Abstract
Objective
Using a systematic review and meta-analysis, we aimed to estimate the mean effect of acute glucagon administration on components of energy balance and glucose homoeostasis in adults without diabetes.
Methods
CENTRAL, CINAHL, Embase, MEDLINE, PubMed, and Scopus databases were searched from inception to May 2021. To be included, papers had to be a randomised, crossover, single- or double-blind study, measuring ad libitum meal energy intake, energy expenditure, subjective appetite, glucose, and/or insulin following acute administration of glucagon and an appropriate comparator in adults without diabetes. Risk of bias was assessed using the Revised Cochrane Risk of Bias Tool for Randomized trials with additional considerations for cross-over trials. Certainty of evidence was assessed using the GRADE approach. Random-effect meta-analyses were performed for outcomes with at least five studies. This study is registered on PROSPERO (CRD42021269623).
Results
In total, 13 papers (15 studies) were considered eligible: energy intake (5 studies, 77 participants); energy expenditure (5 studies, 59 participants); subjective appetite (3 studies, 39 participants); glucose (13 studies, 159 participants); insulin (12 studies, 147 participants). All studies had some concerns with regards to risk of bias. Mean intervention effect of acute glucagon administration on energy intake was small (standardised mean difference [SMD]: –0.19; 95% CI, –0.59 to 0.21; P = 0.345). Mean intervention effect of acute glucagon administration on energy expenditure (SMD: 0.72; 95% CI, 0.37–1.08; P < 0.001), glucose (SMD: 1.11; 95% CI, 0.60–1.62; P < 0.001), and insulin (SMD: 1.33; 95% CI, 0.88–1.77; P < 0.001) was moderate to large.
Conclusions
Acute glucagon administration produces substantial increases in energy expenditure, and in circulating insulin and glucose concentrations. However, the effect of acute glucagon administration on energy intake is unclear. Insufficient evidence was available to evaluate the acute effect of glucagon on subjective appetite.
Similar content being viewed by others
Introduction
Obesity is a global health burden associated with increased cardiometabolic disease risk and mortality [1, 2]. Lifestyle modification centred on dietary restriction and increased physical activity is the first-line treatment. However, adherence to such programmes is typically poor and weight-loss often modest [3, 4]. Bariatric surgery produces substantial and sustained weight loss [5], but it is not universally available or acceptable to all eligible patients. Therefore, pharmacological interventions are urgently required for long-term weight-loss.
Glucagon is a 29 amino acid polypeptide synthesised by the alpha cells of the pancreatic islets, which acts via the glucagon receptor (GCGR) to exert various physiological effects [6]. Glucagon is primarily known for its role in glucose homoeostasis [7], but has also been identified as a key regulator of amino acid metabolism [8]. Furthermore, glucagon is implicated in the stress response, being released under conditions of psychological and metabolic stress [9], including prolonged fasting [10] and acute exercise [11]. Evidence from rodent models have demonstrated that glucagon can also regulate energy balance, acting to concurrently raise energy expenditure [12] and suppress energy intake [13], and thus influence body weight [14]. This is thought to be achieved via both direct mechanisms, including GCGR activation on target tissues such as the hypothalamus [15] and brown adipose tissue [16], and indirect mechanisms, including the release of other hormones such as fibroblast growth factor 21 [17] and catecholamines [18].
GCGR agonism has consequently been identified as a possible therapeutic target for obesity, and a number of studies have investigated the effects of acute glucagon administration on energy intake and energy expenditure in humans. However, the magnitude and/or direction of effects following glucagon administration has been mixed for these components [19,20,21,22,23], likely attributable to differences in study design. Indeed, effects attributed to glucagon are frequently confounded by co-infusion of other bioactive peptides, such as somatostatin [24, 25]. Moreover, many studies do not include an appropriate control arm, instead favouring pre-post designs that do not exclude the effect of time on observed responses [26,27,28].
We therefore conducted a systematic review and random-effects meta-analysis to estimate the mean effects of acute glucagon administration on energy intake, energy expenditure, and subjective hunger in adults without diabetes. Furthermore, mean glucose and insulin responses following acute glucagon administration were also estimated due to their influence on energy balance [29, 30] and recognised association with glucagon.
Methods
Registration
This Review was registered in the international prospective register of systematic reviews (PROSPERO; registration number: CRD42021269623) and written in accordance with the recommendations outlined in the PRISMA 2020 statement [31].
Eligibility criteria
Population
We included randomised, controlled, single- or double blind, crossover studies in adults (>18 years old) of any body mass index (BMI) value. Studies performed in current smokers, pregnant individuals, or individuals with a history of chronic disease (including type 1 and type 2 diabetes) were excluded.
Intervention
Administration of glucagon via any route (intravenous, intramuscular, intranasal) for less than 24 h while at rest. Studies which administered glucagon for longer than 24 hours or co-infused pharmacological agents (e.g. somatostatin) were excluded. Studies could be performed in the fasted or postprandial state.
Comparator
To be included, studies must have performed a time-and energy matched control arm that administered an energy-free control agent (e.g. saline) in place of glucagon.
Outcome
Studies measuring energy intake, energy expenditure, subjective appetite, glucose, and/or insulin were included.
We only considered studies written in the English language and published in peer-reviewed journals. Conference abstracts were excluded. If methodology and/or participant characteristics were not described sufficiently to determine study eligibility, corresponding authors were contacted. If the author did not respond, or could not provide the required information, the study was excluded.
Information sources and search strategy
J.F. searched CENTRAL, CINAHL, Embase, MEDLINE, PubMed, and Scopus databases on 24 May 2021. Embase and Medline databases were accessed via Ovid, and the CINAHL database was accessed via EBSCOhost. All databases were searched from inception to 24 May 2021.
The search strategy was developed based on the PICO format, with additional concepts incorporated to exclude pre-clinical studies. Full details of the search strategy are provided in Supplementary Appendix A. No limits were used during any database search.
