Abstract
Background
Rapid growth and excess weight in early childhood are associated with obesity risk. While maternal preconception BMI has been identified as a potential risk factor, the role of paternal preconception BMI is less clear.
Objectives
To examine the association between paternal preconception BMI and age- and sex-standardized WHO BMI z-score (zBMI) growth rates, zBMI, and weight status, in 0- to 10-year-old children. To determine whether these associations differed by child sex and maternal preconception weight status.
Methods
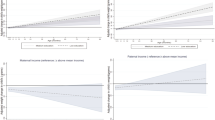
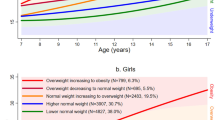
A longitudinal cohort study was conducted through The Applied Research Group for Kids (TARGet Kids!). Children (n = 218) underwent repeated measures of height and weight from birth to 10 years old. Piecewise linear mixed models were used to assess the association between paternal preconception BMI and child zBMI growth rates (zBMI SD units/month) between 0, 4, 30, 48 and 120 months of age. Linear mixed models were used to examine the association with child zBMI, and logistic generalized estimation equations (GEE) were used to assess the association with child weight status. Child sex and maternal preconception weight status were tested as effect modifiers.
Results
Paternal preconception BMI was associated with child zBMI growth rate, mean zBMI and weight status in boys, but not girls. A 5 kg/m2 higher paternal preconception BMI was associated with approximately 0.01 zBMI SD unit/month higher growth rate for boys born to mothers with preconception overweight. Higher paternal BMI was associated with higher mean zBMI and increased odds of overweight and obesity in boys, with greater effects seen when mothers had preconception overweight compared to normal weight.
Conclusion
Paternal preconception BMI was associated with child zBMI growth rate, zBMI and weight status in boys, with greater effects when the biological mother had preconception overweight or obesity. Further understanding of sex differences in paternal preconception weight effects in children is needed.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
Data availability
The datasets generated during and/or analyzed during the current study are not publicly available as we do not have REB approval for data sharing.
References
Wiacek M, Zubrzycki IZ, Tomasiuk R. worldwide obesity trends: an analysis of WHO data. J Obes Body Weight. 2021;2:005.
Di Cesare M, Sorić M, Bovet P, Miranda JJ, Bhutta Z, Stevens GA, et al. The epidemiological burden of obesity in childhood: A worldwide epidemic requiring urgent action. BMC Med. 2019;17:1–20.
Hoffman DJ, Reynolds RM, Hardy DB. Developmental origins of health and disease: current knowledge and potential mechanisms. Nutr Rev. 2017;75:951–70.
Heslehurst N, Vieira R, Akhter Z, Bailey H, Slack E, Ngongalah L, et al. The association between maternal body mass index and child obesity: A systematic review and meta-analysis. PLoS Med. 2019;16:1–20. https://doi.org/10.1371/journal.pmed.1002817.
Voerman E, Santos S, Golab BP, Amiano P, Ballester F, Barros H, et al. Maternal body mass index, gestational weight gain, and the risk of overweight and obesity across childhood: an individual participant data meta-analysis. PLoS Med. 2019;16:1–22.
Yu Z, Han S, Zhu J, Sun X, Ji C, Guo X. Pre-pregnancy body mass index in relation to infant birth weight and offspring overweight/obesity: a systematic review and meta-analysis. PLoS ONE. 2013;8:e61627.
Campbell JM, Lane M, Owens JA, Bakos HW. Paternal obesity negatively affects male fertility and assisted reproduction outcomes: a systematic review and meta-analysis. Reprod Biomed Online. 2015;31:593–604.
Campbell JM, McPherson NO. Influence of increased paternal BMI on pregnancy and child health outcomes independent of maternal effects: a systematic review and meta-analysis. Obes Res Clin Pract. 2019;13:511–21.
Oldereid NB, Wennerholm UB, Pinborg A, Loft A, Laivuori H, Petzold M, et al. The effect of paternal factors on perinatal and paediatric outcomes: A systematic review and meta-analysis. Hum Reprod Update. 2018;24:320–89.
Fleten C, Nystad W, Stigum H, Skjaerven R, Lawlor DA, Davey Smith G, et al. Parent-offspring body mass index associations in the Norwegian Mother and Child Cohort Study: a family-based approach to studying the role of the intrauterine environment in childhood adiposity. Am J Epidemiol. 2012;176:83–92.
