Abstract
Background
Increasing physical activity and limiting sedentary time may minimize weight recurrence after bariatric surgery. However, few studies have evaluated potential associations of objectively-measured physical activity and sedentary time with post-surgical weight recurrence over time.
Aims
To evaluate associations of change in physical activity and sedentary time with weight recurrence after bariatric surgery.
Methods
Participants from the Oslo Bariatric Surgery Study, a prospective cohort study, wore an ActiGraph monitor for seven days at 1- and 5 years after surgery to assess daily physical activity and sedentary time. Participants’ weight was measured at in-person clinic visits. Chi-square Test and Paired-samples T-test evaluated group differences and change over time, while Pearson’s Correlation, multiple logistic and linear regression investigated associations between variables.
Results
Five years after surgery 79 participants (70.5% response rate, 81% female) (mean (sd) age: 54.0 (±9.3), BMI: 32.1 (±4.7)) had valid monitor data. Participants increased their sedentary time (71.4 minutes/day (95% CI: 54.2–88.6, p = <0.001)) and reduced daily steps (−1411.1 (95% CI: 737.8–208.4), p = <0.001), light physical activity (−54.1 min/day (95% CI: 40.9–67.2, p = <0.001)), and total physical activity (−48.2 (95% CI: 34.6–63.3), p = <0.001) from 1- to 5 years after surgery. No change was found for moderate-to-vigorous intensity physical activity. No associations were found between changes in steps, physical activity or sedentary time and weight recurrence.
Conclusion
Participants increased sedentary time and decreased light- and total physical activity between 1- and 5 years post-surgery. Overall, changes in physical activity and sedentary time were not associated with weight recurrence. Interventions to help patients increase physical activity and limit sedentary time after bariatric surgery are needed.
Similar content being viewed by others
Introduction
Obesity is a highly prevalent, debilitating, and costly chronic disease [1, 2]. Bariatric surgery is the most effective treatment, and usually results in significant weight reduction, ranging from 25%–35% of initial weight [3, 4], along with improvements of obesity-related diseases [4, 5]. However, 30% of the patients experience weight recurrence up to 23.8% of maximum weight lost, 3–6 years after surgery [6,7,8,9]. This can lead to reemergence of obesity-related comorbidities and health-related quality of life impairments, as well as overall reduced satisfaction with the surgery performed [6,7,8]. Thus, it is important to identify modifiable factors that may prevent or reduce weight recurrence.
Among several factors that predict weight (e.g. metabolism, psychological and somatic issues, and eating habits), physical activity (PA) is a key strategy to enhance weight loss and prevent weight recurrence [10,11,12,13,14,15,16]. First, PA contributes to daily energy expenditure [17, 18]. PA can also help prevent decreases in resting energy expenditure via preservation of lean body mass which usually accounts for ~30% of weight loss following surgery [19]. Further, a recent study found that PA may assist with eating and appetite regulation in bariatric surgery patients [20].
Independent of PA, sedentary time (ST) has been identified as a predictor of mortality related to chronic disease [21]. Efforts to reduce ST among bariatric surgery patients may thus also be important [13]. ST might influence weight recurrence independent of or in conjunction with PA, however these associations have received less attention.
Due to absence of PA guidelines for bariatric surgery patients specifically, patients are often advised to follow national or international guidelines that recommend at least 150 min of moderate-vigorous physical activity (MVPA) (or 75 min of vigorous intensity) per week. Also, sitting more than 6–8 hours per day (h/day) has been related to increased metabolic risk [21], and guidelines recommend both sitting less and replacing time spent sedentary with movement [22].
While patients report changes in PA and ST after surgery, studies show that most patients do not meet recommendations for PA and ST one year after surgery according to objective measures [13, 14, 23, 24]. With subjective measures being prone to recall and other forms of bias, these findings highlight the importance of using objective measures to capture the true PA level and ST in individuals [25,26,27,28,29].
Whether objectively-measured PA and ST change over time beyond the typical weight loss period of 1–2 years [30] is less clear. Bellicha et al. found no changes in neither MVPA nor ST from pre-surgery to 5 years follow-up [31]. Launius et al. [24] found that daily steps and minutes in MVPA increased from surgery to 5 years follow-up [24]. This was supported by the findings of King et al. that showed that mean steps per day was higher at 5- and 7-years compared to pre-surgery. King et al. additionally reported that the percentage of participants meeting PA recommendations and total minutes in MVPA increased the two years following surgery. Despite a decline, these percentages were still higher compared to pre-surgery at 5 years follow-up, but lower compared to pre-surgery at 7-years. No reduction in ST was observed from pre-surgery through 5- and 7-years after surgery [14].
