist (IL-1ra), CC chemokine ligand 18 (CCL18), total adiponectin and leptin were quantified as described [29,30,31]. In vitro lipolysis was prevented by collecting blood into orlistat-containing vials [32] for microfluorimetrical FFA quantification (Wako Chem USA Inc. Osaka, Japan). Serum concentrations of GH, IGF-1, IGFBP1 and IGFBP3 were measured by ELISA (Quantikine® ELISA immunoassay, R&D Systems, Inc., MN, USA) in samples obtained in the morning after overnight fasting. The intraassay coefficients of variations (CVs) for GH, IGF-1, IGFBP1 and IGFBP3 were 3.6%, 2.3%, 2.7% and 1.4%, respectively, and interassay CVs for GH, IGF-1, IGFBP1 and IGFBP3 were 6.5%, 3.5%, 6.8% and 9.6%, respectively.
Statistical evaluation
Normally distributed parameters are presented as means ± SD or means ± SEM, otherwise as median (Q1;Q3). Not-normally distributed data were loge-transformed to achieve near-normal distribution. Statistical analyses using covariance pattern model for repeated measures analysis were performed. Analysis of covariance (ANCOVA) models of the cohort of participants with obesity as well as regression models were adjusted for age and sex and performed using SAS (version 9.4; SAS Institute, Cary, NC, USA).
Results
OBE exhibit lower circulating GH, but not IGF-1 levels than CON
Before surgery (baseline), OBE had similar age, but higher fasting glycemia and Adipo-IR as well as lower clamp-Rd and HIS when compared to CON (Table 1, Fig. 1a, b). They also had higher plasma FFA but comparable triglycerides (Table 1). Serum insulin, leptin and IGFBP3 were higher, IGF-1 similar, while GH and IGFBP1 were lower in OBE (Table 1, Fig. 2a–d). BMI was higher in individuals with T2D compared to those without T2D, but levels of leptin, GH, IGF-1, IGFBP1 and IGFBP3 were comparable (Suppl. Fig. 1).
Changes in rate of glucose disposal during the hyperinsulinemic-euglycemic clamp (clamp-Rd) (a), hepatic insulin sensitivity index (HIS) (b), leptin (c), total adiponectin (d), interleukin 1 receptor antagonist (IL-1ra) (e) and transforming growth factor β1 (TGFβ1) (f). Control humans depicted by green circles, people with obesity before (0 w) and 2, 12, 24 and 52 weeks after surgery depicted by orange circles. Data are mean ± SEM, #p < 0.05 vs controls, *p < 0.05 vs obese at baseline (0 w).
Changes in growth hormone (GH) (a), insulin-like growth factor-1 (IGF-1) (b), IGF-1 binding protein 1 (IGFBP1) (c) and IGFBP3 (d). Control humans depicted by green circles, people with obesity before (0 w) and 2, 12, 24 and 52 weeks after surgery depicted by orange circles. Data are mean ± SEM, #p < 0.05 vs controls, *p < 0.05 vs obese at baseline (0 w).
GH rapidly and continuously rises, while IGF-1 levels transiently decrease upon metabolic surgery
At 2 weeks after surgery, body weight loss of 10 ± 3 kg was paralleled by a transient increase in FFA, Adipo-IR and HIS, but no change in whole-body insulin sensitivity (Table 1, Fig. 1a, b). Serum insulin, insulin-mediated percent FFA suppression and leptin decreased in OBE early after surgery (Table 1, Fig. 1c). In parallel, the pro-inflammatory biomarkers, IL-1ra and TGFβ1, were transiently higher (p < 0.01) or tended to be higher (p = 0.11), respectively, compared to baseline (Fig. 1e, f).
Until 52 weeks after surgery, OBE exhibited an average weight loss of 33% and continuous improvements in whole-body, adipose tissue and HIS (Fig. 1a, b, Table 1). Similarly, glycemia, Adipo-IR, FFA, hsCRP and IL-1ra were normalised at 52 weeks (Table 1, Fig. 1e). Serum insulin, CCL18 and leptin levels were decreased by 63%, 34% and 65% at 52 weeks, respectively (Table 1, Fig. 1c), while total adiponectin markedly increased (Fig. 1d). Time courses of changes in BMI, insulin, glucose, HbA1c, triglycerides, FFA, hsCRP, Adipo-IR and IL-6 have been reported in a previous analysis of the BARIA_DDZ cohort [18].
