Abstract
Objective
To explore the prevalence of obesity among American Indian and Alaska Native (AIAN) adolescents aged 12–19 years in association with social determinants of health (SDOH), and mental health and substance use disorders.
Methods
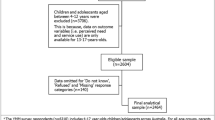
Guided by the World Health Organization’s Social Determinants of Health Framework, we examined data from the Indian Health Service (IHS) Improving Health Care Delivery Data Project from Fiscal Year 2013, supplemented by county-level data from the U.S. Census and USDA. Our sample included 26,226 AIAN adolescents ages 12–19 years. We described obesity prevalence in relationship to SDOH and adolescents’ mental health and substance use disorder status. We then fit a multivariable logit generalized linear mixed model to estimate the relationships after adjusting for other individual and county level characteristics.
Results
We observed a prevalence of 32.5% for obesity, 13.8% for mental health disorders, and 5.5% for substance use disorders. Females had lower odds of obesity than males (OR = 0.76, p < 0.001), which decreased with age. Having Medicaid coverage (OR = 1.09, p < 0.01), residing in a county with lower education attainment (OR = 1.17, p < 0.05), and residing in a county with higher rates of poverty (OR = 1.51, p < 0.001) were each associated with higher odds of obesity. Residing in a county with high access to a grocery store (OR = 0.73, p < 0.001) and residing in a county with a higher proportion of AIANs (OR = 0.83, p < 0.01) were each associated with lower odds of obesity. Those with mental health disorders had higher odds of obesity (OR = 1.26, p < 0.001); substance use disorders were associated with decreased odds of obesity (OR = 0.73, p < 0.001).
Conclusions
Our findings inform future obesity prevention and treatment programs among AIAN youth; in particular, the need to consider mental health, substance use, and SDOH.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
Data availability
The data that support the findings of this study are available from the United States Agency Indian Health Services within the Department of Health and Human Services. Restrictions apply to the availability of the data, which are owned by the tribal nations involved and used under approval for this study. Data requests must be submitted to the IHS National Institutional Review Board (irb@ihs.org), and each of the tribal IRBs, tribal councils and tribal authorities involved with the Indian Health Service Data Project.
References
Bullock A, Sheff K, Moore K, Manson S. Obesity and overweight in American Indian and Alaska Native children, 2006-2015. Am J Public Health. 2017;107:1502–7.
Hales C, Carroll MD, Fryar C, Ogden C. Prevalence of obesity among adults and youth: United States, 2015–2016. In: Statistics NCfH, editor. Rockville, MD: Centers for Disease Control and Prevention; 2017.
Tanamas SK, Reddy SP, Chambers MA, Clark EJ, Dunnigan DL, Hanson RL, et al. Effect of severe obesity in childhood and adolescence on risk of type 2 diabetes in youth and early adulthood in an American Indian population. Pediatric Diabetes. 2018;19:622–9.
Indian Health Service IHS. Newsroom: Disparities—Indian Health Service (IHS). 2013. http://www.ihs.gov/newsroom/factsheets/disparities/.
Tominaga K, Fujimoto E, Suzuki K, Hayashi M, Ichikawa M, Inaba Y. Prevalence of non-alcoholic fatty liver disease in children and relationship to metabolic syndrome, insulin resistance, and waist circumference. Environ Health Prev Med. 2009;14:142–9.
Arias E, Xu J, Curtin S, Bastian B, Tejada-Vera B. Mortality profile of the non-Hispanic American Indian or Alaska Native population, 2019. National Center for Health Statistics (U.S.), editor. National Vital Statistics Reports. 2021;70. https://stacks.cdc.gov/view/cdc/110370.
Solar O, Irwin A. A conceptual framework for action on the social determinants of health. Geneva: WHO Document Production Services; 2010.
World Health Organization (WHO). WHO | About social determinants of health: World Health Organization; 2017. http://www.who.int/social_determinants/sdh_definition/en/.
Health WCoSDo, Organization WH. Closing the gap in a generation: health equity through action on the social determinants of health: Commission on Social Determinants of Health final report: World Health Organization; 2008.