At 5 years, nearly all patients have experienced some amount of weight recurrence [6, 7, 9], thus it is important to look at whether variability in current PA and ST levels relate to the amount of weight recurrence. Few studies have examined this relationship, and even fewer have focused on ST. Bellicha et al. measured PA before, 6 months and 5 years after surgery and found no association between total PA and weight recurrence, but found a negative correlation between MVPA and weight recurrence, 5 years after surgery [31]. Nymo et al. assessed PA and weight recurrence 10–15 years after surgery and found no associations with steps per day, but a negative association between PA duration and weight recurrence [32]. Romagna et al. found that patients who regained less than 20% of initial weight loss had more steps and minutes in MVPA per day and were less sedentary compared to those who experienced ≥20% weight recurrence when both weight and PA was assessed simultaneously ≥5 years after surgery [13]. These findings were supported by King et al. who found that total steps per day and ST, but not MVPA, were associated with weight recurrence when assessed seven years after surgery [14]. If less sitting is associated with less weight recurrence to the same extent as being active, it might be important to focus on motivating patients to reduce ST especially among those who lack motivation or ability to meet PA recommendations.
Since patients on average are shown to make modest improvements in PA 1-year after surgery, and are still losing weight [13, 14, 23], it is important to understand how the magnitude of change in PA from 1-year to 5 years relates to weight recurrence. Studies find that changes in self-reported PA over time may associate more strongly with weight change following surgery, compared to cross-sectional PA [33, 34]. Thus, it is important to understand whether current objectively-measured PA levels and/or the change in PA levels over time matter for weight recurrence.
Weight recurrence may vary according to how MVPA is accumulated. Previous national guidelines recommended that MVPA should be accumulated in bouts of at least 10 min in duration [35]. However, the revised guidelines do not place any restrictions on how MVPA is accumulated [36]. Whether the pattern of MVPA accumulation is important for preventing weight recurrence has previously not been investigated. Also, only evaluating bouted minutes in MVPA might exclude many individuals within the bariatric surgery population because many do not engage in prolonged bouts of MVPA [27]. Importantly, studies within the general population find that using total minutes or bouted minutes in MVPA influence how participants are categorized [37,38,39]. Similar data is not available within the post-bariatric surgery population.
Thus, we aimed to evaluate whether both PA and ST at 5 years and changes in PA and ST from 1- to 5 years post-surgery are associated with weight recurrence 5 years after surgery. Additionally, we sought to investigate changes in objectively-measured PA and ST from 1- to 5 years after bariatric surgery and describe whether frequency of meeting PA recommendations differed based on the use of bouted minutes (≥10 min) or total minutes in MVPA.
Method
Participants and study design
The Oslo Bariatric Surgery Study (OBSS) [40, 41] is a prospective cohort study of patients admitted to bariatric surgery, either Sleeve gastrectomy or Roux-en-Y gastric bypass, at the Center for Morbid Obesity and Bariatric Surgery at Oslo University Hospital, Norway, from 2011 to 2013. The institution is a tertiary referral center for bariatric surgery operating some 300 patients annually. The 1991 National Institutes of Health Consensus Development Conference Statement for indication of bariatric surgery were applied throughout the study period. Clinical follow-up consultations were part of the post-surgery program and scheduled for all patients at 6 months, 1-, 2-, 3-, and 5 years after surgery. As part of the OBSS, objectively-measured PA and ST was investigated at 1- and 5 years after surgery. Recruitment procedure among the OBSS participants for the PA sub-study 1-year after surgery has been described previously [42].
All participants who accepted to wear an ActiGraph 1-year after surgery and returned valid data (N = 112) were eligible to take part in this current 5-year follow-up study. Respondents were invited to medical follow-up (mean (SD) years after surgery was 5.13 (0.34)) and additionally contacted and asked to wear an ActiGraph GT3X+ accelerometer for seven consecutive days after the medical follow-up (mean (SD) years between surgery and use of ActiGraph was 7.88 (0.75)). Data were collected in 2020, during the COVID-19 pandemic.
Measures
Patients reported their age, employment status, educational level, and whether they had a partner or were married. Weight was measured using a calibrated Seca 635 III (0–300 kg) platform scale at follow-up consultations at 1-, 2-, 3-, and 5 years after surgery, with participants wearing light clothing and no shoes. For three participants, self-reported weight pre-surgery was used because objective measured weight was not obtained. Self-reported and objective weight pre-surgery was highly correlated (r = 0.96, p = <0.001), and self-reported values were therefore considered valid for these three individuals. Weight loss from day of surgery to 5 years follow-up was calculated as %TWL = [(Weight on the day of surgery) − (Postoperative Weight)]/(Weight on the day of surgery) × 100 [43], and based on suggested successful weight loss, weight loss was further categorized as ≥20% and <20% of pre-surgery weight [44]. Nadir weight was defined as the lowest postoperative body weight objectively assessed at 1-, 2-, 3- and 5 years after surgery. Weight recurrence was used as a continuous and dichotomous variable, and calculated by 100*(Weight at 5 years follow-up—nadir)/(pre-surgery weight—nadir). Weight recurrence was chosen to be investigated in relation to PA and ST, as it is the weight variable most strongly correlated with cardiometabolic outcomes in bariatric surgery patients [45]. For the same reason as for %TWL, weight recurrence has been recommended to be dichotomized into ≥20% or <20% of maximal weight loss [45]. Body mass index (kg/m2) (BMI) was calculated at the day of surgery and at medical follow-up consultations at 1- and 5 years after surgery.