At 2 weeks, serum GH and IGFBP1 were already increased, but IGF-1 and IGFBP3 levels dropped by 28% and 6% from baseline, respectively (Fig. 2b, d). During the follow-up, GH and IGFBP1 levels continuously rose and were higher or equal to that of CON, respectively, at 52 weeks (Fig. 2a, c). IGF-1 rose only later, at 24 and 52 weeks after surgery (Fig. 2b).
In participants with T2D, body weight loss was lower, but improvement of adipose tissue insulin sensitivity was higher at 24 and 52 weeks after surgery compared to participants without T2D (Suppl. Fig. 1). Increases in IGFBP1 at 12 weeks and IGFBP3 at 52 weeks were higher in individuals without T2D compared to participants with T2D (Suppl. Fig. 1). Despite lower peripheral insulin sensitivity at baseline (p < 0.0001, data not shown), participants with T2D had greater improvements in insulin-stimulated Rd at 2, 12, and 52 weeks compared to participants without T2D (p = 0.007, p = 0.0006 and p = 0.02, respectively, data not shown).
Of note, there were no differences in the time courses of changes of BMI, hepatic and adipose tissue insulin sensitivity as well as GH, IGF-1, IGFBP1, IGFBP3 and leptin concentrations between participants undergoing sleeve gastrectomy and gastric bypass surgery (Suppl. Fig. 2).
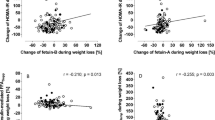
Reversal of the GH/IGF1 system relates to improved FFA and adipose tissue insulin sensitivity, but not whole-body insulin sensitivity
Multiple regression analysis adjusted for age and sex revealed no association between the long-term improvement in GH concentrations and changes in body weight, peripheral or HIS, glycemia or leptin levels, but a negative association with the reduction in insulinemia, FFA, and Adipo-IR (Table 2). The 52-week increase in IGF-1 related positively to the changes in leptin and insulin and negatively to the changes in hsCRP (Table 2). Of note, the transient lowering of IGF-1 at 2 weeks related to the increase in hsCRP, while the decrease in IGFBP3 related to the increase in Adipo-IR and hsCRP (p = 0.04, p = 0.04 and p = 0.03, respectively, data not shown). The 2-week increase of IGFBP1 related positively to the higher FFA concentrations (p = 0.008, data not shown).
Discussion
This study demonstrates that the reversal of alterations of the GH-IGF-1 axis after bariatric surgery relates to improvements in adipose tissue function, but not whole-body and HIS. In particular, normalisation of the obesity-related so-called “functional hyposomatotropism” by surgical weight loss is associated with the reduction in lipid availability, adipose tissue insulin resistance and low-grade inflammation, underlining an important role of adipose tissue also for the regulation of GH-IGF-1 axis in metabolic diseases.
First, this study found lower GH concentrations in humans with obesity than in lean humans in the setting of similar IGF-1 concentrations, indicating a preserved IGF-1 feedback mechanism. Alterations of the GH-IGF-1 axis in obesity have been demonstrated previously by reduced fasting or stimulated GH [8, 33] and controversial data has been reported for IGF-1 concentrations [3, 34]. The latter is likely due to the complex regulation of IGF-1, which in addition to GH involves several other factors, e. g. hypothalamic neuropeptides, ghrelin, insulin, FFA, macronutrients and IGFBPs [14, 35].
The observed increase in GH and IGF-1 levels confirms data at 6- and 12-m follow-up from other prospective bariatric surgery cohorts [9, 19, 22, 36], while the novel data for the 2-w timepoint allows further insights into short-term changes. These revealed a transient reduction in IGF-1 and IGFBP3 levels, which associated with increased hsCRP, suggesting a tight link between inflammatory processes and IGF-1 signaling. This is supported by data showing that interleukin 1 (IL-1), tumour necrosis factor α and the mitogen activated protein kinase pathway regulate IGF-1 and IGFBPs in cross-sectional human [37] and mechanistic rodent studies [38]. The present study also showed a negative association between circulating GH and insulin levels in line with the observation of fasting insulin as a predictor of integrated 24-h GH release [39]. Indeed, insulin infusion lowers the GH response to GH-releasing hormone via the pituitary [40], suggesting an IGF-1-like effect [41]. In addition, the postoperative GH response in persons with obesity undergoing bariatric surgery seems to be mainly modulated by insulin [21]. GH is also a determinant of lean (muscle) mass after metabolic surgery [42] and exercise training [43]. In this context, the improved insulin and GH levels could be responsible for the increase in muscle lipid oxidation pathways and epigenetic regulation of muscle differentiation, as assessed from Gene Ontology analyses in people with obesity at 52 weeks after bariatric surgery [18]. Despite lack of lean body mass measurements in the present study, the improved muscle differentiation and GH levels after bariatric surgery possibly contribute to preservation of lean mass after surgery as seen with GH treatment during hypocaloric diet [44].
