Abstract
Background/objective
There is evidence that metabolic profile changes after Roux-Y gastric bypass (RYGB), especially due to modifications in the gastrointestinal tract. In addition, previous studies have suggested that probiotics can modify the microbiome and produce metabolites important for metabolic health maintenance. In this sense, the aim of this study was to verify the influence of probiotic supplementation on the plasma metabolite profile after RYGB.
Methods
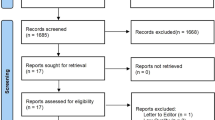
This was a randomized, double-blind, placebo-controlled clinical trial conducted with 31 patients subjected to RYGB surgery, randomized in probiotic group that was supplemented with a probiotic supplement (FloraVantage®) for 3 months after surgery or a placebo group. Plasma metabonomics was performed using nuclear magnetic resonance (NMR) at the preoperative period (T0) and at 45–50 days (T1) and 90–95 days (T2) during the postoperative period/intervention.
Results
Reductions in trimethylamine-N-oxide (TMAO) and alanine were observed in both groups, however this reduction was greater in the probiotic group (TMAO 13.82%, p = 0.01 and alanine 14.03%, p = 0.03) at T2. Additionally, β-hydroxybutyrate (BHB) levels increased 10.77% in the probiotic group (p = 0.03) compared to the placebo group at T2.
Conclusion
Supplementation with Lactobacillus acidophilus NCFM and Bifidobacterium lactis Bi-07 was able to associate with significant differences in relevant plasma metabolites associated with improved metabolic health.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
Data availability
Requests for further information should be directed to the corresponding author.
References
Wang FG, Yan WM, Yan M, Song MM. Outcomes of Mini vs Roux-en-Y gastric bypass: a meta-analysis and systematic review. Int J Surg. 2018;56:7–14.
Buchwald H, Avidor Y, Braunwald E, Jensen MD, Pories W, Fahrbach K, et al. Bariatric surgery: a systematic review and meta-analysis. Jama. 2004;292:1724–37.
Lager CJ, Esfandiari NH, Luo Y, Subauste AR, Kraftson AT, Brown MB, et al. Metabolic parameters, weight loss, and comorbidities 4 years after Roux-en-Y gastric bypass and sleeve gastrectomy. Obes Surg. 2018;28:3415–23.
Adams TD, Davidson LE, Litwin SE, Kim J, Kolotkin RL, Nanjee MN, et al. Weight and metabolic outcomes 12 years after gastric bypass. N Engl J Med. 2017;377:1143–55.
Li JV, Ashrafian H, Bueter M, Kinross J, Sands C, le Roux CW, et al. Metabolic surgery profoundly influences gut microbial–host metabolic cross-talk. Gut. 2011;60:1214–23.
Al Assal K, Prifti E, Belda E, Sala P, Clément K, Dao MC, et al. Gut microbiota profile of obese diabetic women submitted to Roux-en-Y gastric bypass and its association with food intake and postoperative diabetes remission. Nutrients. 2020;12:278.
Pajecki D, de Oliveira LC, Sabino EC, de Souza-Basqueira M, Dantas AC, Nunes GC, et al. Changes in the intestinal microbiota of superobese patients after bariatric surgery. Clinics (Sao Paulo). 2019;74:e1198.
Kong LC, Tap J, Aron-Wisnewsky J, Pelloux V, Basdevant A, Bouillot JL, et al. Gut microbiota after gastric bypass in human obesity: increased richness and associations of bacterial genera with adipose tissue genes. Am J Clin Nutr. 2013;98:16–24.
Ilhan ZE, DiBaise JK, Isern NG, Hoyt DW, Marcus AK, Kang DW, et al. Distinctive microbiomes and metabolites linked with weight loss after gastric bypass, but not gastric banding. ISME J. 2017;11:2047–58.
Samczuk P, Ciborowski M, Kretowski A. Application of metabolomics to study effects of bariatric surgery. J Diabetes Res. 2018;2018:6270875.