Objectively-measured physical activity
The ActiGraph GT3X+ activity monitor (ActiGraph, LLC, Pensacola, FL, USA) was used to measure PA and ST. The participants were instructed to wear the accelerometers on their right hip during all waking hours for seven consecutive days, except during showering and bathing. ActiGraph data was included into analyses if containing at least four days with more than 10 h of valid data per day. The accelerometer data was used to assess steps per day, mean counts per minute (cpm), sedentary time (0–99 cpm), light- (100–2019 cmp), moderate- (2020–5998 cpm) vigorous intensity (≥5999 cpm), and total PA (100->5999 cpm) [46, 47], and finally the percentage of the study population that met the current national PA recommendations of at least 150 min of MVPA (or 75 min of vigorous intensity) per week. Adherence to PA recommendations was determined by summing the time spent performing MVPA in two ways. First, we followed the previous guidelines on how to accumulate MVPA minutes which recommended to sum all minutes spent in continuous MVPA in bouts lasting at least 10 min (with allowance for two interruptions) (bouted MVPA) [35]. Second, we followed the 2018 Committee that suggested to sum all minutes spent in MVPA (total minutes in MVPA) [36]. Both guidelines on how to accumulate minutes, recommend a weekly MVPA of at least 150 min, which reflects the international guidelines for healthy adults published by WHO [22]. Regarding ST, both WHO and the Norwegian directory of health recommend to sit less [22, 48]. Furthermore, sitting more than 6–8 h/day has been related to increased metabolic risk [20], and participants were classified according to whether they accumulated 8 h or more of ST per day.
Statistics
Attrition analysis
Logistic regression was used to examine explanatory factors for attrition to the 5-year follow-up study. Among independent variables (age, sex, employment status, education level, relationship status, BMI, weight- and weight loss, and objectively-measured PA and ST, at 1-year after surgery), only BMI and weight correlated with attrition, but showed high intercorrelation (r = >0.8). Hence, only weight 1-year after surgery was included into the regression model.
Statistical analyses
All data were analyzed with IBM SPSS version 26. Descriptive statistics are presented as mean (sd) and sum (%) for continuous and categorical data, respectively. After visually evaluating the data for normality we used a Chi-Square Test to investigate differences in frequency of participants meeting recommendations on PA and ST between 1- and 5 years after surgery. Paired-samples t-test was used to investigate changes in continuous PA and ST data from 1- to 5 years follow-up. Multiple regression analyses were used to control for possible confounders (sex, age, BMI, or time between 5-year medical follow-up and 5-year assessment of PA) on the change in steps, each PA intensity and ST, and investigate predictors for attrition from 1-year to 5 years participation. Prior to the linear regression, Pearson’s correlation was used to investigate correlation between the dependent and independent variables and for multicollinearity between the independent variables. A multiple logistic regression was chosen to investigate group differences in continuous PA and ST data between weight recurrence groups while controlling for possible confounders (age, sex, %TWL at 1-year after surgery, relationship status, employment status, and educational level). The predictive value of each independent variable is presented through Odds Ratio (OR) with 95% confidence intervals (CI). CIs that do not cross the value of 1 represent significance. For other analyses, p-values at ≤0.05 were evaluated as statistically significant. Hypothesis testing analyses were two-sided.
Results
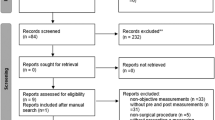
From the 112 participants who returned valid monitor data at 1-year follow-up, and therefore were eligible to be recruited to the 5-year follow-up, 79 (70.5%) participants consented to use the monitor and had four valid days of data at 5 years after surgery (Fig. 1). Among these, 30% at 1-year and 32.9% at 5-year returned monitors without any bouted minutes in MVPA. Attrition analysis found that a higher body weight at 1-year reduced the likelihood of participating at 5 years after surgery (odds ratio: 0.96, 95% CI: 0.93, 0.98).
The flow chart presents the number of individuals who were eligible for the study at 1- and 5-years after surgery, number of individuals reached, number of acceptance and decline, number of excluded individuals, resons for exclusion (boxes to the right-hand side), and final number of included participants in this study.