Of note, this study uncovers a direct link between the surgically-induced improvement in GH levels and adipose tissue insulin sensitivity as well as lipid availability. Adipose tissue dysfunction has developed as the key mechanism underlying the pathophysiology of whole-body insulin resistance mediated by lipotoxicity and low-grade inflammation [27, 45, 46]. GH action also targets lipolysis, lipogenesis as well as adipocyte proliferation, differentiation and function, including adipose tissue inflammation and adipokine secretion [47]. A possible mechanism underlying this link may be upregulation of the GH-dependent signal transducer and activator of transcription-5 phosphorylation as shown in skeletal muscle during acute FFA-suppression by acipimox [48], which is mediated by adipocyte JAK2 signaling [49]. Notably, presence of T2D does not seem to play a relevant role for the reversal of the alterations of the GH-IGF-1 axis, as most observed changes were not dependent on T2D status and no association was found between glycemia and GH-IGF-1 changes. This suggests that early metabolic alterations in insulin sensitivity and adipose tissue function rather than overt diabetes and hyperglycemia are linked to changes in the GH system [50].
Furthermore, the adipokine leptin, which signals adipose tissue mass and energy balance to the brain, also inhibits GH secretion [15, 51] and contributes to IGF-1 regulation [16] and could therefore account for the changes in the GH-IGF axis induced by surgical weight loss. While this study confirms the substantial and continuous improvement of hyperleptinemia following metabolic surgery, no relationship was found between the decrease in circulating leptin and the improvement of GH levels. Of note, leptin secretion may be inhibited under conditions of greater insulin sensitivity [52, 53], so that the present results suggest a dissociation between adipose tissue and skeletal muscle insulin sensitivity with regard to leptin control of the GH-IGF-1 axis. Of note, leptin levels remained elevated at 52 weeks after surgery when compared to lean healthy controls, while the circulating GH concentrations at 52 weeks reached those of the nonobese control group. In line with previous reports, the type of metabolic surgery did neither affect change in GH and leptin [22] nor in body weight loss as well as in improvements of hepatic and adipose tissue insulin sensitivity [18].
Finally, IGFBP1 is negatively associated with impaired glucose tolerance [54] and obesity [55] and serves as a marker of HIS [56], while IGFBP3 correlates directly with hepatic insulin resistance and diabetes incidence [57, 58]. Thus, the long-term changes in IGFBP1 and IGFBP3 after metabolic surgery, as seen in the present study, reflect the glucometabolic improvement in line with previous reports [20]. The transient changes in IGFBP1 and IGFBP3 at 2 weeks after surgery and their relationship to changes in FFA and hsCRP point to a previously unknown link between IGFBPs and adipose tissue function and low-grade inflammation in obesity. This may be due to IGF-1-independent effects of IGFBP3 and IGFBP1 on adipose tissue, such as action via type V TGFβ receptors [59, 60].
In conclusion, the present findings provide detailed insights into dynamic endocrine changes in persons with obesity following metabolic surgery by linking reversal of the dysregulation of the GH-IGF-1 axis to adipose tissue metabolism and function. Specifically, these results point to a future role of modulating GH and its mediators in the treatment of obesity and obesity-related disorders.
Data availability
The datasets used and analysed during the current study are available from the corresponding author on reasonable request.
References
Blüher M. Obesity: global epidemiology and pathogenesis. Nat Rev Endocrinol. 2019;15:288–98.
Biondi B. Thyroid and obesity: an intriguing relationship. J Clin Endocrinol Metab. 2010;95:3614–7.
Scacchi M, Pincelli AI, Cavagnini F. Growth hormone in obesity. Int J Obesity Related Metab Disord: J Int Assoc Study Obesity. 1999;23:260–71.
