Abstract
Background
The main purpose of the study is to assess the association between obstructive sleep apnea (OSA) and insulin secretion in children with obesity.
Methods
We enrolled children and adolescents who attended our pediatric clinic because of obesity and OSA. Glucose homeostasis was assessed through standard 2-h oral glucose tolerance test (OGTT). Nocturnal cardio-respiratory polygraphy was performed for OSA diagnosis. Twenty-two patients underwent a 3-h OGTT to investigate insulin secretion and sensitivity through the oral-minimal model.
Results
seventy-seven children and adolescents were included in the study. Based on OSA severity, the cohort was divided into three groups (29 mild, 29 moderate, and 19 severe OSA). The group with mild OSA showed lower levels of 30-min glucose (p = 0.01) and 60-min glucose (p = 0.03), and lower prevalence of elevated 1-h glucose (10.4% versus 44.8% in moderate and 31.6% in severe OSA, p = 0.01). The odds for elevated 1-h plasma glucose was 6.2-fold (95%CI 1.6–23.4) higher in subjects with moderate and severe OSA compared to mild OSA (p = 0.007) independent of confounders. Spearman correlation test revealed a positive correlation between 30-min plasma glucose and apnea-hypopnea index (AHI, r = 0.31, p = 0.01), oxygen desaturation index (ODI, r = 0.31, p = 0.009), and mean desaturation (r = 0.25, p = 0.04). The 3-h OGTT study included 22 participants (7 mild, 9 moderate, and 6 severe OSA). The group with mild OSA showed a higher dynamic, static, and total insulin secretion compared to those with moderate and severe OSA (p < 0.0001, p = 0.007, p = 0.007, respectively). AHI was significantly correlated to dynamic insulin secretion (r = −0.48, p = 0.02).
Conclusions
OSA might impair beta-cell function reducing the pool of promptly releasable insulin in children and adolescents with obesity, in the absence of an effect on insulin sensitivity.
Similar content being viewed by others
Introduction
Obstructive sleep apnea (OSA) affects up to 40% of children and adolescent with obesity and the risk for OSA is directly correlated with obesity severity [1,2,3]. Several studies have pointed out that OSA per se might impair glucose homeostasis and lead to prediabetes and type 2 diabetes [4,5,6]. In fact, oxygen desaturation has been suggested to be a leading cause of glucose metabolism derangement and insulin-resistance independent of confounding factors [4, 5].
Despite this evidence, the pathophysiologic underpinnings of the association between OSA and glucose metabolism remain unclear, especially in pediatric groups. Mechanistic animal studies suggest that chronic intermittent hypoxia, which is the clinical consequence of OSA, may induce pancreatic beta-cell damage and lowers glucose-induced insulin secretion [7,8,9,10]. It remains unclear if this mechanism is also in place in humans and in particular in children with obesity. To fill this gap of knowledge, we enrolled 77 children and adolescents with obesity and performed a 2-h oral glucose tolerance test (OGTT) and a cardio-respiratory polygraphy. To derive more granular information on insulin secretion, in a subgroup of 22 children and adolescents we performed a prolonged 3- h OGTT and calculated the beta cell response to circulating glucose through an oral minimal model. To the best of our knowledge, this is the first study to evaluate the association between insulin secretion in children and adolescents with indexes of OSA.
Materials and methods
We enrolled children and adolescents with obesity from the outpatient obesity clinic of the University of Campania “Luigi Vanvitelli”. Children were eligible if they had a body mass index (BMI) ≥ 95th for age and sex according to reference charts [11] and presented suspected OSA based on sleep questionnaire screening [12]. Patients using medications affecting glucose or lipid metabolism, diagnosed with syndromes, endocrinopathies, and genetic forms of obesity were excluded. Written informed consent from parents and children assent was obtained before any procedure. The study was conducted according to the criteria set by the Declaration of Helsinki. The Institutional Review Board of the University of Campania Luigi Vanvitelli approved the study (protocol n. 834/2016). Written informed consent was obtained before any procedure. All participants underwent an anthropometric evaluation, overnight cardiorespiratory polygraphy, and a standard 2-h OGTT. In addition, a subgroup of patients underwent a 3-h OGTT to better evaluate insulin secretion by using the oral minimal model (OMM).