Demographics
Participant characteristics 5 years after surgery are shown in Table 1. After a reduction in mean (sd) body weight of 36.35 (11.07) kg from the day of surgery to 1-year after surgery, the participants gained a mean (sd) of 6.6 (9.13) kg (p = <0.001) from 1-year to 5 years after surgery. Time-point for nadir weight, reported as mode was at 1-year follow-up (min = 1, max = 5). The majority had lost ≥20% of preoperative weight, and half of the sample had ≥20% weight recurrence 5 years after surgery (Table 1).
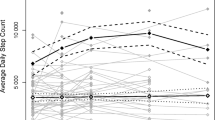
Physical activity and sedentary time 5 years after surgery
At 5 years participants spent on average 79% of waking hours being sedentary, and about 11 and 30 min in bouted MVPA and total minutes in MVPA, respectively (Table 2). Recommendations on PA level and ST were met by 16.5% and 1.3%, respectively (Fig. 2).
Note. Moderate-to-vigorous physical activity: MVPA. MVPA minutes: frequency of participants who meet physical activity (PA) recommendations based on total minutes per day in MVPA; Bouted MVPA minutes: frequency of participants who meet the PA guidelines based on total minutes spent in MVPA bouted in at least 10 min; ST sedentary time. The recommended level of PA according to the Norwegian national guidelines is 150 min objectively-measured [46]. *Significantly different percentage from the percentage meeting PA recommendations based on bouted MVPA. **Significantly different percentage from 1- to 5 years. α = ≤0.05. n = 79.
Changes in physical activity and sedentary time from 1- to 5 years after surgery
Participants increased their time spent sedentary and reduced daily steps, and time in light- and total PA from 1-year to 5 years after surgery (p = <0.001). No changes were found for total minutes in MVPA or bouted MVPA (Table 2). Multiple regression models did not indicate that changes over time were related to confounders such as gender, age, BMI, or time between medical follow-up and use of PA monitor. We found no change in percentage of participants who met PA recommendations based on total minutes in MVPA, while a lower percentage of participants met PA recommendations based on bouted minutes in MVPA at 5 years (16.5%) compared to 1-year (22.8%) after surgery (φ = 0.25, p = 0.028) (Fig. 2). A lower percentage of participants met the threshold recommendations for ST (<8 h per day) (φ = 0.24, p = 0.030) at 5 years (1.3%) compared to 1-year (17.7%) after surgery.
Association between physical activity, sedentary time, and weight recurrence
No significant correlation was found between daily steps (r = −0.12, p = 0.289), different PA intensities (r = −0.21–0.07, p = 0.063–0.698) and ST (r = 0.05, p = 0.640) and weight recurrence at 5 years after surgery (Table 3). Nor did we find any associations between changes in steps (r = −0.12, p = 0.289), PA intensities (r = −0.05–0.11, p = 0.395–0.876) and ST (r = −0.04, p = 0.728) and weight recurrence (Table 4).When controlling for possible confounders, neither daily number of steps, minutes spent in different PA intensities or being sedentary, significantly predicted whether participants experienced ≥20% or <20% weight recurrence at 5 years after surgery (see Supplementary Table 1).
Total minutes in MVPA and minutes in bouted MVPA
When comparing methods of accumulating minutes in MVPA, we found that a higher percentage of participants met PA recommendations when referring to total minutes in MVPA compared to bouted minutes in MVPA (φ = 0.49, 0.28 p = <0.001, 0.014, 1- and 5 years, respectively) (Fig. 2).
Discussion
This is one of the first study to evaluate associations of long-term changes in PA and ST with weight recurrence after bariatric surgery in a Scandinavian patient sample. We found that participants on average did not make favorable changes in PA or ST. Neither PA and ST at 5 years nor changes in PA and ST over time were associated with weight recurrence overall.
Changes in physical activity level and sedentary time
In accordance with previous studies in Brazil, USA, and Sweden [13, 14, 23, 24] we found that participants did not meet PA recommendations and exceeded the suggested threshold (<8 h) for ST one year after surgery. Furthermore, we found that participants on average became even more sedentary, had fewer steps, spent less time in light- and total PA and fewer met MVPA recommendations 5 years after surgery. This reflects a negative trend over time. Our MVPA findings support Bellicha et al. who found no change in MVPA 5 years after surgery [31], contradict the significant increase in steps and minutes in MVPA reported by Launius et al. [24], and partly King et al. who reported a small increase in steps over time, whereas MVPA increased at 5 years which subsequently decreased at 7-years [14].
Our participants increased ST over time in contrast to no change reported by Bellicha et al. and King et al. Intuitively, patients might be expected to increase their PA level and reduce their ST after surgery due to substantial weight loss and improved physical function. However, our findings based on 5-year follow-up data, which align with those from previous studies, do not support this theory. The gap between current recommendations and participants’ PA level and ST reflects an increased risk for chronic disease mortality [21], and poorer overall long-term health [15, 16]. In our sample, the mean difference and the effect size was significantly larger for the increase in ST and reduction in light PA, compared to changes in other PA intensities. Therefore, from a health behavior perspective, it might be most beneficial to intervene on these behaviors if the aim is to comply with PA and ST recommendations. Evidence also suggests that although there is a dose-response relationship between all-cause mortality and PA level, the strongest effect is reported when inactive individuals move towards sitting less and engaging in light intensity activity [49].