Backward (using Google Scholar) and forward citation searching of eligible papers was also performed by J.F on 23 July 2021.
Selection process
Results of each database search were imported into Covidence systematic review software (Veritas Health Innovation, Australia). Duplicate results were automatically detected and removed by Covidence. Title and abstracts were then independently screened by JF and ESC, with each paper being classified as ‘yes’,’no’ or ‘maybe’. Papers classified as ‘yes’ or ‘maybe’ by both JF and ESC continued to the full-text screening phase. All disputes (papers with a ‘yes’ or ‘maybe’ and a ‘no’ vote) were resolved prior to conducting full-text screening. Full texts of each paper were then accessed and independently classified as ‘yes’ or ‘no’ by JF and ESC. Papers classified as ‘yes’ continued to the data extraction phase. Disputes following full-text screening (papers with a ‘yes’ and a ‘no’ vote) were resolved via a meeting with all authors prior to data extraction.
Data collection
Corresponding authors for all eligible studies were first contacted for raw study data. If authors did not respond or could not provide raw study data, data were extracted from the published manuscript. WebPlotDigitizer Version 4.2 (Ankit Rohatgi, USA) was used to extract data from papers that only presented data in a figure.
When data were displayed inadequately (e.g. clustering of data points, overlapping of error bars) or data were not reported in published manuscript or supplementary materials (despite methods stating measurements had been taken), the paper was no longer considered eligible and excluded from analysis.
Data were collected by a single author (JF) and stored in an electronic spreadsheet (Excel 2016, Microsoft Corporation, USA). If data were presented from multiple glucagon doses, only data from the highest dose was collected. ESC checked the accuracy of collected data by comparing the results stored in the electronic spreadsheet with those in the published manuscript or raw study data.
Data items
Eligible outcomes were defined as follows
Energy intake—total ad libitum energy intake at the first meal presented to participants following the administration of glucagon and comparator. Measured in kcal, kJ, or grams.
Energy expenditure—change in energy expenditure (pre- vs post-administration) in the glucagon and comparator arms, in which pre-administration is a baseline measurement prior to glucagon/comparator administration and post-administration is a measurement at least 30 min after initial glucagon/comparator administration (to allow sufficient time for an effect to be observed). Alternatively, baseline and at least two other timepoints during the glucagon and comparator arms, or total energy expenditure during the glucagon and comparator arms. Measured in kcal, kJ, or V̇O2.
Subjective appetite—assessed at baseline and at least two other timepoints during the glucagon and comparator arms. Alternatively, total or incremental area under the curve (AUC) for the glucagon and comparator arms. Measured by a visual analogue scale (VAS) or other questionnaire assessing a domain relating to appetite (e.g. hunger, pleasantness, prospective consumption, fullness) or a composite appetite score.
Glucose—assessed at baseline and at least two other timepoints during the glucagon and comparator arms. Alternatively, total or incremental AUC for the glucagon and comparator arms. Measured in serum or plasma.
Insulin—assessed at baseline and at least two other timepoints during the glucagon and comparator arms. Alternatively, total or incremental AUC for the glucagon and comparator arms. Measured in serum or plasma.
Pre-vs post administration values were accepted for energy expenditure (but not subjective appetite, glucose, or insulin) due to energy expenditure measurements being performed over extended time periods (e.g. 10–30 min) compared to measurements taken at single time points.
The following data items were also collected relating to paper, participant, and intervention characteristics: author(s), year of publication, sample size, proportion of males, participant age, participant BMI, degree of blinding, route of administration, glucagon dose, and duration of administration.
Risk of bias assessment
Risk of bias assessment was performed by a single author (JF). Risk of bias of included studies was assessed using the Revised Cochrane Risk of Bias Tool for Randomized trials (RoB 2.0) with additional considerations for cross-over trials. Risk of bias was assessed using the following domains: bias arising from the randomization process; bias arising from period and carryover effects; bias due to deviations from intended intervention; bias due to missing outcome data; bias in the measurement of the outcome; and bias in the selection of the reported result. Risk of bias assessment was performed for each outcome (energy intake, energy expenditure, subjective appetite, glucose, insulin), in which the risk of bias of each individual study was determined by the highest risk of bias level attained in any of the assessed domains. Studies were not excluded based on the risk of bias assessment.
Data synthesis
Data were collated and grouped by outcome (energy intake, energy expenditure, subjective appetite, glucose, insulin). Standard errors and 95% confidence intervals (CIs) were converted to standard deviations. For energy expenditure, subjective appetite, glucose, and insulin outcomes only, and for studies in which only time-series data were reported, total AUC was calculated for glucagon and comparator arms using the maximum number of timepoints available. If data were extracted from figures using WebPlotDigitizer, standard deviations of AUCs were estimated using the AUC of values depicted by the corresponding top or bottom error bars. If multiple data types were presented (AUC, time points, and/or pre- vs post-administration), the order of priority for extraction was as follows: AUC > time points > pre- vs post-administration.
Standardised mean differences (SMDs) were then calculated for each study as described by Higgins et al. [2]. When raw study data were not available, a correlation coefficient of 0.5 was assumed to calculate the standard error of the SMD [27]. Sensitivity analyses using correlation coefficients of 0.3, 0.7, and 0.9 were performed to assess the robustness of findings to this assumption.
A random-effects meta-analysis model was selected as the effect of glucagon administration on outcomes was expected to vary across studies due to differences in participant and intervention characteristics. This model assumes a distribution of true effect sizes across studies and provides an estimate of the mean intervention effect of this distribution [32, 33]. Between-study variance (τ2) was estimated using the Hartung-Knapp-Sidik-Jonkman method [34, 35], with summary effect CIs being calculated using the Wald-type method [36]. Results of syntheses were presented using forest plots. Leave-one-out meta-analysis was also performed to identify studies that have a large influence on the summary effect estimate.