Rasmussen MH, Hvidberg A, Juul A, Main KM, Gotfredsen A, Skakkebaek NE, et al. Massive weight loss restores 24-hour growth hormone release profiles and serum insulin-like growth factor-I levels in obese subjects. J Clin Endocrinol Metab. 1995;80:1407–15.
Perakakis N, Kokkinos A, Peradze N, Tentolouris N, Ghaly W, Pilitsi E, et al. Circulating levels of gastrointestinal hormones in response to the most common types of bariatric surgery and predictive value for weight loss over one year: Evidence from two independent trials. Metab: Clin Exp. 2019;101:153997.
Yu AP, Ugwu FN, Tam BT, Lee PH, Ma V, Pang S, et al. Obestatin and growth hormone reveal the interaction of central obesity and other cardiometabolic risk factors of metabolic syndrome. Sci Rep. 2020;10:5495.
Cordido F, Casanueva FF, Vidal JI, Dieguez C. Study of insulin-like growth factor I in human obesity. Hormone Res. 1991;36:187–91.
Utz AL, Yamamoto A, Sluss P, Breu J, Miller KK. Androgens May Mediate a Relative Preservation of IGF-I Levels in Overweight and Obese Women Despite Reduced Growth Hormone Secretion. J Clin Endocrinol Metab. 2008;93:4033–40.
Juiz-Valiña P, Pena-Bello L, Cordido M, Outeiriño-Blanco E, Pértega S, Varela-Rodriguez B, et al. Altered GH-IGF-1 Axis in Severe Obese Subjects is Reversed after Bariatric Surgery-Induced Weight Loss and Related with Low-Grade Chronic Inflammation. J Clin Med. 2020;9:2614.
Edén Engström B, Burman P, Holdstock C, Ohrvall M, Sundbom M, Karlsson FA. Effects of gastric bypass on the GH/IGF-I axis in severe obesity—and a comparison with GH deficiency. Eur J Endocrinol. 2006;154:53–9.
Ricco RC, Ricco RG, Queluz MC, de Paula MTS, Atique PV, Custódio RJ, et al. IGF-1R mRNA expression is increased in obese children. Growth Hormone IGF Res: Off J Growth Hormone Res Soc Int IGF Res Soc. 2018;39:1–5.
l’Allemand D, Schmidt S, Rousson V, Brabant G, Gasser T, Grüters A. Associations between body mass, leptin, IGF-I and circulating adrenal androgens in children with obesity and premature adrenarche. Eur J Endocrinol. 2002;146:537–43.
Yakar S, Setser J, Zhao H, Stannard B, Haluzik M, Glatt V, et al. Inhibition of growth hormone action improves insulin sensitivity in liver IGF-1-deficient mice. J Clin Investig. 2004;113:96–105.
Haywood NJ, Slater TA, Matthews CJ, Wheatcroft SB. The insulin like growth factor and binding protein family: Novel therapeutic targets in obesity & diabetes. Mol Metab. 2019;19:86–96.
Mingrone G, Manco M, Granato L, Calvani M, Scarfone A, Mora EV, et al. Leptin pulsatility in formerly obese women. FASEB J: Off Publ Feder Am Soc Exp Biol. 2005;19:1380–2.
Chan JL, Williams CJ, Raciti P, Blakeman J, Kelesidis T, Kelesidis I, et al. Leptin does not mediate short-term fasting-induced changes in growth hormone pulsatility but increases IGF-I in leptin deficiency states. J Clin Endocrinol Metab. 2008;93:2819–27.
Beghini M, Brandt S, Körber I, Kohlsdorf K, Vollbach H, Lennerz B, et al. Serum IGF1 and linear growth in children with congenital leptin deficiency before and after leptin substitution. Int J Obesity (2005). 2021;45:1448–56.
Gancheva S, Ouni M, Jelenik T, Koliaki C, Szendroedi J, Toledo FGS, et al. Dynamic changes of muscle insulin sensitivity after metabolic surgery. Nat Commun. 2019;10:4179.
Valera Mora ME, Manco M, Capristo E, Guidone C, Iaconelli A, Gniuli D, et al. Growth hormone and ghrelin secretion in severely obese women before and after bariatric surgery. Obesity (Silver Spring, Md.). 2007;15:2012–8.