US Department of Health and Human Services. Social Determinants of Health: Office of Disease Prevention and Health Promotion; 2020. https://www.healthypeople.gov/2020/topics-objectives/topic/social-determinants-of-health.
Schell LM, Gallo MV. Overweight and obesity among North American Indian infants, children, and youth. Am J Hum Biol. 2012;24:302–13.
Czyzewski K. Colonialism as a broader social determinant of health. Int Indig Policy J. 2011;2:5.
Baldwin JA, Brown BG, Wayment HA, Nez RA, Brelsford KM. Culture and context: buffering the relationship between stressful life events and risky behaviors in American Indian youth. Subst Use Misuse. 2011;46:1380–94.
O’Connell JM, Novins DK, Beals J, Whitesell N, Libby AM, Orton HD, et al. Childhood characteristics associated with stage of substance use of American Indians: family background, traumatic experiences, and childhood behaviors. Addict Behav. 2007;32:3142–52.
Whitbeck LB, Hoyt DR, McMorris BJ, Chen X, Stubben JD. Perceived discrimination and early substance abuse among American Indian children. J Health Soc Behav. 2001;42:405–24.
Johnson-Jennings MD, Belcourt A, Town M, Walls ML, Walters KL. Racial discrimination’s influence on smoking rates among American Indian Alaska Native two-spirit individuals: does pain play a role? J Health Care Poor Underserved. 2014;25:1667–78.
Shepherd CC, Li J, Cooper MN, Hopkins KD, Farrant BM. The impact of racial discrimination on the health of Australian Indigenous children aged 5–10 years: analysis of national longitudinal data. Int J Equity Health. 2017;16:161–73.
McCubbin LD, Antonio M. Discrimination and obesity among Native Hawaiians. Hawaii J Med Public Health. 2012;71:346–52.
Palmisano GL, Innamorati M, Vanderlinden J. Life adverse experiences in relation with obesity and binge eating disorder: a systematic review. J Behav Addict. 2016;5:11–31.
Eitle TM, Eitle D, Johnson-Jennings M. General strain theory and substance use among American Indian adolescents. Race Justice. 2013;3:3–30.
Young C, Hanson C, Craig JC, Clapham K, Williamson A. Psychosocial factors associated with the mental health of Indigenous children living in high income countries: a systematic review. Int J Equity Health. 2017;16:153–160.
American Psychiatric Association. Mental health disparities: American Indians and Alaska Natives American Psychiatric Association; 2017. https://www.psychiatry.org/Filepercent20Library/Psychiatrists/Cultural-Competency/Mental-Health-Disparities/Mental-Health-Facts-for-American-Indian-Alaska-Natives.pdf.
Swaim RC, Stanley LR. Substance use among American Indian youths on reservations compared with a national sample of US adolescents. JAMA Network Open. 2018;1:e180382–e.
Classen T, Hokayem C. Childhood influences on youth obesity. Econ Hum Biol. 2005;3:165–87.
Marmorstein NR, Iacono WG, Legrand L. Obesity and depression in adolescence and beyond: reciprocal risks. Int J Obes. 2014;38:906.
Newman D, Sontag L, Salvato R. Psychosocial aspects of body mass and body image among rural American Indian adolescents. J Youth Adolesc. 2006;35:265–75.
Wilson SM, Sato AF. Stress and paediatric obesity: what we know and where to go. Stress Health. 2014;30:91–102.
Pasch KE, Velazquez CE, Cance JD, Moe SG, Lytle LA. Youth substance use and body composition: does risk in one area predict risk in the other? J Youth Adolesc. 2012;41:14–26.
Farhat T, Iannotti RJ, Simons-Morton BG. Overweight, obesity, youth, and health-risk behaviors. Am J Prev Med. 2010;38:258–67.
DeLong AJ, Larson NI, Story M, Neumark-Sztainer D, Weber-Main AM, Ireland M. Factors associated with overweight among urban American Indian adolescents: findings from Project EAT. Ethn Dis. 2008;18:317–23.
Jennings DR, Paul K, Little MM, Olson D, Johnson-Jennings MD. Identifying perspectives about health to orient obesity intervention among urban, transitionally housed Indigenous children. Qual Health Res. 2020;30:894–905.