Lee ES, Song EJ, Nam YD, Lee SY. Probiotics in human health and disease: from nutribiotics to pharmabiotics. J Microbiol. 2018;56:773–82.
Vandenplas Y, Huys G, Daube G. Probiotics: An update. J Pediatr (Rio J). 2015;91:06–21.
Chung HJ, Sim JH, Min TS, Choi HK. Metabolomics and lipidomics approaches in the science of probiotics: a review. J Med Food. 2018;21:1086–95.
Seridi L, Leo GC, Dohm GL, Pories WJ, Lenhard J. Time course metabolome of Roux-en-Y gastric bypass confirms correlation between leptin, body weight and the microbiome. PLoS One. 2018;13:e0198156.
Jarak I, Pereira SS, Carvalho RA, Oliveira PF, Alves MG, Guimarães M, et al. Gastric bypass with different biliopancreatic limb lengths results in similar post-absorptive metabolomics profiles. Obes Surg. 2020;30:1068–78.
Herzog K, Berggren J, Al Majdoub M, Balderas AC, Lindqvist A, Hedenbro J, et al. Metabolic effects of gastric bypass surgery: is it all about calories? Diabetes. 2020;69:2027–35.
Dreyfuss JM, Yuchi Y, Dong X, Efthymiou V, Pan H, Simonson DC, et al. High-throughput mediation analysis of human proteome and metabolome identifies mediators of post-bariatric surgical diabetes control. Nat Commun. 2021;12:6951.
Jones B, Sands C, Alexiadou K, Minnion J, Tharakan G, Behary P, et al. The metabolomic effects of tripeptide gut hormone infusion compared to Roux-en-Y gastric bypass and caloric restriction. J Clin Endocrinol Metab. 2022;107:e767–e782.
Greenstein R. Reporting weight loss. Obes Surg. 2007;17:1275.
Beckonert O, Keun HC, Ebbels TM, Bundy J, Holmes E, Lindon JC, et al. Metabolic profiling, metabolomic and metabonomic procedures for NMR spectroscopy of urine, plasma, serum and tissue extracts. Nat Protoc. 2007;2:2692–703.
Foxall PJ, Spraul M, Farrant RD, Lindon LC, Neild GH, Nicholson JK. 750 MHz 1H-NMR spectroscopy of human blood plasma. J Pharm Biomed Anal. 1993;11:267–76.
Bell JD, Brown JC, Nicholson JK, Sadler PJ. Assignment of resonances for ‘acute-phase’ glycoproteins in high resolution proton NMR spectra of human blood plasma. FEBS Lett. 1987;215:311–5.
Fan TW. Metabolite profiling by one-and two-dimensional NMR analysis of complex mixtures. Progress in nuclear magnetic resonance spectroscopy. 1996;28:161–219.
R Core Team. R: A language and environment for statistical computing. Vienna: R Foundation for Statistical Computing. Available from: http://www.r-project.org/index.html
Savorani F, Tomasi G, Engelsen SB. icoshift: A versatile tool for the rapid alignment of 1D NMR spectra. J Magn Reson. 2010;202:190–202.
Andersson CA, Bro R. The N-way toolbox for MATLAB. Chemometrics Intelligent Lab Syst. 2000;52:1–4.
Furet JP, Kong LC, Tap J, Poitou C, Basdevant A, Bouillot JL, et al. Differential adaptation of human gut microbiota to bariatric surgery–induced weight loss: links with metabolic and low-grade inflammation markers. Diabetes. 2010;59:3049–57.
Murphy R, Tsai P, Jüllig M, Liu A, Plank L, Booth M. Differential changes in gut microbiota after gastric bypass and sleeve gastrectomy bariatric surgery vary according to diabetes remission. Obes Surg. 2017;27:917–25.
Ramos MRZ, de Oliveira Carlos L, Wagner NRF, Felicidade I, da Cruz MR, Taconeli CA, et al. Effects of Lactobacillus acidophilus NCFM and Bifidobacterium lactis Bi-07 supplementation on nutritional and metabolic parameters in the early postoperative period after Roux-en-Y Gastric Bypass: a randomized, double-blind, placebo-controlled trial. Obes Surg. 2021;31:2105–14.