Statistical heterogeneity was assessed using the τ2 and I2 statistics alongside their corresponding 95% CIs. Random-effects 95% prediction intervals (PIs) were also calculated to facilitate the interpretation of statistical heterogeneity by providing an expected range of intervention effects in similar future studies. Mixed-effects meta-regression using the Knapp and Hartung adjustment [37] was used to explore possible causes of statistical heterogeneity for outcomes with at least ten studies. Separate univariable models were created for each potential moderator: (i) route of administration, and (ii) total glucagon dose. The choice of moderators was made post-hoc.
Potential publication bias was assessed via visual inspection of contour-enhanced funnel plots [38] and statistically by Egger’s regression test for outcomes containing at least 10 studies. Trim and fill analyses (L0 estimator) were used when publication bias was suspected to explore its impact on effect sizes [39].
All analyses were performed in R version 4.1.0 [40] using the R package ‘metafor’ [41] by one author (JF). Random-effects meta-analysis was only performed for outcomes with at least five studies [42]. Individual study effects were described for outcomes with less than five studies.
Certainty of evidence assessment
Certainty of evidence was assessed by two authors (JF and ESC) using the GRADE approach [43, 44]. Certainty of evidence was assessed using the following domains: study limitations, consistency of effect, imprecision, indirectness, and publication bias. Estimated effect of each outcome was independently classified as high (true effect is similar to the estimated effect), moderate (true effect is probably close to the estimated effect), low (true effect might be markedly different from the estimated effect), or very low (true effect is probably markedly different from the estimated effect) certainty of evidence.
Results
Study selection
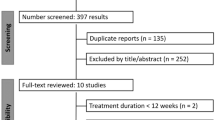
Database searching found 24,833 potentially eligible papers. Following removal of duplicates, 13,020 papers underwent title and abstract screening, resulting in the removal of 12,744 papers. Consequently, 246 papers underwent full-text screening, yielding 13 eligible papers. Due to several papers containing multiple studies, a total of 15 separate studies were deemed eligible. The following number of studies proved eligible for each outcome: energy intake, 5 studies; energy expenditure, 5 studies; subjective appetite, 4 studies; glucose, 13 studies; insulin, 12 studies. This process is summarised in Fig. 1.
Several studies appeared to meet inclusion criteria but were subsequently excluded due to insufficient information regarding blinding, randomization, and comparator used (Supplementary Appendix B).
Study characteristics
Study characteristics of included studies are presented in Table 1.
Risk of bias
The results of the risk of bias assessment for each outcome are presented in Supplementary Appendix C. With regards to overall risk of bias, there were some concerns for all studies included in the review, irrespective of the outcome measured. This was primarily due to inadequate reporting of the randomization and sequence allocation process, or inadequate reporting of the analysis plan.
Meta-analysis
Data used for meta-analysis is presented in Supplementary Appendix D. This also includes details of data source.
Energy intake
Five studies comprising 77 participants (90% males) measured ad libitum energy intake following comparator and glucagon administration [20, 21, 45,46,47]. Of these five studies, four used intravenous administration [20, 23, 45, 46] and one used intranasal administration [47]. Average age of participants ranged from 22.0 to 48.5 years, with three studies being conducted in healthy-weight participants (18.5 ≥ BMI < 25.0) [20, 23, 46] and two studies being conducted in overweight participants (25.0 ≥ BMI < 30.0) [45, 47].
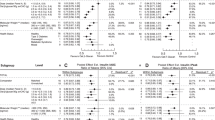
Mean intervention effect of glucagon administration relative to comparator on ad libitum meal energy intake was SMD = –0.19 (95% CI, –0.59 to 0.21; P = 0.345; Fig. 2). Measures of statistical heterogeneity were τ2 = 0.16 (95% CI, 0.03–1.67) and I2 = 81% (95% CI, 41–98%). According to the 95% PI, the effect size for acute glucagon administration relative to comparator on ad libitum meal energy intake is expected to range from –1.60 to 1.22 in future similar studies. Meta-regression and assessments of publication bias were not performed due to an insufficient number of studies.
Results produced from a random-effects meta-analysis using the Hartung-Knapp-Sidik-Jonkman method to estimate between-study variance. Data are presented as mean with 95% confidence intervals. Mean-intervention effect (summary) is also presented alongside a 95% prediction interval (grey horizontal dotted line). Sample size (N), dose (duration of administration in minutes), and route of administration (colour of point estimates) for each study are provided. CI confidence interval, PI prediction interval, SMD standardised mean difference.
Energy expenditure
Five studies containing 59 participants (84% males) measured energy expenditure following comparator and glucagon administration [21, 22, 45, 47, 48]. Of these five studies, four used intravenous administration [21, 22, 45, 48] and one used intranasal administration [47]. Average age of participants ranged from 25.8 to 26.1 years, with two studies being conducted in healthy-weight participants [21, 22] and three studies being conducted in overweight participants [45, 47, 48].
Mean intervention effect of glucagon administration relative to comparator on energy expenditure was SMD = 0.72 (95% CI, 0.37–1.08; P < 0.001; Fig. 3). Measures of statistical heterogeneity were τ2 = 0.04 (95% CI, 0.00–0.74) and I2 = 23% (95% CI, 0–85%). According to the 95% PI, the effect size for acute glucagon administration relative to comparator on energy expenditure is expected to range from –0.12 to 1.56 in future similar studies. Meta-regression and assessments of publication bias were not performed due to an insufficient number of studies.
Results produced from a random-effects meta-analysis using the Hartung-Knapp-Sidik-Jonkman method to estimate between-study variance. Data are presented as mean with 95% confidence intervals. Mean-intervention effect (summary) is also presented alongside a 95% prediction interval (grey horizontal dotted line). Sample size (N), dose (duration of administration in minutes), and route of administration (colour of point estimates) for each study are provided. CI confidence interval, PI prediction interval, SMD standardised mean difference.