Clinical examination
Weight was measured by a balance beam scale; the child wearing undergarments. Height was measured by a Harpenden stadiometer. BMI was calculated as weight (kg)/height2 (m2). Z-score BMI was calculated with the lamba-mu-sigma method [13] according to reference charts to standardize BMI value according to age and gender [11]. Pubertal status was defined according to Tanner stage evaluating breast development in girls and testicular volume and genitalia development in boys [14]. Prepubertal boys and girls were defined as Tanner I, post-pubertal boys and girls were defined as Tanner III.
Biochemical assessment
After informed consent, a blood sample was drawn after an overnight fast. The serum was frozen at −20 °C until analyzed. Triglycerides, total cholesterol, LDL-cholesterol, and HDL-cholesterol levels were determined by an enzymatic colorimetric test with lipid clearing factor (ATLAS MEDICAL, Blankenfelde-Mahlow, Germany). Serum ALT and AST were assayed using a Hitachi Analyzer (Boerhinger-Mannheim Diagnostics, Indianapolis, IN).
Oral glucose tolerance test
After a 12-h overnight fast, children and adolescents were admitted to the Pediatric clinic of University of Campania Luigi Vanvitelli. One antecubital intravenous catheter was inserted after the local appliance of anesthetic cream for blood sampling. Flavored glucose at a dose of 1.75 g/kg weight up to a maximum of 75 g was given orally. Blood samples were obtained every 30 min for 120 min for glucose and insulin serum levels measurements. Elevated 1-h glucose was defined as 60-min glucose ≥133 mg/dL [15]. Homeostasis model assessment for insulin resistance and whole-body insulin sensitivity index (WBISI) [16] were used as measures of insulin resistance. The composite WBISI is based on values of insulin and glucose obtained from the 5-points OGTT and represents a good estimate for clamp-derived insulin sensitivity [16]. Immunoreactive insulin was assayed by IMX (Abbott Diagnostics, Santa Clara, CA). The mean intra- and inter-assay coefficients of variations were 4.7% and 7.2%, respectively.
Insulin secretion was estimated by insulinogenic index (IGI), that is a valid surrogate of beta cell function during OGTT. It is calculated as the ratio of insulin concentration at 30 min minus fasting insulin to the difference of glucose at same time [17]. Oral disposition index (ODI) was obtained by the product of WBISI and IGI [17].
Oral minimal model
Twenty-two children and adolescents underwent a 3-h OGTT to assess the OMM. Beta-Cell responsiveness (φtotal) was computed from glucose and c-peptide using the oral c-peptide minimal model [18]. Briefly, the model describes glucose-stimulated insulin secretion as the result of two components: a dynamic component, representing the secretion of promptly releasable insulin vesicular pool, that is proportional to the rate of glucose increase (φdynamic) and a static component, deriving from new insulin synthesis, this latter described by a static responsivity index (φstatic). The dynamic component describes the early insulin release due to the resident insulin pool of beta-cells and it is proportional to the rate of glucose change, therefore influencing the early glucose raise during the OGTT. Insulin sensitivity (SI) was estimated from glucose and insulin measurements during the 3-h OGTT using the oral glucose minimal model. The β-Cell responsiveness in the contest of insulin sensitivity was described by the product of φtotal × SI and defined through the disposition index (DI) [18,19].
Pediatric Sleep Questionnaire
The Pediatric Sleep Questionnaire (PSQ) [12] scores 22 items that investigate the snoring frequency, loud snoring, observed apneas, difficulty breathing during sleep, daytime sleepiness, inattentive or hyperactive behavior, and other pediatric OSA features, each previously shown to correlate with OSA confirmed by cardiorespiratory polygraphy in referred children [12]. The items are divided into nocturnal, daytime, and cognitive symptoms. Each item is scored as present, absent, or unknown. The score is calculated by dividing the number of symptoms that are present by the total number of symptoms that are present or absent (present/present + absent); any questions that are not answered (unknown) are not included in the calculation. The score can vary from 0 to 1. Previous data suggest that a cutoff value of 0.33 is most effective in identifying pediatric OSA [12,20]. All children and adolescents presenting a PSQ score ≥0.33 underwent a cardiorespiratory polygraphy.