Wagner NRF, Ramos MRZ, de Oliveira Carlos L, da Cruz MRR, Taconeli CA, Filho AJB, et al. Effects of probiotics supplementation on gastrointestinal symptoms and SIBO after Roux-en-Y Gastric Bypass: a prospective, randomized, double-blind, placebo-controlled trial. Obes Surg. 2021;31:143–50.
Carlos LO, Ramos MRZ, Wagner NRF, Freitas LAC, Felicidade I, Campos ACL. Probiotic supplementation attenuates binge eating and food addiction 1 year after Roux-en-Y Gastric Bypass: a randomized, double-blind, placebo-controlled trial. Arq Bras Cir Dig. 2022;35:e1659.
Cornejo-Pareja I, Clemente-Postigo M, Tinahones FJ. Metabolic and endocrine consequences of bariatric surgery. Front Endocrinol (Lausanne). 2019;10:626.
Clemente-Postigo M, del Mar Roca-Rodriguez M, Camargo A, Ocaña-Wilhelmi L, Cardona F, Tinahones FJ. Lipopolysaccharide and lipopolysaccharide-binding protein levels and their relationship to early metabolic improvement after bariatric surgery. Surg Obes Relat Dis. 2015;11:933–9.
Ashrafian H, le Roux CW. Metabolic surgery and gut hormones–a review of bariatric entero-humoral modulation. Physiol Behav. 2009;97:620–31.
Haluzík M, Kratochvílová H, Haluzíková D, Mráz M. Gut as an emerging organ for the treatment of diabetes: focus on mechanism of action of bariatric and endoscopic interventions. J Endocrinol. 2018;237:R1–R17.
Lips MA, Van Klinken JB, van Harmelen V, Dharuri HK, AC’t Hoen P, Laros JF, et al. Roux-en-Y gastric bypass surgery, but not calorie restriction, reduces plasma branched-chain amino acids in obese women independent of weight loss or the presence of type 2 diabetes. Diabetes care. 2014;37:3150–6.
Dharuri H, AC’t Hoen P, van Klinken JB, Henneman P, Laros JF, Lips MA, et al. Downregulation of the acetyl-CoA metabolic network in adipose tissue of obese diabetic individuals and recovery after weight loss. Diabetologia. 2014;57:2384–92.
Lopes TI, Geloneze B, Pareja JC, Calixto AR, Ferreira MM, Marsaioli AJ. Blood metabolome changes before and after bariatric surgery: A 1H NMR-based clinical investigation. OMICS. 2015;19:318–27.
Wijayatunga NN, Sams VG, Dawson JA, Mancini ML, Mancini GJ, Moustaid‐Moussa N. Roux‐en‐Y gastric bypass surgery alters serum metabolites and fatty acids in patients with morbid obesity. Diabetes Metab Res Rev. 2018;34:e3045.
She P, Van Horn C, Reid T, Hutson SM, Cooney RN, Lynch CJ. Obesity-related elevations in plasma leucine are associated with alterations in enzymes involved in branched-chain amino acid metabolism. Am J Physiol Endocrinol Metab. 2007;293:E1552–63.
Juraschek SP, Shantha GP, Chu AY, Miller ER III, Guallar E, Hoogeveen RC, et al. Lactate and risk of incident diabetes in a case-cohort of the atherosclerosis risk in communities (ARIC) study. PloS One. 2013;8:e55113.
Chen YD, Varasteh BB, Reaven GM. Plasma lactate concentration in obesity and type 2 diabetes. Diabete Metab. 1993;19:348–54.
Berggren JR, Boyle KE, Chapman WH, Houmard JA. Skeletal muscle lipid oxidation and obesity: influence of weight loss and exercise. Am J Physiol Endocrinol Metab. 2008;294:E726–32.