Association with weight recurrence
No significant association was found between daily steps or any PA intensity at 5 years or changes in steps and PA intensities over time, with weight recurrence at 5 years after surgery, in our sample. This was also reflected by the lack of difference between weight recurrence groups in steps and PA intensities. This contradicts the negative association found between steps and weight recurrence, but is in line with findings of no association with MVPA, reported by King et al. Our findings related to steps also echoes findings by Nymo et al. but contradicts the negative correlation between PA and weight recurrence ≥5 years after surgery reported by both Bellichia et al. and Nymo et al. [31, 32].
We found no significant association between ST at 5 years or changes in ST over time, with weight recurrence at 5 years after surgery. No difference was neither found between those who experienced ≥20% and <20% weight recurrence. The lack of associations at 5 years contradicts the positive association reported by King et al. in participants 7 years after surgery, however the lack of association when looking at changes in ST over time were similar between the two studies [14]. Because most of our participants exceeded the recommended ST threshold (>8 h), we were statistically not able to investigate group differences related to meeting or not meeting ST recommendations and associations with weight recurrence.
When examining the changes in PA and ST over time, the changes in minutes spent in PA intensities and ST reported in our sample could be too small to have an impact on weight recurrence, and the magnitude of associations might appear different in samples where change over time are more prominent [10,11,12,13, 15, 16]. When interpreting our correlational data, it is important to have in mind that the correlations for both 5 years and changes from 1–5 years are characterized by large 95%CIs, with e.g. r-values ranging from r = −0.2–0.2. This indicates that the sample size might negatively impact the ability to present a precise correlation between variables.
Total minutes in MVPA vs. bouted MVPA
At 5 years after surgery, 72.2% of participants met current MVPA recommendations (≥150 MVPA minutes/week) based on total minutes in MVPA but only 16.5% of participants met previous MVPA recommendations based on bouted MVPA minutes. These data are aligned with findings within the general adult population [37,38,39], but represent novel information on the bariatric surgery population. Choosing the one method over the other clearly decides if our participants are described as a high-risk group for chronic diseases or not, and whether their PA level compares to, or exceeds, the PA level of the general adult population.
Using all minutes in MVPA might be beneficial when evaluating participants following bariatric surgery from several perspectives. Shorter bouts (<10 min) may be more realistic and easily incorporated into the daily life post-surgery, and more clearly reflect movement through an active lifestyle [29]. This activity is not captured with bouted minutes. Also, ~30% of our sample did not participate in any bouted MVPA. Hence, only considering bouted MVPA minutes excludes a large group of participants from being evaluated on an important health-related variable. Namely, using all minutes in MVPA has been found to similarly associate with the metabolic syndrome [39, 50] and cardiometabolic biomarkers when compared to bouted MVPA [51], and could provide equally important information in terms of whether a patient needs to improve MVPA to maintain health.
Strengths and limitations
Among study strengths are: (1) the long-term assessments, (2) the use of objective measures, (3) the additional focus on ST, (4) the investigation of associations between both PA and ST with weight recurrence in a long-term perspective, and (5) the methodological exploration of all minutes in MVPA and bouted minutes in MVPA. Some analyses were most likely underpowered, which indicated that possible group differences and associations related to weight recurrence may have been underestimated. Reported nadir weight depended on weight assessed at time-specific clinical follow-ups, and could therefore differ slightly from the true nadir weight experienced in-between follow-ups. Due to only one sleeve gastrectomy patient, we could not evaluate if results differed by surgery procedure. Also, in accordance with most bariatric surgery studies, our results mainly reflect the female population. Finally, data were collected during the COVID-19 pandemic which could impact our findings since social isolation during the pandemic associated with less PA activity and more ST among previous bariatric surgery patients [52].
Research and practical implications
For the average patient, improvement of PA and a reduction in ST is beneficial for promoting health and weight related benefits of the surgery. Focusing on replacing ST with light PA activity might be more acceptable and easier initially for some patients than to mainly focus on an increase in MVPA. An additional encouragement to increase MVPA to achieve larger increases in overall daily movement as per national guidelines is important. Future research should focus on both long-term PA level and ST within a larger sample size to improve our understanding of their combined and separate influence on weight recurrence. Interventions to help bariatric surgery patients increase PA and limit ST for overall health are needed. However, to better evaluate whether changes in PA and ST influence weight recurrence, randomized controlled trials, in which true changes in behaviors are observed and possible confounders are controlled for, are needed [53]. It might be appropriate to suggest an additional focus on all minutes in MVPA to include all participants and to evaluate PA more appropriately among this specific population.