Cardiorespiratory polygraphy
Sleep recording started at child’s usual bedtime and continued until the spontaneous awakening in the morning. Recordings were performed with Embletta® Gold device (Embla Systems Inc, Ontario, Canada) including the following sensors: nasal cannula pressure, thermistor, pulse oximeter, thoracic and abdominal respiratory inductance plethysmography, and electrocardiogram. Visual scoring of respiratory events was performed according to American Academy of Sleep Medicine (AASM) scoring criteria 2012 for children [21]. This abbreviated polygraphy without electroencephalographic, electro-oculographic or electromyographic leads has previously been demonstrated to be an accurate tool for the detection of OSA [22]. An obstructive apnea was scored if there was >90% fall in nasal pressure transducer for >90% of the entire event, the event lasted ≥2 breaths, and there was continued or increased respiratory effort. A mixed apnea was scored when there was absent respiratory effort during one portion of the event and the presence of inspiratory effort in another portion, regardless of which portion comes first. A central apnea was scored if there was absent respiratory effort for the entire event, and either the event lasted for >20 s or lasted ≥2 breaths and was associated with a ≥ 3% oxygen desaturation. A hypopnea was scored if there was a ≥ 30% reduction in amplitude of the nasal pressure transducer, the event lasted for ≥2 breaths and was associated with a ≥3% oxygen desaturation. The final apnea-hypopnea index (AHI) was determined by dividing the total number of apneas and hypopneas by the number of hours of total sleep time. A value of AHI of >1 was indicative of OSA. The ODI (defined as the number of drops in oxygen saturation ≥3% per hour of sleep time) was also calculated during the study analysis. Mean oxygen saturation (SpO2), mean oxygen desaturation (mean oxygen drop of desaturation events), and lowest oxygen saturation (Nadir) were recorded. OSA severity was scored according to pediatric criteria: mild OSA for 1 < AHI ≤ 5, moderate OSA 5>AHI < 10, severe OSA AHI ≥ 10 [21].
Statistical analysis
Continuous variables were checked for normality with Kolmogorov-Smirnov test. Difference for continuous variables were assessed with ANOVA test or Kruskall-Wallis test as appropriate. Post-hoc analysis for multiple comparisons has been performed with Dunn test. Fisher exact test or Chi-square test were performed for difference in categorical variables. Univariate logistic regression analysis was performed to assess the risk of presenting elevated 1-h plasma glucose according to OSA severity. Multiple logistic regression analysis was performed with age, z-score BMI, and pubertal stage as covariates. Spearman correlation test was performed to investigate the correlation between respiratory sleep parameters and OGTT-derived parameters. Generalized linear models (GLM) were performed to investigate the association between each respiratory parameter and each OGTT parameter adjusting for age, sex, Tanner stage, and z-score BMI. Data are expressed as median (interquartile range, IQR) or frequencies. All the analyses have been performed using SAS® on Demand for Academics (SAS Institute Inc., Cary, NC).
Results
OSA severity and glucose homeostasis during 2-h OGTT
A total of 77 children and adolescents (41 males) were included, with a median age of 11.3 ± 2.7 years, mean z-score BMI of 3.53 ± 0.69. Among them, 29 subjects (37.7%) presented with mild OSA, 29 (37.7%) showed moderate OSA, and 19 (24.6%) with severe OSA. Differences between these three groups are shown in Table 1.
The three groups did not differ in age, z-score BMI, gender, and pubertal stages. Moderate and severe OSA group had significantly higher AHI and ODI levels (p < 0.0001). Moreover, they presented higher mean desaturation levels (p = 0.0002), lower mean SpO2 (p < 0.0001), and nadir (lowest overnight saturation) values (p < 0.0001). Post-hoc analyses confirmed the significance of these differences among the three groups (Supplementary Table 1). Severe OSA group showed a trend toward higher ALT levels compared to the other two groups (p = 0.09). With regards to glucose homeostasis, we observed a significant difference for 30-min glucose and 60-min glucose among the three groups (p = 0.01 and p = 0.04, respectively). Post-hoc analyses showed that mild OSA group had lower 30-min and 60-min glucose levels compared to moderate OSA (p = 0.01 and p = 0.04), whereas no difference was observed in the other comparisons (Supplementary Table 1).