Jones TE, Pories WJ, Houmard JA, Tanner CJ, Zheng D, Zou K, et al. Plasma lactate as a marker of metabolic health: Implications of elevated lactate for impairment of aerobic metabolism in the metabolic syndrome. Surgery. 2019;166:861–6.
Houmard JA, Pories WJ, Dohm GL. Is there a metabolic program in the skeletal muscle of obese individuals? J Obes. 2011;2011:250496.
Fernández M, Zúñiga M. Amino acid catabolic pathways of lactic acid bacteria. Crit Rev Microbiol. 2006;32:155–83.
Vieco-Saiz N, Belguesmia Y, Raspoet R, Auclair E, Gancel F, Kempf I, et al. Benefits and inputs from lactic acid bacteria and their bacteriocins as alternatives to antibiotic growth promoters during food-animal production. Front Microbiol. 2019;10:57.
Patrone V, Vajana E, Minuti A, Callegari ML, Federico A, Loguercio C, et al. Postoperative changes in fecal bacterial communities and fermentation products in obese patients undergoing bilio-intestinal bypass. Front Microbiol. 2016;7:200.
Brinkworth GD, Noakes M, Clifton PM, Bird AR. Comparative effects of very low-carbohydrate, high-fat and high-carbohydrate, low-fat weight-loss diets on bowel habit and faecal short-chain fatty acids and bacterial populations. Br J Nutr. 2009;101:1493–502.
Wang L, Zhang J, Guo Z, Kwok L, Ma C, Zhang W, et al. Effect of oral consumption of probiotic Lactobacillus planatarum P-8 on fecal microbiota, SIgA, SCFAs, and TBAs of adults of different ages. Nutrition. 2014;30:776–83.
Pérez-Burillo S, Pastoriza S, Gironés A, Avellaneda A, Francino MP, Rufián-Henares JA. Potential probiotic salami with dietary fiber modulates metabolism and gut microbiota in a human intervention study. J Functional Foods. 2020;66:103790.
Frost G, Sleeth ML, Sahuri-Arisoylu M, Lizarbe B, Cerdan S, Brody L, et al. The short-chain fatty acid acetate reduces appetite via a central homeostatic mechanism. Nat Commun. 2014;5:3611.
Dehghan P, Farhangi MA, Nikniaz L, Nikniaz Z, Asghari‐Jafarabadi M. Gut microbiota‐derived metabolite trimethylamine N‐oxide (TMAO) potentially increases the risk of obesity in adults: an exploratory systematic review and dose‐response meta‐analysis. Obes Rev. 2020;21:e12993.
Gruppen EG, Garcia E, Connelly MA, Jeyarajah EJ, Otvos JD, Bakker SJ, et al. TMAO is associated with mortality: impact of modestly impaired renal function. Sci Rep. 2017;7:13781.
Haghikia A, Li XS, Liman TG, Bledau N, Schmidt D, Zimmermann F, et al. Gut microbiota–dependent trimethylamine N-oxide predicts risk of cardiovascular events in patients with stroke and is related to proinflammatory monocytes. Arterioscler Thromb Vasc Biol. 2018;38:2225–35.
Senthong V, Wang Z, Fan Y, Wu Y, Hazen SL, Tang WW. Trimethylamine N‐oxide and mortality risk in patients with peripheral artery disease. J Am Heart Assoc. 2016;5:e004237.
Din AU, Hassan A, Zhu Y, Yin T, Gregersen H, Wang G. Amelioration of TMAO through probiotics and its potential role in atherosclerosis. Appl Microbiol Biotechnol. 2019;103:9217–28.
Kalani M, Hodjati H, Khanian MS, Doroudchi M. Lactobacillus acidophilus increases the anti-apoptotic micro RNA-21 and decreases the pro-inflammatory micro RNA-155 in the LPS-treated human endothelial cells. Probiotics Antimicrob Proteins. 2016;8:61–72.
Jensen MD, Haymond MW, Rizza RA, Cryer PE, Miles J. Influence of body fat distribution on free fatty acid metabolism in obesity. J Clin Invest. 1989;83:1168–73.