Conclusion
In this study the participants were overall less active and more sedentary at 5 years compared to 1-year after bariatric surgery. No statistically significant associations were observed between continuous measures of PA and ST and weight recurrence.
Data availability
The dataset analyzed during the current study is available from the corresponding author on reasonable request.
References
Gastroenterology TL. Aanother ongoing pandemic. Lancet. 2021;6:1.
OECD. The Heavy Burden of Obesity: The Economics of Prevention. OECD Health Policy Studies. Paris: Publishing; 2019.
Courcoulas AP, Christian NJ, Belle SH, Berk PD, Flum DR, Garcia L, et al. Weight change and health outcomes at 3 years after bariatric surgery among individuals with severe obesity. JAMA. 2013;310:2416–25.
Adams TD, Davidson LE, Litwin SE, Kolotkin RL, LaMonte MJ, Pendleton RC, et al. Health benefits of gastric bypass surgery after 6 years. JAMA. 2012;308:1122–31.
Gloy VL, Briel M, Bhatt DL, Kashyap SR, Schauer PR, Mingrone G, et al. Bariatric surgery versus non-surgical treatment for obesity: a systematic review and meta-analysis of randomised controlled trials. BMJ. 2013;347:1–16.
Adams TD, Davidson LE, Litwin SE, Kim J, Kolotkin RL, Nanjee MN, et al. Weight and metabolic outcomes 12 years after gastric bypass. N Engl J Med. 2017;377:1143–55.
Courcoulas AP, King WC, Belle SH, Berk P, Flum DR, Garcia L, et al. Seven-year weight trajectories and health outcomes in the Longitudinal Assessment of Bariatric Surgery (LABS) study. JAMA Surg. 2018;153:427–34.
Voorwinde V, Steenhuis IH, Janssen I, Monpellier VM, van Stralen MM. Definitions of long-term weight regain and their associations with clinical outcomes. Obes Surg. 2020;30:527–36.
King WC, Hinerman AS, Courcoulas AP. Weight regain after bariatric surgery: a systematic literature review and comparison across studies using a large reference sample. Surg Obes Relat Dis. 2020;16:1133–44.
Herman KM, Carver TE, Christou NV, Andersen RE. Keeping the weight off: physical activity, sitting time, and weight loss maintenance in bariatric surgery patients 2 to 16 years postsurgery. Obes Surg. 2014;24:1064–72.
Steinfeld B, Scott J, Vilander G, Marx L, Quirk M, Lindberg J, et al. The role of lean process improvement in implementation of evidence-based practices in behavioral health care. Jf Behav Health Ser Res. 2015;42:504–18.
Tettero OM, Aronson T, Wolf RJ, Nuijten MA, Hopman MT, Janssen I. Increase in physical activity after bariatric surgery demonstrates improvement in weight loss and cardiorespiratory fitness. Obes Surg. 2018;28:3950–7.
Romagna EC, Lopes KG, Mattos DMF, Farinatti P, Kraemer-Aguiar LG. Physical activity level, sedentary time, and weight regain after bariatric surgery in patients without regular medical follow-up: a cross-sectional study. Obes Surg. 2021;31:1705–13.
King WC, Hinerman AS, White GE, Courcoulas AP, Saad MAB, Belle SH. Associations Between Physical Activity and Changes in Weight Across 7 Years After Roux-en-Y Gastric Bypass Surgery: A Multicenter Prospective Cohort Study. Ann Surg. 2022;275:718–26.
Santos C, Carvalho M, Oliveira L, Palmeira A, Rodrigues LM, Gregório J. The Long-Term Association between Physical Activity and Weight Regain, Metabolic Risk Factors, Quality of Life and Sleep after Bariatric Surgery. Int J Environ Res Public Health. 2022;19:8328.
King WC, Hinerman AS, White GE, Courcoulas AP, Belle SH. Associations between physical activity and changes in depressive symptoms and health-related quality of life across 7 years following Roux-en-Y gastric bypass surgery: a multicenter prospective cohort study. Ann Surg. 2022;276:e777–83.
Jakicic JM. The effect of physical activity on body weight. Obesity. 2009;17:34–8.
Goodpaster BH, DeLany JP, Otto AD, Kuller L, Vockley J, South-Paul JE, et al. Effects of diet and physical activity interventions on weight loss and cardiometabolic risk factors in severely obese adults: a randomized trial. JAMA. 2010;304:1795–802.
Chaston TB, Dixon J, O’Brien PE. Changes in fat-free mass during significant weight loss: a systematic review. Int J Obes. 2007;31:743–50.
Bond DS, Smith KE, Schumacher LM, Vithiananthan S, Jones DB, Webster J, et al. Associations of physical activity and sedentary behavior with appetite sensations and eating regulation behaviors before and during the initial year following bariatric surgery. Obes Sci Pract. 2022;8:164–75.