Prevalence of elevated 1-hour glucose was significantly lower in children and adolescents with mild OSA (10.4%) compared to the other groups (44.8% and 31.6%, p = 0.01). No difference was found in impaired fasting glucose (IFG), impaired glucose tolerance (IGT), and type-2 diabetes (T2D) prevalence (cumulative prevalence 3.4%, 3.4%, and 10.4% in mild, moderate, and severe OSA, p = 0.48). The odd of showing elevated 1-h plasma glucose was 6.2-fold (95% CI 1.6–23.4) higher in children and adolescents with moderate and severe OSA compared to mild OSA (p = 0.007). Multivariate analysis confirmed this association even adjusting for confounding factors (p = 0.002, Supplementary Table 2). No differences were found for insulin resistance, lipid profile, and liver enzymes between the groups.
Spearman correlation showed a positive correlation between 30-min plasma glucose and AHI (r = 0.31, p = 0.01), ODI (r = 0.31, p = 0.009), and mean desaturation (r = 0.25, p = 0.04). GLM showed a significant association between AHI (p = 0.003) and ODI (p = 0.003) with 30-min plasma glucose. Conversely, the association of mean desaturation with 30-min plasma glucose was no longer significant after adjusting for confounders.
OSA severity and insulin secretion
The subgroup of 22 children and adolescents underwent a 3-h OGTT did not differ from the 2-h OGTT cohort for age, z-score BMI, gender, pubertal stage, and OSA severity (Supplementary Table 3).
The group included children and adolescents, of whom seven had mild OSA, nine moderate OSA, and six had severe OSA. No differences were found for anthropometric characteristics, glucose levels, insulin sensitivity, DI, and IGI (Supplementary Table 4).
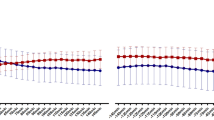
No differences were found for insulin sensitivity (SI, p = 0.17, Fig. 1, panel D) and disposition index according to OMM (beta-cell function adjusted for insulin sensitivity, p = 0.87). Nevertheless, when beta cell responsiveness was dissected into its dynamic (φdynamic) and static (φstatic) components, as described by the oral minimal model, we observed a lower dynamic, static, and total insulin secretion in those with moderate and severe OSA (p < 0.0001, p = 0.007, p = 0.007, respectively) (Fig. 1, panels A–C).
Spearman correlation showed a negative correlation between AHI and φdynamic (r = −0.48, p = 0.02; Fig. 2). No correlation was however, found between the other polygraphy parameters, φtotal and φstatic (Supplementary Table 5). No gender effect was observed in our cohort.
Discussion
Our study investigated global insulin secretion and the two different phases of beta-cell response after oral glucose in children and adolescents with obesity and OSA. The study conducted after standard 2-h OGTT revealed that children and adolescents with moderate or severe OSA displayed higher 30- and 60-min plasma glucose levels. In addition, they presented higher rates of elevated 1-hour plasma glucose that has been associated with lower insulin sensitivity and early insulin secretion in children and adolescents with obesity [16] . The association between 30-min plasma glucose and OSA severity was also verified by correlation and GLM analyses and it remained significant adjusting for confounding factors. By using the oral minimal model, we dissected the role of the single components of beta-cell responsiveness, showing that those with moderate and severe OSA have a lower dynamic and static component of beta-cell responsiveness as compared to those with mild OSA. As mentioned above, the dynamic component depends on pre-constituted insulin in pancreatic beta-cell and it influences early glucose raise during the OGTT. Among respiratory parameters, AHI correlated with late insulin secretion that describes de novo synthesis in pancreatic beta-cell. This secretion phase influences the late glucose plasma levels during OGTT and it’s impaired in IGT patients [23]. In contrast with previous studies, we found no differences in terms of insulin resistance measures between the groups.