Jääskeläinen A, Pussinen J, Nuutinen O, Schwab U, Pirkola J, Kolehmainen M, et al. Intergenerational transmission of overweight among Finnish adolescents and their parents: a 16-year follow-up study. Int J Obes. 2011;35:1289–94.
Lawlor DA, Smith GD, O’Callaghan M, Alati R, Mamun AA, Williams GM, et al. Epidemiologic evidence for the fetal overnutrition hypothesis: Findings from the Mater-University study of pregnancy and its outcomes. Am J Epidemiol. 2007;165:418–24.
Reilly JJ, Armstrong J, Dorosty AR, Emmett PM, Ness A, Rogers I, et al. Early life risk factors for obesity in childhood: cohort study. Br Med J. 2005;330:1357–9.
Sharp GC, Lawlor DA, Richardson SS. It’s the mother!: how assumptions about the causal primacy of maternal effects influence research on the developmental origins of health and disease. Soc Sci Med. 2018;213:20–7.
Durmus B, Kruithof CJ, Gillman MH, Willemsen SP, Hofman A, Raat H. et al. Parental smoking during pregnancy, early growth, and risk of obesity in preschool children: the Generation R Study 1-3. Am J Clin Nutr. 2011;94:164–71. https://academic.oup.com/ajcn/article/94/1/164/4597774.
Regnault N, Botton J, Forhan A, Hankard R, Thiebaugeorges O, Hillier TA, et al. Determinants of early ponderal and statural growth in full-term infants in the EDEN mother-child cohort study. Am J Clin Nutr. 2010;92:594–602.
Halilagic A, Moschonis G. The effect of growth rate during infancy on the risk of developing obesity in childhood: a systematic literature review. Nutrients. 2021;13:3449. https://pubmed.ncbi.nlm.nih.gov/34684450/.
Koletzko B. Early nutrition and its later consequences: new opportunities. Adv Exp Med Biol.2005;569:1–12. https://pubmed.ncbi.nlm.nih.gov/16137099/.
Rath SR, Marsh JA, Newnham JP, Zhu K, Atkinson HC, Mountain J, et al. Parental pre-pregnancy BMI is a dominant early-life risk factor influencing BMI of offspring in adulthood. Obes Sci Pract. 2016;2:48–57.
Zalbahar N, Jan Mohamed HJB, Loy SL, Najman J, McIntyre HD, Mamun A. Association of parental body mass index before pregnancy on infant growth and body composition: Evidence from a pregnancy cohort study in Malaysia. Obes Res Clin Pract. 2016;10:S35–47. https://doi.org/10.1016/j.orcp.2015.08.002.
Aris IM, Bernard JY, Chen L-W, Tint MT, Pang WW, Soh SE, et al. Modifiable risk factors in the first 1000 days for subsequent risk of childhood overweight in an Asian cohort: significance of parental overweight status. Int J Obes. 2018;42:44–51.
Durmuş B, Arends LR, Ay L, Hokken-Koelega AC, Raat H, Hofman A, et al. Parental anthropometrics, early growth and the risk of overweight in pre-school children: the Generation R study. Pediatr Obes. 2013;8:339–50.
Sørensen TIA, Ajslev TA, Ängquist L, Morgen CS, Ciuchi IG, Smith GD. Comparison of associations of maternal peri-pregnancy and paternal anthropometrics with child anthropometrics from birth through age 7 y assessed in the Danish National Birth Cohort. Am J Clin Nutr. 2016;104:389–96.
Carsley S, Borkhoff CM, Maguire JL, Birken CS, Khovratovich M, McCrindle B, et al. Cohort profile: the Applied Research Group for Kids (TARGet Kids!). Int J Epidemiol. 2015;44:776–88.
Linabery AM, Nahhas RW, Johnson W, Choh AC, Towne B, Odegaard AO, et al. Stronger influence of maternal than paternal obesity on infant and early childhood BMI: the Fels Longitudinal Study. Pediatr Obes. 2013;8:159–69.
Eny KM, Chen S, Anderson LN, Chen Y, Lebovic G, Pullenayegum E, et al. Breastfeeding duration, maternal body mass index, and birth weight are associated with differences in body mass index growth trajectories in early childhood. Am J Clin Nutr. 2018;107:584–92.
Deveci AC, Keown‐Stoneman CDG, Maguire JL, O’Connor DL, Anderson LN, Dennis C, et al. Maternal BMI in the preconception period, and association with child zBMI growth rates. Pediatr Obes. 2022. https://pubmed-ncbi-nlm-nih-gov.myaccess.library.utoronto.ca/36573480/.