Patterson R, McNamara E, Tainio M, de Sá TH, Smith AD, Sharp SJ, et al. Sedentary behaviour and risk of all-cause, cardiovascular and cancer mortality, and incident type 2 diabetes: a systematic review and dose response meta-analysis. Eur J Epidemiol. 2018;33:811–29.
Bull FC, Al-Ansari SS, Biddle S, Borodulin K, Buman MP, Cardon G, et al. World Health Organization 2020 guidelines on physical activity and sedentary behaviour. Br J Sports Med. 2020;54:1451–62.
Berglind D, Willmer M, Eriksson U, Thorell A, Sundbom M, Uddén J, et al. Longitudinal assessment of physical activity in women undergoing Roux-en-Y gastric bypass. Obes Surg. 2015;25:119–25.
Launius KN, Herb Neff KM, Schuh LM, Saules KK, Creel DB, Inman MM. Long-term Engagement in Physical Activity Among Bariatric Surgery Patients: Associations with Treatment Outcomes at 5-Year Follow-up. Obes Surg. 2022;33:1–9.
Berglind D, Willmer M, Tynelius P, Ghaderi A, Näslund E, Rasmussen F. Accelerometer-measured versus self-reported physical activity levels and sedentary behavior in women before and 9 months after Roux-en-Y gastric bypass. Obes Surg. 2016;26:1463–70.
Kuipers E, Timmerman J, van Det M, Vollenbroek-Hutten M. The Need for Objective Physical Activity Measurements in Routine Bariatric Care. Obes Surg. 2022;32:2975–86.
Bergh I, Kvalem IL, Mala T, Hansen BH, Sniehotta FF. Predictors of physical activity after gastric bypass—a prospective study. Obes Surg. 2017;27:2050–7.
Possmark S, Sellberg F, Willmer M, Tynelius P, Persson M, Berglind D. Accelerometer-measured versus self-reported physical activity levels in women before and up to 48 months after Roux-en-Y Gastric Bypass. BMC Surg. 2020;20:1–10.
Strath SJ, Holleman RG, Richardson CR, Ronis DL, Swartz AM. Peer reviewed: objective physical activity accumulation in bouts and nonbouts and relation to markers of obesity in US adults. Prev Chronic Dis. 2008;5:A131.
Higa K, Ho T, Tercero F, Yunus T, Boone KB. Laparoscopic Roux-en-Y gastric bypass: 10-year follow-up. Surg Obes Relat Dis. 2011;7:516–25.
Bellicha A, Ciangura C, Roda C, Torcivia A, Aron-Wisnewsky J, Poitou C, et al. Effect of exercise training after bariatric surgery: A 5-year follow-up study of a randomized controlled trial. PLoS ONE. 2022;17:e0271561.
Nymo S, Lundanes J, Aukan M, Sandvik J, Johnsen G, Græslie H, et al. Diet and physical activity are associated with suboptimal weight loss and weight regain 10–15 years after Roux-en-Y gastric bypass: A cross-sectional study. Obes Res Clin Pract. 2022;16:163–9.
Monpellier VM, Janssen IM, Antoniou EE, Jansen AT. Weight change after Roux-en Y gastric bypass, physical activity and eating style: is there a relationship? Obes Surg. 2019;29:526–33.
Voorwinde V, Hoekstra T, Monpellier VM, Steenhuis IH, Janssen IM, van Stralen MM. Five-year weight loss, physical activity, and eating style trajectories after bariatric surgery. Surg Obes Relat Dis. 2022;18:911–8.
HHS. 2008 Physical activity guidelines for Americans. In: Services DoHaH, editor. Hyattsville, MD: Author, Washington, DC. Washington DC U.S: US Dept of Health and Human Services; 2008. p. 1–40.
HHS. 2018 Physical Activity Guidelines Advisory Committee Scientific Report. Washington, DC: U.S., Services DoHaH; 2018.
Arigo D, Mogle JA, Brown MM, Roberts SR, Pasko K, Butryn ML, et al. Differences between accelerometer cut point methods among midlife women with cardiovascular risk markers. Menopause. 2020;27:559–67.
Clarke J, Colley R, Janssen I, Tremblay MS. Accelerometer-measured moderate-to vigorous physical activity of Canadian adults, 2007 to 2017. Health Rep. 2019;30:3–10.
Glazer NL, Lyass A, Esliger DW, Blease SJ, Freedson PS, Massaro JM, et al. Sustained and shorter bouts of physical activity are related to cardiovascular health. Med Sci Sports Exerc. 2013;45:109–15.
Kvalem IL, Bergh I, von Soest T, Rosenvinge JH, Johnsen TA, Martinsen EW, et al. A comparison of behavioral and psychological characteristics of patients opting for surgical and conservative treatment for morbid obesity. BMC Obesity. 2015;3:1–11.