This is the first study that performed oral minimal model to assess insulin secretion in pediatric OSA. OSA has been reported as an independent risk factor for T2D in adults and insulin resistance in both adults and children [4, 5, 8, 9, 24] However, the natural history of T2D development highlights the crucial role of beta-cell function impairment on diabetes occurrence [25]. Our results suggest an independent role for OSA in the natural history of T2D as we observed an impaired insulin secretion in children and adolescents with moderate and severe OSA. The pathogenic mechanisms underlying this association should be better investigated. OSA enhances oxidative stress and inflammation through chronic hypoxia and reoxygenation [22]. Animal models have demonstrated that chronic intermittent hypoxia damages pancreatic beta-cell through reactive oxygen species (ROS) production and inflammation [8]. The increased generation of ROS and the ensuing oxidative stress have been implicated in the progression of type 2 diabetes via pancreatic beta cell damage. Chronic intermittent hypoxia in mice models leads to persistent increase in mitochondrial ROS, which was due to impaired electron transport chain function at the complex I [8]. These processes impair glucose-induced insulin secretion [8, 9, 26]. and induce beta-cell apoptosis in rats [9]. Moreover, pancreatic inflammation, lesions and apoptosis, and insulin resistance worsened as oxygen saturation decreases, suggesting that the metabolic disorders and pancreatic injury rely on the OSA severity [9]. However, in our study, ODI, the main index of hypoxia-reoxygenation among respiratory parameters, was less associated with insulin secretion compared to AHI, suggesting that intermittent hypoxia is not the only responsible for beta-cell function derangement. Indeed, further pathophysiological mechanism can be advocated. For instance, sleep-breathing disorders have been associated with autonomic nervous system dysfunction, with a prevalence of sympathetic activity over parasympathetic system. Autonomic nervous system affects insulin sensitivity and secretion. Therefore, it might be hypothesized that this imbalance contributes to beta-cell dysfunction [27]. Moreover, it is likely that OSA-related sleep disruption, with consequent reduction of REM sleep stage with high rates of glucose utilization [28], places short sleepers at risk of poor glycemic control [28]. However, data about sleep architecture and autonomic function in our cohort are lacking. Therefore, to gain better knowledge of the complex OSA-glucose homeostasis relationship more studies should be conducted.
In addition to differences in insulin secretion, children and adolescents with severe OSA showed higher ALT levels compare to the other groups. This finding is in line to other scientific evidence that reported higher rates of non-alcoholic fatty liver disease (NAFLD) and elevated liver enzymes in children and adolescents with OSA compared to controls independent from confounding factors [29, 30]. In our cohort, we did not observe any gender effect on insulin secretion and glucose metabolism impairment. However, gender dimorphism in diabetes risk have been advocated [31]. This incongruence might be due to the small sample size that might underpower the study in identifying all the confounders.
We acknowledge that this study has some limitations. The main limitation is the lack of complete polysomnography involving EEG recordings; moreover, the subgroup undergoing the OMM is a small sample. In addition, the lack of information about adiposity distribution in the abdomen as well as the lack of information about percent body fat and fat free mass (FFM) limit the strength of the results. Despite that, it has to be taken into account that these studies (polygraphy and 3-h OGTT) are not easy to perform in young children. Further studies with larger sample size and longitudinal design might help to clarify the role of OSA in the natural history of type 2 diabetes and the potential role of non-invasive ventilatory support in restoring beta-cell function.
Conclusions
Our study investigated the association between pediatric OSA and beta-cell function in children and adolescents with obesity. This is the first pediatric study that sought to assess whether the degree of OSA is associated with beta cell response and that has used the oral minimal model to estimate insulin secretion in pediatric OSA. Our findings support the previous data of increased risk of metabolic derangement in these patients. Moreover, our study suggests that sleep apnea may predispose to an early onset of prediabetes and type 2 diabetes by impairing early insulin secretion in children and adolescents with obesity.
Data availability
Data are available are available from the corresponding author on reasonable request.
References
Mallory GB Jr, Fiser DH, Jackson R. Sleep-associated breathing disorders in morbidly obese children and adolescents. J Pediatr. 1989;115:892–7. https://doi.org/10.1016/s0022-3476(89)80738-3
Redline S, Tishler PV, Schluchter M, Aylor J, Clark K, Graham G. Risk factors for sleep-disordered breathing in children. Associations with obesity, race, and respiratory problems. Am J Respir Crit Care Med. 1999;159:1527–32. https://doi.org/10.1164/ajrccm.159.5.9809079
Kang KT, Lee PL, Weng WC, Hsu WC. Body weight status and obstructive sleep apnea in children. Int J Obes. 2012;36:920–4. https://doi.org/10.1038/ijo.2012.5
IIsobe Y, Nakatsumi Y, Sugiyama Y, Hamaoka T, Murai H, Takamura M, et al. Severity indices for obstructive sleep apnea syndrome reflecting glycemic control or insulin resistance. Intern Med. 2019;58:3227–34. https://doi.org/10.2169/internalmedicine.3005-19
Shamsuzzaman A, Szczesniak RD, Fenchel MC, Amin RS. Glucose, insulin, and insulin resistance in normal-weight, overweight and obese children with obstructive sleep apnea. Obes Res Clin Pract. 2014;8:e584–e591. https://doi.org/10.1016/j.orcp.2013.11.006.