Subjective appetite
Four studies comprising 57 participants (73% males) measured subjective appetite following comparator and glucagon administration [19, 20]. Of these four studies, two used intramuscular [19] administration and two used intravenous administration [20, 23]. Average age of participants ranged from 22.0 to 28.4 years, with three studies being conducted in healthy-weight participants [19, 20, 23] and one study being conducted in obese participants (BMI ≥ 30.0) [19]. Two studies reported subjective satiety [19], one study reported a composite appetite score [20], and one study reported subjective hunger [23].
Due to the limited number of studies, a meta-analysis was not performed. However, two studies reported an increase in subjective appetite following glucagon administration relative to comparator [19, 20] and two studies reported a decrease in subjective appetite [19, 23] (Supplementary Appendix D).
Glucose
Thirteen studies comprising 159 participants (80% males) measured glucose following comparator and glucagon administration [19,20,21, 23, 45, 47,48,49,50,51,52]. Of these 13 studies, nine used intravenous administration [20, 21, 23, 45, 48,49,50,51,52], 3 used intramuscular administration [19, 49], and one used intranasal administration [47]. Average age of participants ranged from 21.0 to 48.5 years, with five studies being conducted in healthy-weight participants [19,20,21, 23, 51], four studies being conducted in overweight participants [45, 47, 48, 50], and one study being conducted in obese participants [19]. Three studies did not report participant body weight characteristics [49, 52].
Mean intervention effect of glucagon administration relative to comparator on glucose was SMD = 1.11 (95% CI, 0.60 to 1.62; P < 0.001; Fig. 4). Measures of statistical heterogeneity were τ2 = 0.64 (95% CI, 0.71–2.10) and I2 = 82% (95% CI, 55–94%). According to the 95% PI, the effect size for acute glucagon administration relative to comparator on glucose is expected to range from –0.74 to 2.97 in future similar studies.
Results produced from a random-effects meta-analysis using the Hartung-Knapp-Sidik-Jonkman method to estimate between-study variance. Data are presented as mean with 95% confidence intervals. Mean-intervention effect (summary) is also presented alongside a 95% prediction interval (grey horizontal dotted line). Sample size (N), dose (duration of administration in minutes), and route of administration (colour of point estimates) for each study are provided. *duration of administration not reported. CI confidence interval, PI prediction interval, SMD standardised mean difference.
Mixed-effects meta-regression analyses with route of administration or total glucagon dose included as a moderator did not indicate that glucose response differed between administration routes or across total glucagon dose (Supplementary Appendix E).
Visual inspection of the contour-enhanced funnel plot showed asymmetry that indicated potential publication bias (Supplementary Appendix F). This is supported by the result of Egger’s regression test (P < 0.001). Trim and fill analysis estimated five missing studies on the left side of the funnel plot (Supplementary Appendix F), resulting in adjusted SMD of 0.63 (95% CI, 0.01, 1.25; P = 0.046).
Insulin
Twelve studies comprising 147 participants (79% males) measured insulin following comparator and glucagon administration [19,20,21, 23, 45, 47,48,49, 51, 52]. Of these 12 studies, eight used intravenous administration [20, 21, 23, 45, 48, 49, 51, 52], three used intramuscular administration [19, 49], and one used intranasal administration [47]. Average age of participants ranged from 21.0 to 48.5, with five studies being conducted in healthy-weight participants [19,20,21, 23, 51], three studies being conducted in overweight participants [45, 47, 48], and one study being conducted in obese participants [19]. Three studies did not report participant body weight characteristics [49, 52].
Mean intervention effect of glucagon administration relative to comparator on insulin was SMD = 1.33 (95% CI, 0.88–1.77; P < 0.001; Fig. 5). Measures of statistical heterogeneity were τ2 = 0.45 (95% CI, 0.13–1.56) and I2 = 83% (95% CI, 58–95%). According to the 95% PI, the effect size for acute glucagon administration relative to comparator on insulin is expected to range from –0.25 to 2.91 in future similar studies.
Results produced from a random-effects meta-analysis using the Hartung-Knapp-Sidik-Jonkman method to estimate between-study variance. Data are presented as mean with 95% confidence intervals. Mean-intervention effect (summary) is also presented alongside a 95% prediction interval (grey horizontal dotted line). Sample size (N), dose (duration of administration in minutes), and route of administration (colour of point estimates) for each study are provided. *duration of administration not reported. CI confidence interval, PI prediction interval, SMD standardised mean difference.
Mixed-effects meta-regression analyses with route of administration or total glucagon dose included as a moderator did not indicate that insulin response differed between administration routes or across total glucagon dose (Supplementary Appendix E).
Visual inspection of the contour-enhanced funnel plot showed asymmetry that indicated potential publication bias (Supplementary Appendix F). This is supported by the result of Egger’s regression test (P < 0.001). Trim and fill analysis estimated three missing studies on the left side of the funnel plot (Supplementary Appendix F), resulting in adjusted SMD of 1.07 (95% CI, 0.57, 1.58; P < 0.001).
Sensitivity analyses
Sensitivity analyses employing correlation coefficients of 0.3, 0.7 and 0.9 did not meaningfully alter the mean intervention effect and overall interpretation of glucagon administration on energy intake, energy expenditure, glucose, or insulin (Supplementary Appendix G).
Two studies were identified during the full-text screening phase that selected glucagon doses that were defined as sub-anorectic [45] or prevented hyperglycaemia [47]. Consequently, additional sensitivity analyses were performed for energy intake and glucose outcomes excluding these studies from meta-analytical procedures. However, exclusion of these studies did not meaningfully change the mean intervention effect and overall interpretation of results for either outcome (Supplementary Appendix H).