Brynskov T, Laugesen CS, Floyd AK, Frystyk J, Sørensen TL. The IGF-Axis and Diabetic Retinopathy Before and After Gastric Bypass Surgery. Obesity Surg. 2017;27:408–15.
De Marinis L, Bianchi A, Mancini A, Gentilella R, Perrelli M, Giampietro A, et al. Growth hormone secretion and leptin in morbid obesity before and after biliopancreatic diversion: relationships with insulin and body composition. J Clin Endocrinol Metab. 2004;89:174–80.
Kruljac I, Mirošević G, Kirigin LS, Nikolić M, Ljubičić N, Budimir I, et al. Changes in metabolic hormones after bariatric surgery and their predictive impact on weight loss. Clin Endocrinol. 2016;85:852–60.
Koliaki C, Szendroedi J, Kaul K, Jelenik T, Nowotny P, Jankowiak F, et al. Adaptation of hepatic mitochondrial function in humans with non-alcoholic fatty liver is lost in steatohepatitis. Cell Metab. 2015;21:739–46.
Faramia J, Hao Z, Mumphrey MB, Townsend RL, Miard S, Carreau AM, et al. IGFBP-2 partly mediates the early metabolic improvements caused by bariatric surgery. Cell Rep Med. 2021;2:100248.
Kwok KHM, Andersson DP, Rydén M, Arner P. A longitudinal study of the antilipolytic effect of insulin in women following bariatric surgery. Int J Obesity. 2021;45:2675–8.
Gastaldelli A, Gaggini M, DeFronzo RA. Role of Adipose Tissue Insulin Resistance in the Natural History of Type 2 Diabetes: Results From the San Antonio Metabolism Study. Diabetes. 2017;66:815–22.
Klein S, Gastaldelli A, Yki-Järvinen H, Scherer PE. Why does obesity cause diabetes? Cell Metab. 2022;34:11–20.
Matsuda M, DeFronzo RA. Insulin sensitivity indices obtained from oral glucose tolerance testing: comparison with the euglycemic insulin clamp. Diabetes Care. 1999;22:1462–70.
Fritsch M, Koliaki C, Livingstone R, Phielix E, Bierwagen A, Meisinger M, et al. Time course of postprandial hepatic phosphorus metabolites in lean, obese, and type 2 diabetes patients. Am J Clin Nutr. 2015;102:1051–8.
Wolf K, Popp A, Schneider A, Breitner S, Hampel R, Rathmann W, et al. Association Between Long-term Exposure to Air Pollution and Biomarkers Related to Insulin Resistance, Subclinical Inflammation, and Adipokines. Diabetes. 2016;65:3314–26.
Herder C, Baumert J, Zierer A, Roden M, Meisinger C, Karakas M, et al. Immunological and cardiometabolic risk factors in the prediction of type 2 diabetes and coronary events: MONICA/KORA Augsburg case-cohort study. PloS ONE. 2011;6:e19852.
Nowotny B, Zahiragic L, Krog D, Nowotny PJ, Herder C, Carstensen M, et al. Mechanisms underlying the onset of oral lipid-induced skeletal muscle insulin resistance in humans. Diabetes. 2013;62:2240–8.
Glad CAM, Svensson PA, Nystrom FH, Jacobson P, Carlsson LMS, Johannsson G, et al. Expression of GHR and Downstream Signaling Genes in Human Adipose Tissue-Relation to Obesity and Weight Change. J Clin Endocrinol Metab. 2019;104:1459–70.
Carlzon D, Svensson J, Petzold M, Karlsson MK, Ljunggren Ö, Tivesten Å, et al. Both low and high serum IGF-1 levels associate with increased risk of cardiovascular events in elderly men. J Clin Endocrinol Metab. 2014;99:E2308–16.
Vottero A, Guzzetti C, Loche S. New aspects of the physiology of the GH-IGF-1 axis. Endocr Dev. 2013;24:96–105.
Al-Regaiey K, Alshubrami S, Al-Beeshi I, Alnasser T, Alwabel A, Al-Beladi H, et al. Effects of gastric sleeve surgery on the serum levels of GH, IGF-1 and IGF-binding protein 2 in healthy obese patients. BMC Gastroenterol. 2020;20:199.