Watson SE, Li Z, Tu W, Jalou H, Brubaker JL, Gupta S, et al. Obstructive sleep apnoea in obese adolescents and cardiometabolic risk markers. Pediatr Obes. 2014;9:471–7. https://doi.org/10.1111/j.2047-6310.2013.00198.x
Hermans MP, Ahn SA, Mahadeb YP, Rousseau MF. Sleep apnoea syndrome and 10-year cardiovascular risk in females with type 2 diabetes: relationship with insulin secretion and insulin resistance. Diabetes Metab Res Rev. 2013;29:227–34. https://doi.org/10.1002/dmrr.2387
Wang N, Khan SA, Prabhakar NR, Nanduri J. Impairment of pancreatic β-cell function by chronic intermittent hypoxia. Exp Physiol. 2013;98:1376–85. https://doi.org/10.1113/expphysiol.2013.072454
Wang Y, Hai B, Niu X, Ai L, Cao Y, Li R, et al. Chronic intermittent hypoxia disturbs insulin secretion and causes pancreatic injury via the MAPK signaling pathway. Biochem Cell Biol. 2017;95:415–20. https://doi.org/10.1139/bcb-2016-0167
Mokhlesi B, Tjaden AH, Temple KA, Edelstein SL, Sam S, Nadeau KJ, et al. Obstructive sleep apnea, glucose tolerance, and β-cell function in adults with prediabetes or untreated type 2 diabetes in the restoring insulin secretion (RISE) Study. Diabetes Care. 2021;44:993–1001. https://doi.org/10.2337/dc20-2127
Cacciari E, Milani S, Balsamo A, Spada E, Bona G, Cavallo L, et al. Italian cross-sectional growth charts for height, weight and BMI (2 to 20 yr). J Endocrinol Invest. 2006;29:581–93. https://doi.org/10.1007/BF03344156
Chervin RD, Hedger K, Dillon JE, Pituch KJ. Pediatric sleep questionnaire (PSQ): validity and reliability of scales for sleep-disordered breathing, snoring, sleepiness, and behavioral problems. Sleep Med. 2000;1:21–32. https://doi.org/10.1016/s1389-9457(99)00009-x
Cole TJ. The LMS method for constructing normalized growth standards. Eur J Clin Nutr. 1990;44:45–60.
Tanner JM, Whitehouse RH. Clinical longitudinal standards for height, weight, height velocity, weight velocity, and stages of puberty. Arch Dis Child. 1976;51:170–9. https://doi.org/10.1136/adc.51.3.170
Manco M, Miraglia Del Giudice E, Spreghini MR, Cappa M, Perrone L, Brufani C, et al. 1-Hour plasma glucose in obese youth. Acta Diabetol. 2012;49:435–43. https://doi.org/10.1007/s00592-012-0384-3
Yeckel CW, Weiss R, Dziura J, Taksali SE, Dufour S, Burgert TS, et al. Validation of insulin sensitivity indices from oral glucose tolerance test parameters in obese children and adolescents. J Clin Endocrinol Metab. 2004;89:1096–101. https://doi.org/10.1210/jc.2003-031503.
Yeckel CW, Taksali SE, Dziura J, Weiss R, Burgert TS, Sherwin RS, et al. The normal glucose tolerance continuum in obese youth: evidence for impairment in beta-cell function independent of insulin resistance. J Clin Endocrinol Metab. 2005;90:747–54. https://doi.org/10.1210/jc.2004-1258.