Leave-one-out meta-analyses for energy expenditure, glucose, and insulin did not identify any study that possessed sufficient influence, that when excluded, resulted in a different interpretation of the summary effect estimate (Supplementary Appendix I). The leave-one-out meta-analysis performed for energy intake did identify one study [23] that did exert a noticeable influence, in which its exclusion resulted in a confidence interval (and corresponding P-value) indicative of an anorectic effect (Supplementary Appendix I). However, due to the limited number of studies eligible for this meta-analysis, the importance of this finding is difficult to interpret.
Certainty of evidence
Certainty of evidence for energy intake, glucose and insulin was rated as low, whilst energy expenditure was rated as high. Explanation of judgements alongside certainty of evidence assessments are presented in the summary of findings table (Table 2).
Discussion
This review analysed the evidence on the effect of acute glucagon administration on energy intake, energy expenditure, subjective appetite, glucose, and insulin responses in humans. Meta-analyses revealed that, on average, acute glucagon administration increases energy expenditure, as well as glucose and insulin concentrations. However, the effect of acute glucagon administration on energy intake is unclear, whilst too few studies exist to permit a meta-analysis on subjective appetite.
The effect of acute glucagon administration on components of energy balance
The results from our analysis highlight that the effect of acute glucagon administration on energy intake in humans is inconclusive. Despite the point estimate for the mean intervention effect suggesting a small anorectic effect, the confidence interval for this effect was large and included both an increase and decrease in energy intake following acute glucagon administration. This uncertainty is also reflected in the effect sizes of the individual studies, the prediction interval for energy intake, and the reported effects of acute glucagon administration on subjective appetite. Indeed, no study performed a power calculation based on differences in energy intake between groups (with only two studies stating energy intake as a pre-registered primary outcome [20, 23]), likely contributing to the observed imprecision of the mean intervention effect. The small number of eligible studies also precluded mixed-effects meta-regression analysis from being performed, making it difficult to identify possible moderators responsible for the heterogeneity in responses.
It has been widely reported that glucagon administration can increase feelings of nausea [50, 52,53,54,55]. It is therefore possible that any observed effects in energy intake and appetite are secondary to a change in nausea, rather than a direct influence on any appetite-regulation system per se. Subsequently, any inconsistency in response may be related to the degree of nausea induced. However, all authors who assessed nausea reported that glucagon had no effect on the levels of nausea experienced [20, 23, 45], suggesting that nausea is not a likely explanation for the level of inconsistency observed.
Anorectic effects of chronic glucagon administration have, however, been previously reported [55, 56]; though a significant decrease in energy intake was only observed after multiple days of administration [55]. This suggests that either acute glucagon doses (<48 hours of continuous infusion) may not suppress energy intake, or that the suppression of energy intake following acute administration may be too small to be detected using the number of participants commonly recruited by studies investigating these effects (<20 participants; Table 1). Both explanations are nonetheless consistent with the findings of the present meta-analysis.
In contrast to its effect on energy intake, the mean intervention effect of acute glucagon administration on energy expenditure was a moderate-to-large increase, which was consistent across all included studies, and congruent with prior research in rodents [12, 57, 58]. Mechanisms responsible for this increase in energy expenditure may include futile substrate cycling, characterised by a repeated conversion between glucose and glucose-6-phosphate [59], but are unlikely related to changes in brown adipose tissue thermogenesis [21]. The absence of any corresponding increase in energy intake of a similar magnitude therefore suggests that acute glucagon administration would have a favourable effect on energy balance in the short-term.
Challenging the acute data on glucagon administration, recent evidence has suggested that chronic administration (72 hours) of glucagon may not raise energy expenditure [55]. This could explain why the smallest effect in our meta-analysis was observed in the study with the longest infusion duration (10 hours) [22], but also questions the efficacy of chronic glucagon administration and/or GCGR receptor agonism for weight loss via increased energy expenditure. Moreover, most studies (3/5 in this review) measuring energy expenditure following acute glucagon administration report pre-post measurements, preventing any investigation of temporal trends (and thus determining the time point at which energy expenditure is no longer raised). However, it remains to be fully elucidated whether the relative conservation of energy expenditure following weight loss would aid weight loss maintenance with a drug that had a glucagonergic element.
Visual inspection of changes in glucose and insulin over time following acute glucagon administration (Supplementary Appendix J) suggest the effect of glucagon on glucose homoeostasis is transient, with values returning to baseline within 200 min of administration. Importantly, insulin and glucose levels return to baseline despite glucagon levels remaining elevated via infusion, implying that acute supraphysiological doses of glucagon do not result in chronically elevated blood glucose concentrations. If it is assumed that the release of stored liver glycogen followed by endogenous insulin release (futile substrate cycling) is the primary driver of increased energy expenditure following acute glucagon administration, then a glucagonergic agent may not have therapeutic benefit as a long-acting preparation. However, if the energy-expenditure rise outlives the acute glucose raising effects (for example, due to effects on amino acid metabolism), then the absence of chronic hyperglycaemia with glucagon treatment is reassuring. Further research is needed to confirm if the increase in energy expenditure following acute glucagon administration is lost when administered chronically, to establish how energy expenditure changes over time following acute administration, and to firmly establish the mechanism by which glucagon acutely and chronically elevates energy expenditure in humans. Given glucagon’s effect on the catecholaminergic system [60], this research should also investigate possible negative effects of chronic glucagon administration such as changes in heart rate and blood pressure.
The effect of acute glucagon administration on glucose homoeostasis
The mean intervention effect of acute glucagon administration on both glucose and insulin concentrations was large. The effect on glucose concentrations is not surprising considering the well-established role of glucagon in upregulating hepatic glucose production via glycogenolysis [61]. Similarly, glucagon is known to stimulate insulin release both directly (via activation of beta-cells when glucose concentrations are high) and indirectly (via increased glucose concentrations) [62, 63]. Despite most studies reporting an increase in glucose and insulin following acute glucagon administration, the magnitude of this increase varied considerably between studies, resulting in a high degree of statistical heterogeneity that could not be explained by differences in administration route or glucagon dose in our analyses. It is important to note that the number of studies included in the mixed-effects meta-regression analyses (13 and 12 for glucose and insulin outcomes, respectively) was small. Therefore, when considering the small number of studies and large degree of statistical heterogeneity, a moderating effect of administration route or glucagon dose on glucose and insulin responses cannot be excluded as such analyses are likely inadequately powered to detect small to moderate effects [64].