Rajpathak SN, McGinn AP, Strickler HD, Rohan TE, Pollak M, Cappola AR, et al. Insulin-like growth factor-(IGF)-axis, inflammation, and glucose intolerance among older adults. Growth Hormone IGF Res: Off J Growth Hormone Res Soc Int IGF Res Soc. 2008;18:166–73.
Fukushima M, Okamoto Y, Katsumata H, Ishikawa M, Ishii S, Okamoto M, et al. Growth hormone ameliorates adipose dysfunction during oxidative stress and inflammation and improves glucose tolerance in obese mice. Hormone Metab Res = Hormon- und Stoffwechselforschung = Hormones et metabolisme. 2014;46:656–62.
Clasey JL, Weltman A, Patrie J, Weltman JY, Pezzoli S, Bouchard C, et al. Abdominal visceral fat and fasting insulin are important predictors of 24-hour GH release independent of age, gender, and other physiological factors. J Clin Endocrinol Metab. 2001;86:3845–52.
Lanzi R, Manzoni MF, Andreotti AC, Malighetti ME, Bianchi E, Sereni LP, et al. Evidence for an inhibitory effect of physiological levels of insulin on the growth hormone (GH) response to GH-releasing hormone in healthy subjects. J Clin Endocrinol Metab. 1997;82:2239–43.
Melmed S. Insulin suppresses growth hormone secretion by rat pituitary cells. J Clin Investig. 1984;73:1425–33.
Savastano S, Di Somma C, Angrisani L, Orio F, Longobardi S, Lombardi G, et al. Growth hormone treatment prevents loss of lean mass after bariatric surgery in morbidly obese patients: results of a pilot, open, prospective, randomized, controlled study. J Clin Endocrinol Metab. 2009;94:817–26.
Kraemer WJ, Ratamess NA, Hymer WC, Nindl BC, Fragala MS. Growth Hormone(s), Testosterone, Insulin-Like Growth Factors, and Cortisol: Roles and Integration for Cellular Development and Growth With Exercise. Front Endocrinol. 2020;11:33.
Nørrelund H, Børglum J, Jørgensen JO, Richelsen B, Møller N, Nair KS, et al. Effects of growth hormone administration on protein dynamics and substrate metabolism during 4 weeks of dietary restriction in obese women. Clin Endocrinol. 2000;52:305–12.
Roden M, Shulman GI. The integrative biology of type 2 diabetes. Nature. 2019;576:51–60.
Blüher M. Adipose tissue inflammation: a cause or consequence of obesity-related insulin resistance? Clin Sci (London, England: 1979). 2016;130:1603–14.
Berryman DE, Henry B, Hjortebjerg R, List EO, Kopchick JJ. Developments in our understanding of the effects of growth hormone on white adipose tissue from mice: implications to the clinic. Expert Rev Endocrinol Metab. 2016;11:197–207.
Møller N, Gormsen LC, Schmitz O, Lund S, Jørgensen JOL, Jessen N. Free Fatty Acids Inhibit Growth Hormone/Signal Transducer and Activator of Transcription-5 Signaling in Human Muscle: A Potential Feedback Mechanism. Journal Clin Endocrinol Metab. 2009;94:2204–7.
Corbit KC, Camporez JPG, Tran JL, Wilson CG, Lowe DA, Nordstrom SM, et al. Adipocyte JAK2 mediates growth hormone-induced hepatic insulin resistance. JCI Insight. 2017;2:e91001.
Salgin B, Marcovecchio ML, Williams RM, Jackson SJ, Bluck LJ, Humphreys SM, et al. Effects of growth hormone and free fatty acids on insulin sensitivity in patients with type 1 diabetes. J Clin Endocrinol Metab. 2009;94:3297–305.
Casanueva FF, Dieguez C. Neuroendocrine regulation and actions of leptin. Front Neuroendocrinol. 1999;20:317–63.
Wellhoener P, Fruehwald-Schultes B, Kern W, Dantz D, Kerner W, Born J, et al. Glucose metabolism rather than insulin is a main determinant of leptin secretion in humans. J Clin Endocrinol Metab. 2000;85:1267–71.
Mueller WM, Gregoire FM, Stanhope KL, Mobbs CV, Mizuno TM, Warden CH, et al. Evidence that glucose metabolism regulates leptin secretion from cultured rat adipocytes. Endocrinology. 1998;139:551–8.