NHANES III (1988-1994) - Anthropometric procedure videos. 2021. https://wwwn.cdc.gov/nchs/nhanes/nhanes3/anthropometricvideos.aspx.
Carsley S, Parkin PC, Tu K, Pullenayegum E, Persaud N, Maguire JL, et al. Reliability of routinely collected anthropometric measurements in primary care. BMC Med Res Methodol. 2019;19:84.
de Onis M, Garza C, Victora C. The WHO Multicentre Growth Reference Study: strategy for developing a new international growth reference. Forum Nutr.2003;56:238–40. https://pubmed.ncbi.nlm.nih.gov/15806880.
Secker D, Armistead C.Dietitians of Canada, Canadian Paediatric Society, College of Family Physicians of Canada, Community Health Nurses of Canada et al. Promoting optimal monitoring of child growth in Canada: Using the new World Health Organization growth charts. Paediatr Child Health.2010;15:77–9. https://pubmed.ncbi.nlm.nih.gov/21815309/.
Dietitians of Canada, Canadian Paediatric Society, College of Family Physicians of Canada, Community Health Nurses of Canada, Secker D. Promoting optimal monitoring of child growth in Canada: using the new WHO growth charts. Can J Diet Pract Res. 2010;71. https://pubmed.ncbi.nlm.nih.gov/21815309/.
Howe LD, Tilling K, Matijasevich A, Petherick ES, Santos AC, Fairley L, et al. Linear spline multilevel models for summarising childhood growth trajectories: a guide to their application using examples from five birth cohorts. Stat Methods Med Res. 2016;25:1854–74.
Canadian Community Health Survey - Canada.ca. 2021. https://www.canada.ca/en/health-canada/services/food-nutrition/food-nutrition-surveillance/health-nutrition-surveys/canadian-community-health-survey-cchs.html.
Caprio S, Daniels SR, Drewnowski A, Kaufman FR, Palinkas LA, Rosenbloom AL, et al. Influence of race, ethnicity, and culture on childhood obesity: implications for prevention and treatment A consensus statement of Shaping America’s Health and the Obesity Society. Diabetes Care. 2008;31:2211–21.
Taveras EM, Gillman MW, Kleinman K, Rich-Edwards JW, Rifas-Shiman SL. Racial/ethnic differences in early-life risk factors for childhood obesity. Pediatrics. 2010;125:686–95.
Anderson LN, Fatima T, Shah B, Smith BT, Fuller AE, Borkhoff CM, et al. Income and neighbourhood deprivation in relation to obesity in urban dwelling children 0-12 years of age: a cross-sectional study from 2013 to 2019. J Epidemiol Community Health. 2021;0:1–7. http://jech.bmj.com/.
Danielzik S, Langnäse K, Mast M, Spethmann C, Müller MJ. Impact of parental BMI on the manifestation of overweight 5-7 year old children. Eur J Nutr. 2002;41:132–8.
Obesity and overweight. 2019 https://www.who.int/en/news-room/fact-sheets/detail/obesity-and-overweight.
De Onis M, Garza C, Victora CG, Onyango AW, Frongillo EA, Martines J. The WHO Multicentre Growth Reference Study: planning, study design, and methodology. Food Nutr Bull.2004;25:S15–26. https://pubmed.ncbi.nlm.nih.gov/15069916/.
De Onis M, Onyango AW, Borghi E, Siyam A, Nishida C, Siekmann J. Development of a WHO growth reference for school-aged children and adolescents. Bull World Health Organ.2007;85:660–7. https://pubmed.ncbi.nlm.nih.gov/18026621/.
Harrell FE. Regression modeling strategies with applications to linear models, logistic and ordinal regression, and survival analysis. in: regression modeling strategies with applications to linear models, logistic and ordinal regression, and survival analysis. 2nd ed. Springer; 2015. http://www.springer.com/series/692.
van Buuren S, Groothuis-Oudshoorn K. mice: Multivariate imputation by chained equations in R. J Stat Softw.2011;45:1–67. https://www.jstatsoft.org/index.php/jss/article/view/v045i03/v45i03.pdf.
R Core Team (2020). R: a language and environment for statistical computing. Vienna, Austria: R Foundation for Statistical Computing. https://www.R-project.org/.
Piechowski-Jozwiak B, Bogousslavsky J. Couvade syndrome - custom, behavior or disease? Front Neurol Neurosci. 2017;42:51–8.
Scherdel P, Botton J, Rolland-Cachera MF, Léger J, Pelé F, Ancel PY. et al. Should the WHO growth charts be used in france?. PLoS ONE.2015;10:e0120806 https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0120806.