Nevertheless, the consistent increase observed in both insulin and glucose concentrations across studies suggests that they are unlikely to play any potential role in mediating the effects of glucagon on appetite. It is also important to note that the state of hyperglycaemia induced by acute glucagon administration may increase cardiometabolic disease risk [65, 66]. It would therefore seem prudent that any glucagon-based anti-obesity approach is also capable of reducing glucose levels. This could be achieved by a glucagon-like peptide 1 (GLP-1) co-agonist, or a molecule with both GCGR and GLP-1 receptor activity [48].
Limitations
The present review is subject to several limitations. Firstly, several of the outcomes (energy intake, energy expenditure, and subjective appetite) were only measured by a small number of studies, reducing the precision of summary effect estimates and preventing the use of meta-regression analysis for exploring causes of heterogeneity (e.g. glucagon dose). Secondly, energy intake, glucose, and insulin outcomes showed considerable heterogeneity in response, which was not explained by administration route or total glucagon dose for glucose and insulin outcomes. Owing to the lack of studies to adequately detect moderator effects, it therefore remains unclear what moderates the response of these outcomes following acute glucagon administration. Thirdly, possible publication bias was detected for both glucose and insulin outcomes, suggesting that non-significant findings may have not been published, and that the effect estimates of the present review may be inflated. However, trim-and-fill analyses indicate that that inclusion of theoretical non-significant findings does not change the overall interpretation of the acute effect of glucagon on these outcomes. The possible presence of publication bias alongside large statistical heterogeneity for both glucose and insulin outcomes resulted in the evidence being graded as low certainty. It should be noted that this certainty relates to the precision of the effect estimate, not the direction, as the data clearly shows that acute glucagon administration increases both glucose and insulin concentrations. Fourthly, the participants of included studies were predominantly young (<35 years old) males, with less than half of eligible studies being conducted in participants with a BMI ≥ 25.0. The findings of the present analysis may therefore not be applicable to all populations, particularly those more likely to be treated with anti-obesity agents. Finally, the present analysis only focuses on acute effects of glucagon administration on energy balance and glucose homoeostasis, and thus any observed effects cannot be extrapolated to chronic administration.
Summary
Overall, acute administration of glucagon in humans appears to produce a marked rise in energy expenditure, glucose, and insulin. However, statistical heterogeneity and potential publication bias reduce our confidence in the effect size estimates for glucose and insulin responses. The effect of acute glucagon administration on energy intake and subjective appetite also remains unclear. Future work should look to clarify the effect of acute glucagon administration on energy intake and appetite, investigate any potential differences between acute and chronic administration, and if needed, develop protocols that can sustain acute beneficial effects such as increased expenditure over longer time periods.
Data availability
Data and R scripts used for analysis are available from the Open Science Framework at: https://osf.io/57xt9/ (https://doi.org/10.17605/OSF.IO/57XT9).
References
Berrington de Gonzalez A, Hartge P, Cerhan JR, Flint AJ, Hannan L, MacInnis RJ, et al. Body-mass index and mortality among 1.46 million white adults. N Engl J Med. 2010;363:2211–9.
Kivimäki M, Kuosma E, Ferrie JE, Luukkonen R, Nyberg ST, Alfredsson L, et al. Overweight, obesity, and risk of cardiometabolic multimorbidity: pooled analysis of individual-level data for 120 813 adults from 16 cohort studies from the USA and Europe. Lancet Public Heal. 2017;2:e277–e285.
Robison JI, Rogers MA. Adherence to exercise programmes. Sport Med. 1994;17:39–52.
Garrow JS, Summerbell CD. Meta-analysis: effect of exercise, with or without dieting, on the body composition of overweight subjects. Eur J Clin Nutr. 1995;49:1–10.
O’Brien PE, Hindle A, Brennan L, Skinner S, Burton P, Smith A, et al. Long-term outcomes after bariatric surgery: a systematic review and meta-analysis of weight loss at 10 or more years for all bariatric procedures and a single-centre review of 20-year outcomes after adjustable gastric banding. Obes Surg. 2019;29:3–14.
Müller TD, Finan B, Clemmensen C, DiMarchi RD, Tschöp MH. The new biology and pharmacology of glucagon. Physiol Rev. 2017;97:721–66.
Sandoval DA, D’Alessio DA. Physiology of proglucagon peptides: role of glucagon and GLP-1 in health and disease. Physiol Rev. 2015;95:513–48.
Holst JJ, Wewer Albrechtsen NJ, Pedersen J, Knop FKG. Glucagon and amino acids are linked in a mutual feedback cycle: the liver–α-cell axis. Diabetes. 2017;66:235–40.
Jones BJ, Tan T, Bloom SR. Minireview: glucagon in stress and energy homeostasis. Endocrinology. 2012;153:1049–54.
Marliss EB, Aoki TT, Unger RH, Soeldner JS, Cahill GF. Glucagon levels and metabolic effects in fasting man. J Clin Invest. 1970;49:2256–70.
Frampton J, Cobbold B, Nozdrin M, Oo HTH, Wilson H, Murphy KG, et al. The effect of a single bout of continuous aerobic exercise on glucose, insulin and glucagon concentrations compared to resting conditions in healthy adults: a systematic review, meta-analysis and meta-regression. Sport Med. 2021;51:1949–66.
Davidson IWF, Salter JM, Best CH. The effect of glucagon on the metabolic rate of rats. Am J Clin Nutr. 1960;8:540–6.