O’Connell J, Guh S, Ouellet J, Rockell, J.; Li, Y.; Croy, C.; and Gutilla, M. ARRA ACTION: comparative effectiveness of health care delivery systems for American Indians and Alaska Natives using enhanced data infrastructure: final report. Rockville, MD: Agency for Healthcare Research and Policy; 2014.
US Department of Department of Health and Human Services. Centers for Disease Control. Healthy People 2020. Washington DC; 2013. Accessed March 2018. http://www.healthypeople.gov/.
Indian Health Service. Age and Gender of the IHS User Population. Fiscal Year 2010. Unpublished report. Rockville, MD: U.S. Department of Health and Human Services; 2010. Accessed March 2017.
US Department of Health and Human Services. CDC Growth Charts. Centers for Disease Control and Prevention. Accessed March 1, 2018. http://www.cdc.gov/growthcharts/cdc_charts.htm.
USDA Food Environment Atlas: USDA; 2010. http://www.ers.usda.gov/data-products/food-environment-atlas.aspx.
Hileman G, Steele S. Accuracy of claims-based risk scoring models. Schaumburg, Illinois; 2016.
US Department of Health and Human Services. Risk adjustment: U.S. Centers for Medicare & Medicaid Service. Accessed online March 2017. https://www.cms.gov/Medicare/Health-Plans/MedicareAdvtgSpecRateStats/Risk-Adjustors.
Peterson L, Crockett A. Adolescent development: health risks and opportunities for health promotion. In: Millstein S, Petersen A, Nightengale E, editors. Promoting the health of adolescents: new directions for the 21st century. Oxford: Oxford University Press; 1993.
Erikson EH. Identity, youth, and crisis. New York: W. W. Norton; 1968.
Arnett JJ. Emerging adulthood: a theory of development from the late teens through the twenties. Am Psychol. 2000;55:469–80.
Sweeting HN. Gendered dimensions of obesity in childhood and adolescence. Nutr J. 2008;7:1.
Frederick CB, Snellman K, Putnam RD. Increasing socioeconomic disparities in adolescent obesity. Proc Natl Acad Sci USA. 2014;111:1338.
Eitle TM, Johnson-Jennings M, Eitle DJ. Family structure and adolescent alcohol use problems: extending popular explanations to American Indians. Soc Sci Res. 2013;42:1467–79.
Johnson-Jennings M, Paul K, Olson D, Labeau M, Jennings D. Ode’imin Giizis: proposing and piloting gardening as an Indigenous childhood health intervention. J Health Care Poor Underserved. 2020;31:871–88.
Satterfield D, DeBruyn L, Santos M, Alonso L. Health promotion and diabetes prevention in American Indian and Alaska Native Communities—Traditional Foods Project, 2008–2014. MMWR Suppl. 2016;65:4–10.
Warne D, Frizzell LB. American Indian Health Policy: historical trends and contemporary issues. Am J Public Health. 2014;104:S263–7.
Goins RT, Conway C, Reid M, Jiang L, Chang J, Huyser KR, et al. Social determinants of obesity in American Indian and Alaska Native peoples aged ≥50 years. Public Health Nutr. 2022:1–10. https://www.cambridge.org/core/journals/public-health-nutrition/article/social-determinants-of-obesity-in-american-indian-and-alaska-native-peoples-aged-50-years/7BCDFFA6BFDF220BDDDFA90B94D6FF40.
Brace AM, Moore TW, Matthews TL. The relationship between food deserts, farmers’ markets, and food assistance programs in Hawai’i census tracts. Hawaii J Health Soc Welf. 2020;79:36–41.
Schaft KA, Jensen EB, Hinrichs CC. Food deserts and overweight schoolchildren: evidence from Pennsylvania*. Rural Sociol. 2009;74:153–77.
Campbell CD, Evans-Campbell T. Historical trauma and Native American child development and mental health: an overview. In: Sarche MC, Spicer P, Farrell P, Fitzgerald HE, editors. American Indian and Alaska Native children and mental health: development, context, prevention, and treatment. Santa Barbara: Praeger Publishing. 2011. p. 1–26.