Wright C, Lakshman R, Emmett P, Ong KK. Implications of adopting the WHO 2006 Child Growth Standard in the UK: two prospective cohort studies. Arch Dis Child. 2008;93:566–9.
Júlíusson PB, Roelants M, Hoppenbrouwers K, Hauspie R, Bjerknes R. Growth of Belgian and Norwegian children compared to the WHO growth standards: prevalence below -2 and above +2 SD and the effect of breastfeeding. Arch Dis Child.2011;96:916–21. https://pubmed.ncbi.nlm.nih.gov/19948662/.
Roelants M, Hauspie R, Hoppenbrouwers K. Breastfeeding, growth and growth standards: performance of the WHO growth standards for monitoring growth of Belgian children. Ann Hum Biol .2010;37:129–30. https://pubmed.ncbi.nlm.nih.gov/19968593/.
Rolland-Cachera MF, Péneau S. Assessment of growth: variations according to references and growth parameters used. Am J Clin Nutr. 2011;94. https://pubmed.ncbi.nlm.nih.gov/21525200/.
Van Dijk CE, Innis SM. Growth-curve standards and the assessment of early excess weight gain in infancy. Pediatrics.2009;123:102–8. https://pubmed.ncbi.nlm.nih.gov/19117867/.
Chen Y-P, Xiao X-M, Li J, Reichetzeder C, Wang Z-N, Hocher B. Paternal Body Mass Index (BMI) is associated with offspring intrauterine growth in a gender dependent manner. www.plosone.org.
Hansen PJ, Dobbs KB, Denicol AC, Siqueira LGB. Sex and the preimplantation embryo - implications of sexual dimorphism in the preimplantation period for maternal programming of embryonic development. Cell Tissue Res. 2016;363:237.
Billah MM, Khatiwada S, Morris MJ, Maloney CA. Effects of paternal overnutrition and interventions on future generations. Int J Obes.2022;46:901–17. https://www.nature.com/articles/s41366-021-01042-7.
Emmott EH, Mace R. Why the son-bias in caregiving? Testing sex-differences in the associations between paternal caregiving and child outcomes in England. J Fam Issues. 2021;42:1354–83. https://doi.org/10.1177/0192513X20941902.
Tu Y-K, Tilling K, Sterne JAC, Gilthorpe MS. A critical evaluation of statistical approaches to examining the role of growth trajectories in the developmental origins of health and disease. Int J Epidemiol.2013;42:1327–39. https://pubmed.ncbi.nlm.nih.gov/24038715/.
Tilling K, MacDonald-Wallis C, Lawlor DA, Hughes RA, Howe LD. Modelling childhood growth using fractional polynomials and linear splines. Ann Nutr Metab. 2014;65:129–38.
Nagin DS, Odgers CL. Group-based trajectory modeling in clinical research. Annu Rev Clin Psychol. 2010;6:109–38. https://www.annualreviews.org/doi/abs/10.1146/annurev.clinpsy.121208.131413.
Author information
Authors and Affiliations
Consortia
Contributions
JLM, and CSB: designed and led the TARGet Kids! cohort study; LNA led TARGet Kids! cohort study; ACD, CKS, DLO, JLM, CLD, and CSB: designed the present analysis; ACD and CKS: analyzed the data; ACD and CSB: wrote the manuscript; CSB: had primary responsibility for final content. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
COMPETING INTERESTS
CSB reported receiving research funding from the Canadian Institute for Health Research, Heart and Stroke Foundation of Canada, Physician Services Inc, The Edwin S.H. Leong Centre for Healthy Children, University of Toronto and Hospital for Sick Children, Centre for Addictions and Mental Health, Ontario Child Health Support Unit (OCHSU) Impact Child Health Award, and a Walmart Community Grant through the SickKids Foundation for a study on food insecurity in the inpatient hospital setting. The other authors had no conflicts of interest relevant to this article to disclose. The funding agencies had no role in the design and conduct of the study, the collection, management, analysis and interpretation of the data, or the preparation, review and approval of the manuscript.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
A list of members and their affiliations appears at the end of the paper.
A full list of members and their affiliations appears in the Supplementary Information.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Deveci, A.C., Keown-Stoneman, C.D.G., Maguire, J.L. et al. Paternal BMI in the preconception period, and the association with child zBMI. Int J Obes 47, 280–287 (2023). https://doi.org/10.1038/s41366-023-01261-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41366-023-01261-0