Sandhu MS, Heald AH, Gibson JM, Cruickshank JK, Dunger DB, Wareham NJ. Circulating concentrations of insulin-like growth factor-I and development of glucose intolerance: a prospective observational study. Lancet (London, England). 2002;359:1740–5.
Frystyk J, Brick DJ, Gerweck AV, Utz AL, Miller KK. Bioactive insulin-like growth factor-I in obesity. J Clin Endocrinol Metab. 2009;94:3093–7.
Kotronen A, Lewitt M, Hall K, Brismar K, Yki-Järvinen H. Insulin-like growth factor binding protein 1 as a novel specific marker of hepatic insulin sensitivity. J Clin Endocrinol Metab. 2008;93:4867–72.
Rajpathak SN, He M, Sun Q, Kaplan RC, Muzumdar R, Rohan TE, et al. Insulin-like growth factor axis and risk of type 2 diabetes in women. Diabetes. 2012;61:2248–54.
Frystyk J, Skjaerbaek C, Vestbo E, Fisker S, Orskov H. Circulating levels of free insulin-like growth factors in obese subjects: the impact of type 2 diabetes. Diabetes/metabolism Res Rev. 1999;15:314–22.
Jogie-Brahim S, Feldman D, Oh Y. Unraveling insulin-like growth factor binding protein-3 actions in human disease. Endocr Rev. 2009;30:417–37.
Wheatcroft SB, Kearney MT. IGF-dependent and IGF-independent actions of IGF-binding protein-1 and -2: implications for metabolic homeostasis. Trends Endocrinol Metab. 2009;20:153–62.
Acknowledgements
We would like to thank all volunteers for their participation in this study and Drs Tomas Jelenik, Chrysi Koliaki, Daniel Markgraf for their important contributions to the clinical examination and/or laboratory assessments as well as Kai Tinnes, Myrko Esser, David Höhn, Andrea Sparla, Kerstin Förster, Fariba Zivehe, Jan-Marc Leonhard, Michelle Reina Do Fundo, Karin Röhrig and Ulrike Partke for their excellent technical assistance.
Funding
This study was supported in part by the German Diabetes Center (DDZ), which is funded by the Ministry of Culture and Science of the State of Northrhine Westphalia and the German Federal Ministry of Health (BMG), by grants of the Federal Ministry for Research (BMBF) to the German Center for Diabetes Research (DZD e. V., DZD Grant 2016). Parts of the study were also supported by grants from the European Funds for Regional Development (EFRE-0400191), the German Research Foundation (DFG, SFB 1116/2, GRK 2576), the German Diabetes Association (DDG), the Schmutzler-Stiftung, the European Community (HORIZON-HLTH-2022-STAYHLTH-02-01: Panel A) to the INTERCEPT-T2D consortium and is receiving funding from the programme “Profilbildung 2020”, an initiative of the Ministry of Culture and Science of the State of Northrhine Westphalia. The sole responsibility for the content of this publication lies with the authors. The funding sources had no role in study design, data collection, data analysis, data interpretation or writing of the report. Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and Affiliations
Contributions
SG performed clinical experiments, collected and analysed data and wrote, edited, and reviewed the paper. SK, KP, TS and JS performed clinical experiments and edited and reviewed the paper. CH performed laboratory analyses and edited and reviewed the paper. KS performed statistical analyses, edited and reviewed the paper. MS performed bariatric surgery procedures and edited and reviewed the paper. MR initiated the investigation, designed and led the clinical experiments and wrote, reviewed and edited the paper. All authors gave final approval of the version to be published. MR is the guarantor of this work and, as such, had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Corresponding author
Ethics declarations
Competing interests
SG, SK, KP, TS, JS, CH, KS and MS declare no competing interests. MR is on scientific advisory boards of Allergan, Astra-Zeneca, Bristol-Myers Squibb, Eli Lilly, Gilead Sciences, Inventiva, Intercept Pharma, Novartis, Novo Nordisk, Servier Laboratories, Target RWE and Terra Firma and has received support for investigator-initiated studies from Boehringer Ingelheim, Nutricia/Danone and Sanofi–Aventis.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Gancheva, S., Kahl, S., Herder, C. et al. Metabolic surgery-induced changes of the growth hormone system relate to improved adipose tissue function. Int J Obes 47, 505–511 (2023). https://doi.org/10.1038/s41366-023-01292-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41366-023-01292-7