Hunter RG, McEwen BS. Stress and anxiety across the lifespan: structural plasticity and epigenetic regulation. Epigenomics. 2013;5:177–94.
Kalarchian MA, Marcus MD, Levine MD, Courcoulas AP, Pilkonis PA, Ringham RM, et al. Psychiatric disorders among bariatric surgery candidates: relationship to obesity and functional health status.(Author abstract). Am J Psychiatry. 2007;164:328.
da Luz FQ, Hay P, Touyz S, Sainsbury A. Obesity with comorbid eating disorders: associated health risks and treatment approaches. Nutrients. 2018;10:829–38.
Whitegoat W, Vu J, Thompson K, Gallagher J. Mental health in diabetes prevention and intervention programs in American Indian/Alaska Native Communities. Wash Univ J Am Indian Alsk Native Health. 2015;1:4–19.
Johnson-Jennings MD, Paul K, Olson D, LaBeau M, Jennings D. Ode’imin Giizis: proposing and piloting gardening as an Indigenous childhood health intervention. J Health Care Poor Underserved. 2020;31:871–88.
Huang DY, Lanza HI, Anglin MD. Association between adolescent substance use and obesity in young adulthood: a group-based dual trajectory analysis. Addict Behav. 2013;38:2653–60.
Pasch KE, Nelson MC, Lytle LA, Moe SG, Perry CL. Adoption of risk-related factors through early adolescence: associations with weight status and implications for causal mechanisms. J Adolesc Health. 2008;43:387–93.
Gearhardt AN, Corbin WR, Brownell KD. Food addiction: an examination of the diagnostic criteria for dependence. J Addict Med. 2009;3:1–7.
Johnson-Jennings M, Johnson-Jennings A, Jennings D. Land transforming place: land as a culturally appropriate venue for health interventions among Indigenous persons. International Medical and Health Sciences Conference Paper. Phuket, Thailand: Research Fora; 2020. p. 8.
Funding
The research reported in this publication was supported by the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) of the National Institutes of Health under Award Numbers P30DK092923 (SMM) and R18DK114757 (JO and SMM). Funding for the development of the data infrastructure, utilized in the reported analyses, was supported by the Agency for Healthcare Research and Quality (290-2006-00020-I, TO #11, JO) and the Patient-Centered Outcomes Research Institute (AD-1304–6451, JO). Furthermore the lead author received partial support from CIHR and NIH R01-DA037176-01, The content of this report is solely the responsibility of the authors and does not necessarily represent the official views of these organizations. The data used in this secondary analysis stem from project, known as the Indian Health Service (IHS) Health Care Delivery Data Project. The data set includes information for many American Indian and Alaska Native communities. This work was conducted with the guidance and advice of IHS and Tribal health program colleagues, as well as members of the project’s Steering, Project Site, and Patient Committees. Members of Tribal and IHS institutional review boards, Tribal Councils, and Tribal Authorities educate us about the health concerns they have for their Tribal members and how they hope this project will inform their work. This project relies on their support and approval. The authors would also like to express their gratitude to Sara Mumby for her editorial assistance.
Author information
Authors and Affiliations
Contributions
MDJJ: conceptualization, original draft preparation, investigation, methodology, investigation, writing—review and editing, project administration; MR: methodology, formal analysis, data curation/management, visualization, writing reviewing and editing; LJ: methodology, visualization, formal analysis, data curation/management, writing reviewing and editing; KRH: conceptualization, methodology, writing—review and editing; AGB: project administration, investigation, supervision, conceptualization, methodology, writing—reviewing and editing; JFS: supervision, conceptualization writing—reviewing and editing, project administration; SMM: conceptualization, supervision, validation, writing—reviewing and editing, funding acquisition, project administration; JC: data curation, writing—reviewing and editing; ALFJ: writing reviewing and editing; CC: writing reviewing and editing; JO: supervision, conceptualization, project administration, data curation, investigation, methodology, writing reviewing and editing.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Johnson-Jennings, M.D., Reid, M., Jiang, L. et al. American Indian Alaska Native (AIAN) adolescents and obesity: the influence of social determinants of health, mental health, and substance use. Int J Obes 47, 297–305 (2023). https://doi.org/10.1038/s41366-022-01236-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41366-022-01236-7