Bergh I, Kvalem IL, Risstad H, Cameron LD, Sniehotta FF. Predictors of preoperative weight loss in morbidly obese adults waiting for bariatric surgery: a prospective cohort study. Obes Surg. 2015;25:1610–7.
Bergh I, Kvalem IL, Risstad H, Sniehotta FF. Preoperative predictors of adherence to dietary and physical activity recommendations and weight loss one year after surgery. Surg Obes Relat Dis. 2016;12:910–8.
Brethauer SA, Kim J, El Chaar M, Papasavas P, Eisenberg D, Rogers A, et al. Standardized outcomes reporting in metabolic and bariatric surgery. Obes Surg. 2015;25:587–606.
Grover BT, Morell MC, Kothari SN, Borgert AJ, Kallies KJ, Baker MT. Defining weight loss after bariatric surgery: a call for standardization. Obes Surg. 2019;29:3493–9.
King WC, Hinerman AS, Belle SH, Wahed AS, Courcoulas AP. Comparison of the performance of common measures of weight regain after bariatric surgery for association with clinical outcomes. JAMA. 2018;320:1560–9.
Hansen BH, Kolle E, Dyrstad SM, Holme I, Anderssen SA. Accelerometer-determined physical activity in adults and older people. Med Sci Sports Exerc. 2012;44:266–72.
Troiano RP, Berrigan D, Dodd KW, Masse LC, Tilert T, McDowell M. Physical activity in the United States measured by accelerometer. Med Sci Sports Exerc. 2008;40:181.
NNR. Nordic Nutrition Recommendations 2012: Integrating nutrition and physical activity. Copenhagen: Nordic Council of Ministers; 2014. p. 1–627.
Ekelund U, Dalene KE, Tarp J, Lee I-M. Physical activity and mortality: what is the dose response and how big is the effect? Br J Sports Med. 2020;54:1–12.
Clarke J, Janssen I. Sporadic and bouted physical activity and the metabolic syndrome in adults. Med Sci Sports Exerc. 2014;46:76–83.
Wolff-Hughes DL, Fitzhugh EC, Bassett DR, Churilla JR. Total activity counts and bouted minutes of moderate-to-vigorous physical activity: relationships with cardiometabolic biomarkers using 2003–2006 NHANES. J Phys Act Health. 2015;12:694–700.
Rezende DA, Pinto AJ, Goessler KF, Nicoletti CF, Sieczkowska SM, Meireles K, et al. Influence of adherence to social distancing due to the COVID-19 pandemic on physical activity level in post-bariatric patients. Obes Surg. 2021;31:1372–5.
Bond DS, Manuel KM, Wu Y, Livingston J, Papasavas P, Baillot A, et al. Exercise for counteracting weight recurrence after bariatric surgery: a systematic review and meta-analysis of randomized controlled trials. Surg Obes Relat Dis. 2022:1–10.
Acknowledgements
We are thankful for the help given by personnel at Center for Morbid Obesity and Bariatric Surgery, Oslo University Hospital in the assistance with the recruitment process. A big thanks to Jon A. Kristinsson for taking part in the study development and Marianne Sæter for all your help related to data retrieval. We would also like to thank all participants for their contribution to this study.
Funding
CSB’s Post-doc position is funded by South-Eastern Norway Regional Health Authority.
Author information
Authors and Affiliations
Contributions
The overall OBSS study is managed by TM and coordinated by ILK. The current sub-study is led by ØR. CSB, TM, ILK, and IB were involved in the data collection, and BHH was in charge of the ActiGraph data processing. CSB conducted the statistical analyses and drafted the paper. All authors have made essential contributions to the paper structure, interpretation of the analyses, and revisions of the paper. All authors have read and approved the final paper.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval
All participants received oral and written information about the project. Written consent was obtained prior to participating in the study, and participants were required to give specific consent regarding collecting data from their medical records. Separate consent was obtained for wearing the ActiGraph. The study was approved by REK South East (REK2009/1248) and The Norwegian Data Protection Authority at Oslo University Hospital.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Sundgot-Borgen, C., Bond, D.S., Sniehotta, F.F. et al. Associations of changes in physical activity and sedentary time with weight recurrence after bariatric surgery: a 5-year prospective study. Int J Obes 47, 463–470 (2023). https://doi.org/10.1038/s41366-023-01284-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41366-023-01284-7
This article is cited by
-
Do patients with obesity undergoing bariatric surgery modify their objectively measured physical activity? A systematic review and meta-analysis
International Journal of Obesity (2024)
-
Prevalence of Perceived Barriers to Physical Activity Among Pre- and Post-Metabolic and Bariatric Surgery Patients: A Cross-Sectional Study
Obesity Surgery (2024)