Boden G. Obesity and free fatty acids. Endocrinol Metab Clin North Am. 2008;37:635–46.
Boden G, Shulman GI. Free fatty acids in obesity and type 2 diabetes: defining their role in the development of insulin resistance and beta‐cell dysfunction. Eur J Clin Invest. 2002;32:14–23.
Kullberg J, Sundbom M, Haenni A, Freden S, Johansson L, Börnert P, et al. Gastric bypass promotes more lipid mobilization than a similar weight loss induced by low-calorie diet. J Obes. 2011;2011:959601.
Jacobsen SH, Bojsen-Møller KN, Dirksen C, Jørgensen NB, Clausen TR, Wulff BS, et al. Effects of gastric bypass surgery on glucose absorption and metabolism during a mixed meal in glucose-tolerant individuals. Diabetologia. 2013;56:2250–4.
Klein S, Mittendorfer B, Eagon JC, Patterson B, Grant L, Feirt N, et al. Gastric bypass surgery improves metabolic and hepatic abnormalities associated with nonalcoholic fatty liver disease. Gastroenterology. 2006;130:1564–72.
Hansen M, Lund MT, Gregers E, Kraunsøe R, Van Hall G, Helge JW, et al. Adipose tissue mitochondrial respiration and lipolysis before and after a weight loss by diet and RYGB. Obesity (Silver Spring). 2015;23:2022–9.
Randle PJ, Garland PB, Hales CN, Newsholme EA. The glucose fatty-acid cycle its role in insulin sensitivity and the metabolic disturbances of diabetes mellitus. The Lancet. 1963;281:785–9.
Lopes TI, Geloneze B, Pareja JC, Calixto AR, Ferreira MM, Marsaioli AJ. “Omics” prospective monitoring of bariatric surgery: Roux-en-Y gastric bypass outcomes using mixed-meal tolerance test and time-resolved 1H NMR-based metabolomics. OMICS. 2016;20:415–23.
Kim YA, Keogh JB, Clifton PM. Probiotics, prebiotics, synbiotics and insulin sensitivity. Nutr Res Rev. 2018;31:35–51.
Funding
This research received financial support from the CAPES (Coordination for the Improvement of Higher Education Personnel). CAPES had no influence on the writing, submission, or any other part of research formulation.
Author information
Authors and Affiliations
Contributions
MRZR, LCO, NRFW, IF, MRRC, and ACLC contributed to the conception and design of the study. MRZR, LCO, NRFW were responsible for data collect. MRZR, IF, FCHB, TIBL, MSM, LRR, JVZ, FCMJ, and ACLC were responsible for the analysis, and/or interpretation and discussion of the data. LVAL was responsible for the graphical abstract. MRZR and FCHB submitted the manuscript. All authors have read and agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare that they have no conflict of interest. The probiotics were donated by Bariatric Advantage (Aliso Viejo, California, United States) and placebo and glucose by Dermatologica Pharmacy (Curitiba, Paraná, Brazil). The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript, or in the decision to publish the results.
Ethics approval
The study was conducted according to the guidelines of the Declaration of Helsinki and approved by the Research Ethics Committee of the Pontifical Catholic University of Paraná (PUCPR) (n° 4.252.808) and was registered in the Brazilian Clinical Trials Registry - REBEC (n°RBR-4x3gqp)
Informed consent
Informed consent was obtained from all subjects involved in the study.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ramos, M.R.Z., Felicidade, I., de Oliveira Carlos, L. et al. Effect of probiotic supplementation on plasma metabolite profile after Roux-Y gastric bypass: a prospective, randomized, double-blind, placebo-controlled clinical trial. Int J Obes 46, 2006–2012 (2022). https://doi.org/10.1038/s41366-022-01213-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41366-022-01213-0
This article is cited by
-
Effects of probiotics in patients with morbid obesity undergoing bariatric surgery: a systematic review and meta-analysis
International Journal of Obesity (2023)
-
Brazilian guide to nutrition in bariatric and metabolic surgery
Langenbeck's Archives of Surgery (2023)