Geary N, Le Sauter J, Noh U. Glucagon acts in the liver to control spontaneous meal size in rats. Am J Physiol Integr Comp Physiol. 1993;264:R116–R122.
de Castro JM, Paullin SK, DeLugas GM. Insulin and glucagon as determinants of body weight set point and microregulation in rats. J Comp Physiol Psychol. 1978;92:571–9.
Inokuchi A, Oomura Y, Nishimura H. Effect of intracerebroventricularly infused glucagon on feeding behavior. Physiol Behav. 1984;33:397–400.
Billington CJ, Briggs JE, Link JG, Levine AS. Glucagon in physiological concentrations stimulates brown fat thermogenesis in vivo. Am J Physiol Integr Comp Physiol. 1991;261:R501–R507.
Habegger KM, Stemmer K, Cheng C, Muller TD, Heppner KM, Ottaway N, et al. Fibroblast growth factor 21 mediates specific glucagon actions. Diabetes. 2013;62:1453–63.
Filali-Zegzouti Y, Abdelmelek H, Rouanet JL, Cottet-Emard JM, Pequignot JM, Barr H. Role of catecholamines in glucagon-induced thermogenesis. J Neural Transm. 2005;112:481–9.
Arafat AM, Weickert MO, Adamidou A, Otto B, Perschel FH, Spranger J, et al. The impact of insulin-independent, glucagon-induced suppression of total ghrelin on satiety in obesity and type 1 diabetes mellitus. J Clin Endocrinol Metab. 2013;98:4133–42.
Bagger JI, Holst JJ, Hartmann B, Andersen B, Knop FK, Vilsbøll T. Effect of oxyntomodulin, glucagon, GLP-1, and combined glucagon +GLP-1 infusion on food intake, appetite, and resting energy expenditure. J Clin Endocrinol Metab. 2015;100:4541–52.
Salem V, Izzi‐Engbeaya C, Coello C, Thomas DB, Chambers ES, Comninos AN, et al. Glucagon increases energy expenditure independently of brown adipose tissue activation in humans. Diabetes, Obes Metab. 2016;18:72–81.
Chakravarthy M, Parsons S, Lassman ME, Butterfield K, Lee AYH, Chen Y, et al. Effects of 13-hour hyperglucagonemia on energy expenditure and hepatic glucose production in humans. Diabetes. 2017;66:36–44.
Izzi-Engbeaya C, Jones S, Crustna Y, Machenahalli PC, Papadopoulou D, Modi M, et al. Acute effects of glucagon on reproductive hormone secretion in healthy men. J Clin Endocrinol Metab. 2020;105:1899–905.
Genuth SM, Hoppel CL. Acute hormonal effects on carnitine metabolism in thin and obese subjects: responses to somatostatin, glucagon, and insulin. Metabolism. 1981;30:393–401.
Calles-Escandón J. Insulin dissociates hepatic glucose cycling and glucagon-induced thermogenesis in man. Metabolism. 1994;43:1000–5.
Samols E, Marri G, Marks V. Promotion of insulin secretion by glucagon. Lancet. 1965;286:415–6.
Crockford PM, Porte D, Wood FC, Williams RH. Effect of glucagon on serum insulin, plasma glucose and free fatty acids in man. Metabolism. 1966;15:114–22.
Arafat MA, Otto B, Rochlitz H, Tschöp M, Bähr V, Möhlig M, et al. Glucagon inhibits ghrelin secretion in humans. Eur J Endocrinol. 2005;153:397–402.
Loh K, Zhang L, Brandon A, Wang Q, Begg D, Qi Y, et al. Insulin controls food intake and energy balance via NPY neurons. Mol Metab. 2017;6:574–84.
Wyatt P, Berry SE, Finlayson G, O’Driscoll R, Hadjigeorgiou G, Drew DA, et al. Postprandial glycaemic dips predict appetite and energy intake in healthy individuals. Nat Metab. 2021;3:523–9.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71.
Borenstein M, Hedges LV, Higgins JPT, Rothstein HR. A basic introduction to fixed-effect and random-effects models for meta-analysis. Res Synth Methods. 2010;1:97–111.
Riley RD, Higgins JPT, Deeks JJ. Interpretation of random effects meta-analyses. BMJ. 2011;342:d549–d549.
Hartung J, Knapp G. On tests of the overall treatment effect in meta-analysis with normally distributed responses. Stat Med. 2001;20:1771–82.
Sidik K, Jonkman JN. A simple confidence interval for meta-analysis. Stat Med. 2002;21:3153–9.
Veroniki AA, Jackson D, Bender R, Kuss O, Langan D, Higgins JPT, et al. Methods to calculate uncertainty in the estimated overall effect size from a random‐effects meta‐analysis. Res Synth Methods. 2019;10:23–43.
Knapp G, Hartung J. Improved tests for a random effects meta-regression with a single covariate. Stat Med. 2003;22:2693–710.
Peters JL, Sutton AJ, Jones DR, Abrams KR, Rushton L. Contour-enhanced meta-analysis funnel plots help distinguish publication bias from other causes of asymmetry. J Clin Epidemiol. 2008;61:991–6.
Duval S, Tweedie R. A nonparametric “trim and fill” method of accounting for publication bias in meta-analysis. J Am Stat Assoc. 2000;95:89–98.
R Core Team. R: a language and environment for statistical computing. R Found. Stat Comput 2021. https://www.r-project.org/.
Viechtbauer W. Conducting meta-analyses in R with the metafor package. J Stat Softw. 2010;36:1–48.
Jackson D, Turner R. Power analysis for random-effects meta-analysis. Res Synth Methods. 2017;8:290–302.
Guyatt GH, Oxman AD, Vist GE, Kunz R, Falck-Ytter Y, Alonso-Coello P, et al. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ. 2008;336:924–6.
The GRADE Working Group. GRADE handbook for grading quality of evidence and strength of recommendations. 2013. https://gdt.gradepro.org/app/handbook/handbook.html.