Cobelli C, Dalla Man C, Toffolo G, Basu R, Vella A, Rizza R. The oral minimal model method. Diabetes. 2014;63:1203–13. https://doi.org/10.2337/db13-1198
Breda E, Cavaghan MK, Toffolo G, Polonsky KS, Cobelli C. Oral glucose tolerance test minimal model indexes of beta-cell function and insulin sensitivity. Diabetes. 2001;50:150–8. https://doi.org/10.2337/diabetes.50.1.150
Chervin RD, Weatherly RA, Garetz SL, Ruzicka DL, Giordani BJ, Hodges EK, et al. Pediatric sleep questionnaire: prediction of sleep apnea and outcomes. Arch Otolaryngol Head Neck Surg. 2007;133:216–22. https://doi.org/10.1001/archotol.133.3.216
Berry RB, Budhiraja R, Gottlieb DJ, Gozal D, Iber C, Kapur VK, et al. Rules for scoring respiratory events in sleep: update of the 2007 AASM manual for the scoring of sleep and associated events. Deliberations of the Sleep Apnea Definitions Task Force of the American Academy of Sleep Medicine. J Clin Sleep Med. 2012;8:597–619. https://doi.org/10.5664/jcsm.2172
Kaditis AG, Alonso Alvarez ML, Boudewyns A, Alexopoulos EI, Ersu R, Joosten K, et al. Obstructive sleep disordered breathing in 2- to 18-year-old children: diagnosis and management. Eur Respir J. 2016;47:69–94. https://doi.org/10.1183/13993003.00385-2015
Abdul-Ghani MA, Tripathy D, DeFronzo RA. Contributions of beta-cell dysfunction and insulin resistance to the pathogenesis of impaired glucose tolerance and impaired fasting glucose. Diabetes Care. 2006;29:1130–9. https://doi.org/10.2337/diacare.2951130
Pamidi S, Wroblewski K, Broussard J, Day A, Hanlon EC, Abraham V, et al. Obstructive sleep apnea in young lean men: impact on insulin sensitivity and secretion. Diabetes Care. 2012;35:2384–9. https://doi.org/10.2337/dc12-0841.
Arslanian S. Type 2 diabetes in children: clinical aspects and risk factors. Horm Res. 2002;57:19–28. https://doi.org/10.1159/000053308
Ota H, Tamaki S, Itaya-Hironaka A, Yamauchi A, Sakuramoto-Tsuchida S, Morioka T, et al. Attenuation of glucose-induced insulin secretion by intermittent hypoxia via down-regulation of CD38. Life Sci. 2012;90:206–11. https://doi.org/10.1016/j.lfs.2011.11.011
Kakutani-Hatayama M, Kadoya M, Morimoto A, Miyoshi A, Kosaka-Hamamoto K, Kusunoki Y, et al. Associations of sleep quality, sleep apnea and autonomic function with insulin secretion and sensitivity: HSCAA study. Metabol Open. 2020;6:100033. https://doi.org/10.1016/j.metop.2020.100033
Grandner MA, Seixas A, Shetty S, Shenoy S. Sleep duration and diabetes risk: population trends and potential mechanisms. Curr Diab Rep. 2016;16:106. https://doi.org/10.1007/s11892-016-0805-8
Chen LD, Chen MX, Chen GP, Lin XJ, Huang JF, Zeng AM, et al. Association between obstructive sleep apnea and non-alcoholic fatty liver disease in pediatric patients: a meta-analysis. Pediatr Obes. 2021;16:e12718. https://doi.org/10.1111/ijpo.12718
Carotenuto M, Di Sessa A, Esposito M, Grandone A, Marzuillo P, Bitetti I, et al. Association between hepatic steatosis and obstructive sleep apnea in children and adolescents with obesity. Children. 2021;8:984. https://doi.org/10.3390/children8110984
Tramunt B, Smati S, Grandgeorge N, Lenfant F, Arnal JF, Montagner A, et al. Sex differences in metabolic regulation and diabetes susceptibility. Diabetologia. 2020;63:453–61. https://doi.org/10.1007/s00125-019-05040-3
Funding
The study was supported by FONDAZIONE Cassa di risparmio di Padova e Rovigo (CARIPARO2018 to AG) and by University of Campania Luigi Vanvitelli (Bando Giovani di Ateneo, D.R. n. 834 del 30/09/2022 to GRU).
Author information
Authors and Affiliations
Contributions
EMDG conceptualization; GRU and PM writing and editing; AG and MM oral minimal model data analysis; OC and FA cardiorespiratory study; ADS statistical analyses; EMDG and AP supervision and final manuscript revision.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
41366_2023_1257_MOESM1_ESM.docx
Post-hoc analysis for differences in anthropometric, biochemical, and polysomnographic characteristics between mild, moderate, and severe OSA groups.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Umano, G.R., Galderisi, A., Aiello, F. et al. Obstructive sleep apnea (OSA) is associated with the impairment of beta-cell response to glucose in children and adolescents with obesity. Int J Obes 47, 257–262 (2023). https://doi.org/10.1038/s41366-023-01257-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41366-023-01257-w