Cegla J, Troke RC, Jones B, Tharakan G, Kenkre J, McCullough KA, et al. Coinfusion of low-dose GLP-1 and glucagon in man results in a reduction in food intake. Diabetes. 2014;63:3711–20.
Geary N, Kissileff HR, Pi-Sunyer FX, Hinton V. Individual, but not simultaneous, glucagon and cholecystokinin infusions inhibit feeding in men. Am J Physiol Integr Comp Physiol. 1992;262:R975–R980.
Stahel P, Lee SJ, Sud SK, Floh A, Dash S. Intranasal glucagon acutely increases energy expenditure without inducing hyperglycaemia in overweight/obese adults. Diabetes, Obes Metab. 2019;21:1357–64.
Tan TM, Field BCT, McCullough KA, Troke RC, Chambers ES, Salem V, et al. Coadministration of glucagon-like peptide-1 during glucagon infusion in humans results in increased energy expenditure and amelioration of hyperglycemia. Diabetes. 2013;62:1131–8.
Chernish SM, Maglinte DDT, Brunelle RL. The laboratory response to glucagon dosages used in gastrointestinal examinations. Invest Radiol. 1988;23:847–52.
Lockton JA, Poucher SM. Single dose glucagon (0.5 mg IV bolus) administration in healthy human volunteers is a robust model for assessment of glycogenolysis. J Pharmacol Toxicol Methods. 2007;55:86–90.
Ranganath L, Schaper F, Gama R, Morgan L, Wright J, Teale D, et al. Effect of glucagon on carbohydrate-mediated secretion of glucose-dependent insulinotropic polypeptide (GIP) and glucagon-like peptide-1 (7-36 amide) (GLP-1). Diabetes Metab Res Rev. 1999;15:390–4.
Schjoldager B, Lawaetz O, Christiansen J. Effect of pancreatic glucagon and its 1-21 fragment on gastric emptying in man. Scand J Gastroenterol. 1988;23:726–30.
Larsen S, Osnes M, Christensen MS. The effect of glucagon, glucagon-(l-21)-peptide, and placebo on duodenal pressure activity in healthy subjects. Scand J Gastroenterol. 1986;21:634–40.
Arvat E, Maccagno B, Ramunni J, Giordano R, DiVito L, Broglio F, et al. Glucagon is an ACTH secretagogue as effective as hCRH after intramuscolar administration while it is ineffective when given intravenously in normal subjects. Pituitary. 2000;3:169–73.
Whytock KL, Carnero EA, Vega RB, Tillner J, Bock C, Chivukula K, et al. Prolonged glucagon infusion does not affect energy expenditure in individuals with overweight/obesity: a randomized trial. Obesity. 2021;29:1003–13.
Schulman JL, Carleton JL, Whitney G, Whitehorn JC. Effect of glucagon on food intake and body weight in man. J Appl Physiol. 1957;11:419–21.
Davidson IWF, Salter JM, Best CH. Calorigenic action of glucagon. Nature. 1957;180:1124–1124.
Doi K, Kuroshima A. Thermogenic response to glucagon in cold-acclimated mice. Jpn J Physiol. 1982;32:377–85.
Miyoshi H, Shulman GI, Peters EJ, Wolfe MH, Elahi D, Wolfe RR. Hormonal control of substrate cycling in humans. J Clin Invest. 1988;81:1545–55.
Siqueira-Filho AG, Sheps SG, Maher FT, Jiang NS, Elveback LR. Glucagon-blood catecholamine test: use in isolated and familial pheochromocytoma. Arch Intern Med. 1975;135:1227–31.
Ramnanan CJ, Edgerton DS, Kraft G, Cherrington AD. Physiologic action of glucagon on liver glucose metabolism. Diabetes, Obes Metab. 2011;13:118–25.
Huypens P, Ling Z, Pipeleers D, Schuit F. Glucagon receptors on human islet cells contribute to glucose competence of insulin release. Diabetologia. 2000;43:1012–9.
Song G, Pacini G, Ahrén B, D’Argenio DZ. Glucagon increases insulin levels by stimulating insulin secretion without effect on insulin clearance in mice. Peptides. 2017;88:74–79.
Hempel S, Miles JNV, Booth MJ, Wang Z, Morton SC, Shekelle PG. Risk of bias: a simulation study of power to detect study-level moderator effects in meta-analysis. Syst Rev. 2013;2:107.
Pyörälä M, Miettinen H, Laakso M, Pyörälä K. Hyperinsulinemia predicts coronary heart disease risk in healthy middle-aged men. Circulation. 1998;98:398–404.
Lu J, He J, Li M, Tang X, Hu R, Shi L, et al. Predictive value of fasting glucose, postload glucose, and hemoglobin A 1c on risk of diabetes and complications in Chinese adults. Diabetes Care. 2019;42:1539–48.
Acknowledgements
We would like to thank contacted authors for taking the time to respond to data requests in such a kind and prompt manner.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors. The Section of Endocrinology and Investigative Medicine is funded by grants from the MRC, BBSRC and NIHR, and is supported by the NIHR Biomedical Research Centre Funding Scheme. JF is funded by the Imperial College London President’s PhD Scholarship.
Author information
Authors and Affiliations
Contributions
JF and ESC conceived and designed the study. JF performed databases searches. JF and ESC participated in the screening process. JF extracted data and performed all statistical analyses. JF, CI, VS, KGM, TMT and ESC interpreted results of the analysis. JF wrote the initial draft of the manuscript, and critically revised by CI, VS, KGM, TMT and ESC. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Frampton, J., Izzi-Engbeaya, C., Salem, V. et al. The acute effect of glucagon on components of energy balance and glucose homoeostasis in adults without diabetes: a systematic review and meta-analysis. Int J Obes 46, 1948–1959 (2022). https://doi.org/10.1038/s41366-022-01223-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41366-022-01223-y